Fig. 3.1
Assessing scapular dyskinesis. The subject performs 3–5 repetitions in each of scaption (pictured) and flexion
The diagnostic value of observation has only been reported in reference to the shrug sign [5], an elevation of the entire shoulder girdle while attempting elevation of the arm (Fig. 3.2). When the shrug sign is negative, glenohumeral osteoarthritis, adhesive capsulitis, and severe rotator cuff tendinopathy can be ruled out as diagnoses with relative certainty.


Fig. 3.2
Shrug sign. The patient demonstrates the shrug sign in the right shoulder
3.4 Screening
The objective of an effective screen is to raise suspicions of and help rule out non-musculoskeletal sources of pain and also to help focus the physical examination in situations where symptoms encompass more than one joint. The standard screening examination that is inclusive of the shoulder and elbow is the upper quarter screen. The screen combines active motions of the cervical spine and combined motions of the shoulder and elbow (Fig. 3.3a, b) with upper motor neuron testing and testing of dermatomes, myotomes, and reflexes (Table 3.1). Overpressure can be applied by the examiner to further stress the active motions. A more detailed examination can include 2-point discrimination, testing of vibration sense, and vascular testing.
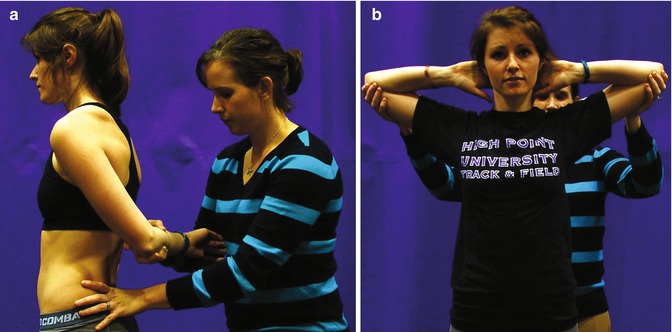
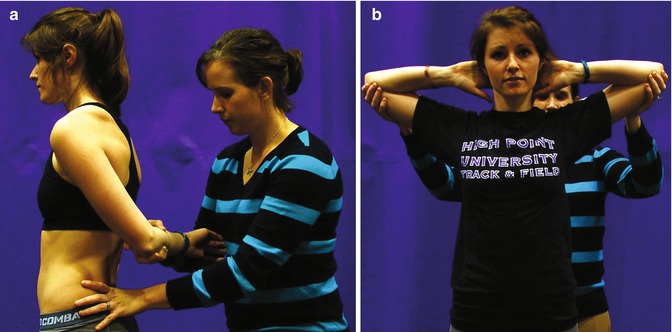
Fig. 3.3
(a) Combined motions of the shoulder and elbow with overpressure. Shoulder extension, adduction, and internal rotation. (b) Combined motions of the shoulder and elbow with overpressure. Shoulder abduction and external rotation with elbow flexion
Table 3.1
Dermatomes, myotomes, and reflexes of the upper quarter screen
C1–3 | C4 | C5 | C6 | C7 | C8 | T1 | |
|---|---|---|---|---|---|---|---|
Dermatome | Side of face | Suprascapular region | Deltoid region | Thumb and pointer finger | Middle finger | Ulnar border of hand | Medial border of upper arm |
Myotomes | Cervical rotation | Shoulder shrug | Shoulder abduction | Elbow flexion, wrist extension | Elbow extension | Thumb extension | Finger abduction |
Reflexes | None | None | Biceps, brachioradialis | Biceps, brachioradialis | Triceps | Triceps | None |
Reproduction of the concordant sign during active and combined motions indicates that a more thorough examination (see following sections of this chapter) of the offending joint should be performed.
Combined testing of dermatomes, myotomes, and reflexes, especially with findings of decreased sensation, weakness, and hyporeflexia when compared to the opposite arm, should alert the examiner to the likely presence of cervical radiculopathy.
Testing for an upper motor neuron lesion (spinal cord or brain) in the upper quarter screen is best done with Hoffman’s test, which is performed by flexing or flicking the distal phalanx of the middle finger. A positive test is indicated by flexion of the thumb or the distal phalanxes of the other fingers (clawing).
3.5 Motion Testing
3.5.1 Active Motion
Active motions at the shoulder typically performed are flexion, extension, abduction, horizontal adduction, internal rotation, and external rotation. Internal rotation and external rotation are often repeated with the arm in 90° of abduction to more closely mimic the position of the arm during throwing. Active elbow motions include flexion, extension, forearm pronation, and forearm supination. In the presence of trauma, the inability of the patient to fully flex, fully extend, fully pronate, or fully supinate is a highly specific sign for fracture [6]. Whether testing the shoulder, elbow, or both, active motion is performed in comparison to the other arm, and reproduction of the concordant sign is an important finding.
3.5.2 Passive Testing
Passive motions performed at the elbow are the same as active and for the same reasons: to note limitations and excesses (instability) and to look for the concordant sign. A global loss of shoulder motion is highly indicative of adhesive capsulitis [7]. Passive motions at the shoulder are also the same as active with the exception that most clinicians perform isolated glenohumeral flexion, abduction, and internal and external rotation at 90° abduction. The reason that glenohumeral motions are isolated is that gross movements at the shoulder are accomplished with contribution of other joints like the acromioclavicular and sternoclavicular joints as well as adjacent areas of the body like the scapulothoracic pseudo-joint and the thoracic spine. Isolating the glenohumeral joint (Fig. 3.4a, b) gives a better comparison of limitation at the shoulder and is likely to produce the concordant sign in glenohumeral pathology. A specific example can be found in isolated abduction, called the hyperabduction test [8], which can be used to detect inferior laxity or instability (Fig. 3.5). Another example is that many throwing athletes display excessive isolated glenohumeral external rotation with an accompanying loss of isolated glenohumeral internal rotation.
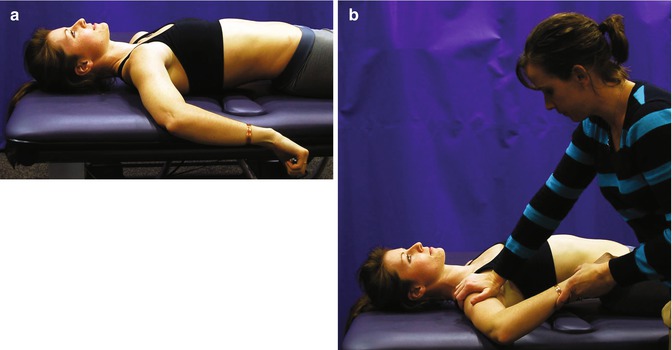

