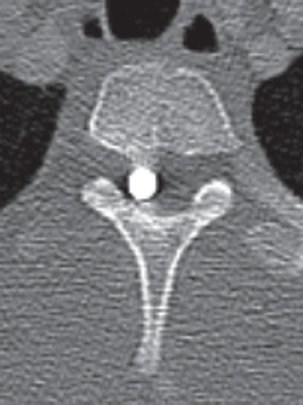
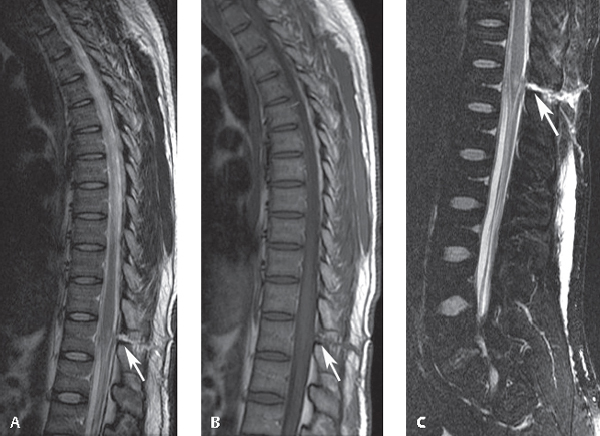
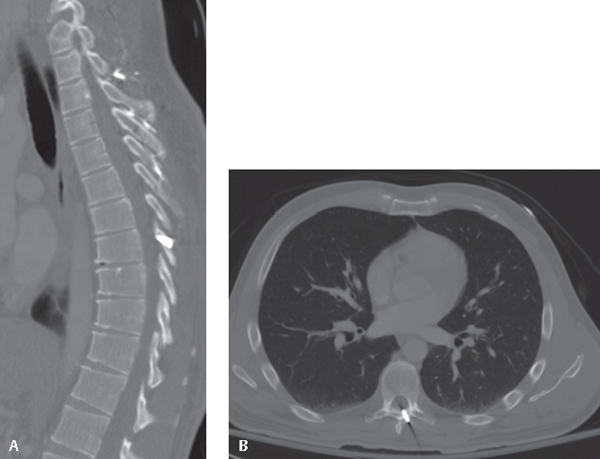
72 In a cohort of more than 24,000 patients studied by the National Spinal Cord Injury Statistical Center, violence was found to be the third most common cause of spinal cord injury (SCI) and was responsible for 18.2% of admissions.1 Gunshot wounds (GSWs) and knife injuries account for most violence-related SCIs. Accidents and work-related impalement injuries of the spine are relatively uncommon and constitute the remaining penetrating injuries of the spine seen in practice.2 To our knowledge, no formal classification scheme for penetrating SCI exists. It is convenient, however, to divide penetrating SCI treatment into two broad categories based on the mechanism of injury: impaling/stabbing injuries and ballistic injuries. Acute penetrating SCI not only affects the spinal cord; it also puts many neighboring vital structures at risk for injury. Therefore, it is important to follow Advanced Trauma Life Support protocols3 and involve general surgery trauma specialists and emergency department physicians as appropriate. Once the patient is appropriately stabilized, initial evaluation of penetrating SCI involves the same detailed history and physical examination as that of patients with other suspected spine injuries. For penetrating injuries, information regarding the penetrating object helps guide appropriate management. Recovery of the actual object provides the most useful information; otherwise, a careful history, including a general description of the weapon or object, is helpful. It is also important to determine whether any neurologic symptoms occurred immediately after the injury and to document the progression, or lack thereof, of any of these symptoms. In addition to comprehensive neurologic and spine examinations, a thorough inspection of all entrance and exit wounds should be performed. Palpation of the tissue for the presence of crepitus and general turgor is important for gauging the extent of underlying tissue necrosis.4 If an object remains impaled in the wound, it is important that it not be removed in the emergency department, particularly if a viscus has been perforated. Withdrawing an impaling object without appropriate surgical irrigation and débridement can result in bowel content contamination of surrounding tissues and eventual sepsis.5 Standard radiographic views of the involved spinal region should always be obtained, even in the absence of neurologic deficits. Klein and colleagues6 retrospectively analyzed 244 patients with substantial spinal injuries secondary to GSWs and found that 13% presented with no neurologic symptoms. They concluded that complete radiographic spine evaluation was mandatory after a GSW to the face, neck, or trunk, even without neurologic deficit.6 Spine fractures should be characterized by type and classified morphologically or through the use of one of the commonly accepted fracture classification systems, such as the subaxial injury classification score (SLIC) or the Thoracolumbar Injury Classification and Severity Score (TLICS). Imaging modalities are chosen to visualize various aspects of the injury, including the location of foreign debris, extent of osseous involvement, and soft-tissue integrity. Radiographs should be scrutinized for residual fragments and/or foreign debris from the impaling object/projectile. Approximately one-third of the neurologic deficits secondary to GSWs are associated with retained bullet fragments in the spinal canal.7 Computed tomography can help determine the extent of spine injury and evaluate the degree of spinal canal encroachment by bone or bullet fragments (Fig. 72.1). Magnetic resonance imaging provides excellent information regarding spinal neural elements and surrounding soft-tissue integrity (Fig. 72.2), but, in the setting of retained metallic fragments, its use is controversial, particularly if retained fragments are near vital and susceptible anatomic structures, such as the spinal cord.1,8 An alternative study, such as a myelogram followed by immediate computed tomography, can assess the spinal neural elements after SCI secondary to GSWs.1 The initial care of patients with penetrating SCI begins with local wound care, most of which can occur in the emergency department. The exception is injuries with large exit wounds and physical and radiographic findings that suggest the presence of a large cavity at the injury site. If the wound has been contaminated by passage of an object through the pharynx, esophagus, or colon, or if the wound has been contaminated after injury, it is essential that wound cultures be taken from the injury tract. If the impaling object has been retained, it is important not to manipulate the object before surgery. Identification of its track and the organs violated along that path is essential for appropriate