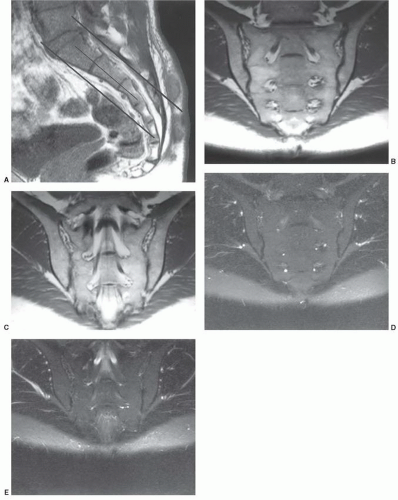
techniques should be used to reduce motion artifact in the upper pelvis. Thinner slices can be used if a more defined area of the anatomy is to be studied.
flip angle 40°).22 Thin section fast scan three-dimensional techniques can be reformatted in multiple planes to more easily assess subtle changes in articular cartilage.23 Axial and coronal or sagittal T1-weighted spin-echo and T2-weighted turbo spin-echo sequences provide initial screening of the thighs (Table 6.1).
Table 6.1 MR Examinations of the Pelvis, Hips, and Thighs (based upon 1.5 T units) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
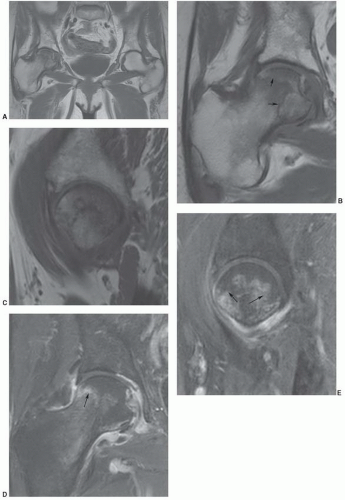
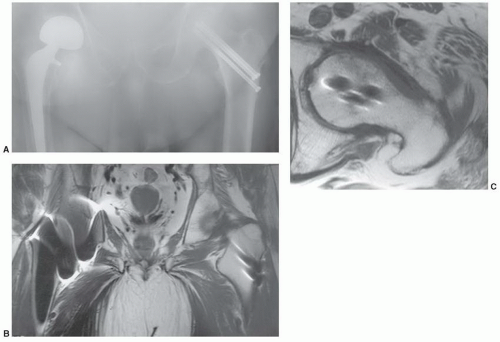
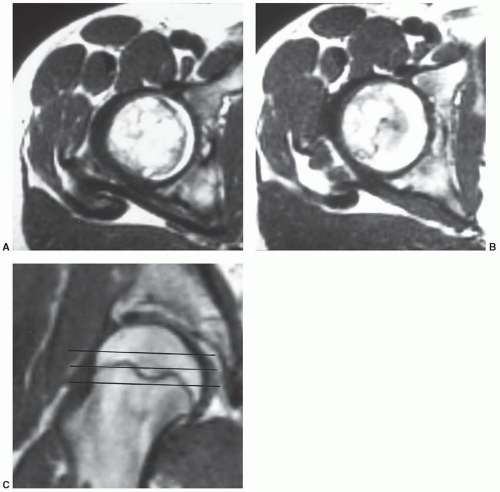
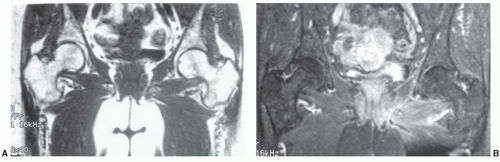
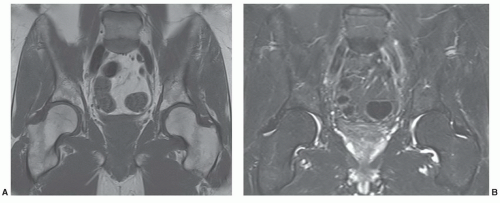 Figure 6.3 3.0 T coronal images of the pelvis and hips. A: Coronal 650/10 image with 1 echo train. B: Coronal turbo spin-echo 3800/62 with 7 ET. |
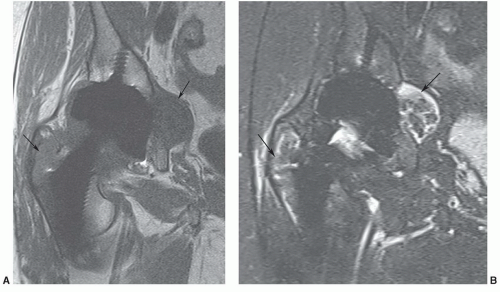
changes in articular cartilage and synovium.19,21,24,25 Conventional sequences are usually performed followed by fat-suppressed T1-weighted sequences after contrast injection (Fig. 6.7).