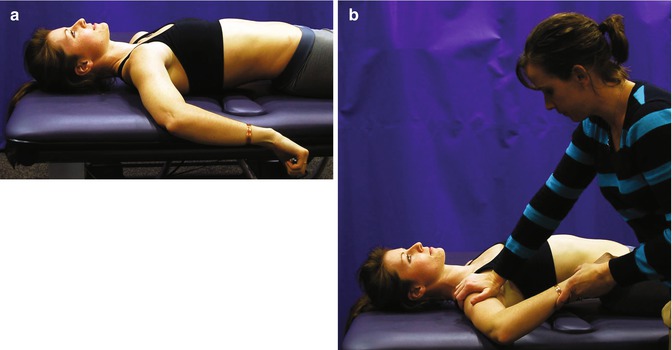
Fig. 3.4
(a) Gross internal rotation of the shoulder. Accomplished with anterior tipping of the scapula. (b) Isolated glenohumeral motion. Internal rotation is far less when anterior tipping of the scapula is controlled

Fig. 3.5
The hyperabduction test. Greater than 105° of isolated glenohumeral abduction is indicative of inferior laxity
3.5.3 Accessory Motion
The final motions tested are accessory motions, which can be defined as the gliding of one joint surface on another. Sometimes referred to as stability testing, accessory motions are labeled by the direction in which the moving side of the joint is pushed or pulled. For example, a posterior-to-anterior accessory motion of the glenohumeral joint would indicate that the humeral head was mobilized in an anterior direction in reference to the glenoid fossa. Excessive motion with this accessory test, especially when accompanied by patient apprehension, would lead the clinician to suspect anterior instability. Other examples of accessory motion findings and the interpretation of those findings can be found in Table 3.2. In addition to limitations or excessive motion during testing, the clinician also should take note of reproduction of the concordant sign.
Table 3.2
Examples of accessory motions and interpretation of findings
Accessory motion and finding | Interpretation of finding |
|---|---|
Glenohumeral anterior to posterior → limited | Tight posterior capsule—often present in patients with impingement pain |
Glenohumeral superior to inferior (with arm at side) → excessive or painful | Inferior laxity or instability—injury to the superior labrum, biceps, or coracohumeral ligament |
Glenohumeral superior to inferior (with arm at 90° abduction) → excessive or painful | Inferior laxity or instability—injury to the inferior capsuloligamentous structure |
Radiohumeral lateral glide → excessive or painful | Radial head laxity or instability—disruption of the annular ligament or fracture of the proximal radius |
3.6 Palpation
Palpation is performed next in the systematic examination and the process of palpation should be very directed based on the results of history, observation, screening, and motion testing. While many clinicians palpate in an effort to detect side-to-side differences in bony and soft tissue architecture, there is no research at present to support the value of this approach at either the shoulder or elbow. However, there is value in palpation of the long head of the biceps (tendinopathy) [9], the supraspinatus (tendinopathy) [9], and the acromioclavicular (AC) joint (AC pathology) [10]. Palpation of these structures is a sensitive test and therefore, an absence of pain when palpating contributes to ruling out the associated pathologies.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