treatment.5 Premature removal of the impaling object can contaminate the entire tract (e.g., with intestinal bacteria). Every effort should be made to débride and irrigate contaminated areas before the impaled object is removed in the operating room.5 The clinician should remember to administer tetanus prophylaxis, especially if the immunization status is unknown. Fig. 72.1 This 21-year-old man had an incomplete SCI after a GSW to the thoracic spine. A bullet is seen in the spinal canal at the T4 level. Fig. 72.2 A spinal cord injury from a stab injury to the conus medullaris. (A) A sagittal T2-weighted image of the thoracic spine showing a linear track (arrow) from the skin to the conus medullaris with an associated region of increased signal within the conus medullaris, compatible with edema. (B) A sagittal T1-weighted image of the thoracic spine also showing the track (arrow) but not showing the edema within the conus medullaris. (C) A sagittal STIR image of the lumbar spine accentuates the edema along the track (arrow) and also that within the conus medullaris. (From Okubadejo GO, Daftary AR, Buchowski JM, Carrino JA, Khanna AJ. The lumbar and thoracic spine. In: Khanna AJ, ed. MRI for Orthopaedic Surgeons. New York, NY: Thieme; 2010:269–315; Figure 11.6. Reprinted with permission.) Steroids are not recommended for SCI related to penetrating spine injuries. The Second National Acute Spinal Cord Injury Study did not include GSWs.9 Three retrospective studies examining steroids in the setting of penetrating SCI suggested that steroids provide no benefit and may be associated with a higher risk of infectious complications.10–12 In the absence of any reported efficacy of such treatment, steroids are not recommended for penetrating SCI.1,10–13 Most impalement/stabbing SCIs are limited to soft-tissue damage, with minimal disruption of the osseous architecture (Fig. 72.3). Exceptions include high-energy industrial accidents involving heavy machinery, which can produce large soft-tissue and bony defects.5 For impalement/stabbing injuries or injuries with large cavities at the injury site, patients should undergo urgent spine débridement. Preoperative coordination with the trauma team is critical in the setting of collateral or multiple injuries. Intraoperatively, it is extremely important to search for and evacuate any foreign bodies (e.g., clothing) in the wounds and to obtain wound cultures. Such injuries require a minimum of 3 weeks of parenteral antibiotics with coverage specific to the organisms found at débridement.1 It is important to remember that spine infections after penetrating injury can be insidious and that at least 6 months of follow-up is necessary to declare a patient free of spinal infection.1 Associated fractures of the spine identified on imaging should be treated via standard treatment algorithms. With few exceptions, most GSWs to the spine can be treated with little to no surgery.1,14,15 Previously, radical spine débridement with bullet extraction was favored in such situations, but the best results have been reported with minimal spine débridement and protection with 1 to 2 weeks of parenteral antibiotics.15 SCIs secondary to GSWs are relatively uncontaminated, with the exception of GSWs that first penetrate the pharynx, esophagus, or colon, which require a tailored broad-spectrum antibiotic regimen of variable duration depending on the extent of visceral injury.1,15 Most GSWs to the spine are stable.1,14 For the cervical spine, the use of immobilization depends on the degree of bony ligamentous disruption: with no bony involvement, no immobilization is necessary; with the anterior vertebral body fractured or posterior bony elements, a rigid cervical collar can be considered; with both the anterior vertebral body and posterior elements disrupted, halo vest immobilization is recommended.1 For the thoracic/lumbar spine, the use of immobilization also depends on the degree of bony and ligamentous disruption: if none or only the anterior or posterior bony elements, no immobilization is needed; if both the anterior and posterior bony and ligamentous structures, a thoracolumbosacral orthosis is recommended when the patient is out of bed.1 After 6 to 8 weeks of immobilization, flexion and extension conventional radiographs of the affected region are obtained to evaluate healing.1 In contrast to closed SCIs, operative intervention to establish stability after a GSW of the spine is rarely necessary.1,14 Fig. 72.3 CT images showing a knife blade that broke off in the spinal lamina in the midthoracic spine. (A) Sagittal reconstructed view. (B) Axial view.
Penetrating Injuries to the Spine
![]() Classification
Classification
![]() Evaluation
Evaluation
History
Physical Examination
Spinal Imaging
![]() Treatment
Treatment
Initial Care
Impalement/Stabbing Injuries
Gunshot Wounds
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