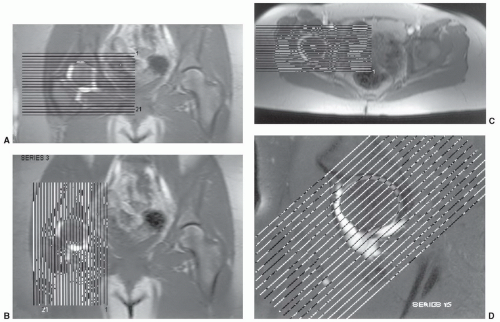
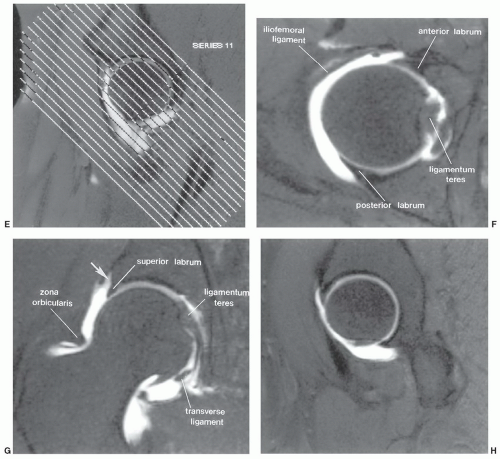
that radial imaging does not add significant new information to the study.30 Therefore, we do not perform radial imaging at our institution. T1-weighted fat-suppressed spin-echo and turbo spin-echo T2-weighted sequences are most commonly used with MR arthrography.20,27 Three-dimensional gradient-echo sequences (30/9, 45° flip angle) can also be utilized.26,31
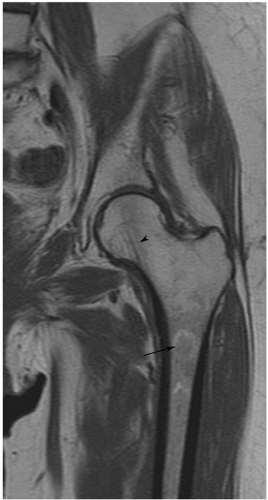
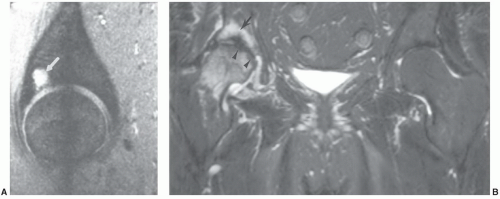
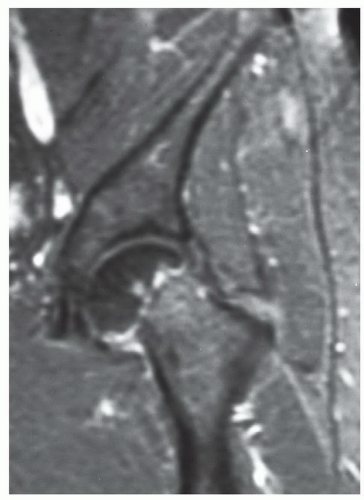 Figure 6.7 Coronal post-contrast fat-suppressed T1-weighted image demonstrates a femoral neck fracture with no enhancement of the femoral head due to vascular injury. |
T1-weighted images are useful for evaluating subtle changes.2,10
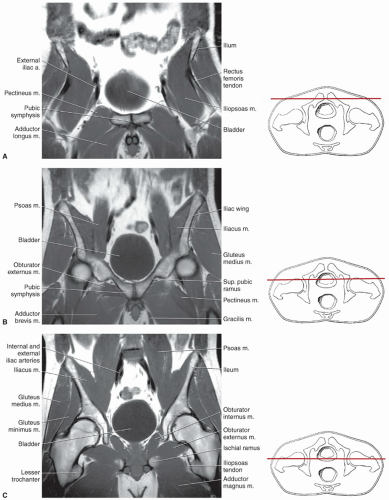
pubic and arcuate ligaments that encase a fibrocartilaginous disc. The disc lies between the two pubic bones (Figs. 6.9 and 6.12).37,38 The sacroiliac joint is a synovial joint with posterior and anterior ligamentous support (Fig. 6.12). The posterior ligaments are stronger than the anterior ligaments, which allow some anterior motion. In addition, there are several accessory ligaments that assist in the support of the sacroiliac joint. These include the sacrotuberous ligament, which extends from the inferolateral margin of the sacrum to the ischial tuberosity; the sacrospinous ligament, which extends from the lower margin of the sacrum to the ischial spine; and the iliolumbar ligament, which extends from the anterior inferior transverse process of L5 and passes inferiorly to blend with the anterior sacroiliac ligament along the base of the sacrum. These ligamentous structures appear dark or have no signal intensity on MR images. The synovial cavity of the sacroiliac joint contains only a small amount of fluid. Joint fluid is most easily identified on axial T2-weighted or contrast-enhanced MR images (Fig. 6.7).37,38
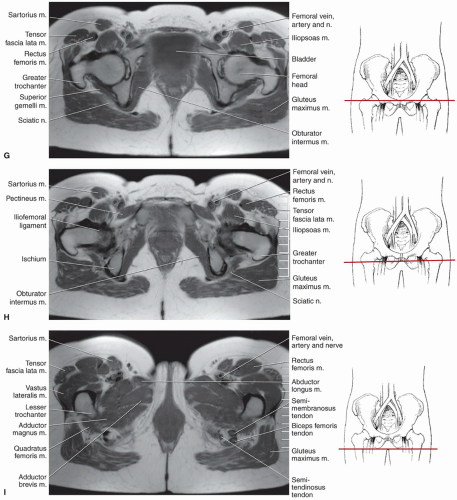
to the lower part of the anterior inferior iliac spine and body of the ilium. The base of this triangular ligament attaches to the intertrochanteric lines (Fig. 6.15). The ischiofemoral ligament, the thinnest of the three major ligaments, arises from the ischium behind and below the acetabulum. Its upper fibers are horizontal; its lower fibers extend upward and laterally and attach to the upper posterior neck at the junction of the greater trochanter. The vascular supply of the hip and femoral head is important, especially in the etiology of osteonecrosis. This is discussed in depth in the section on osteonecrosis.34,38,41,42
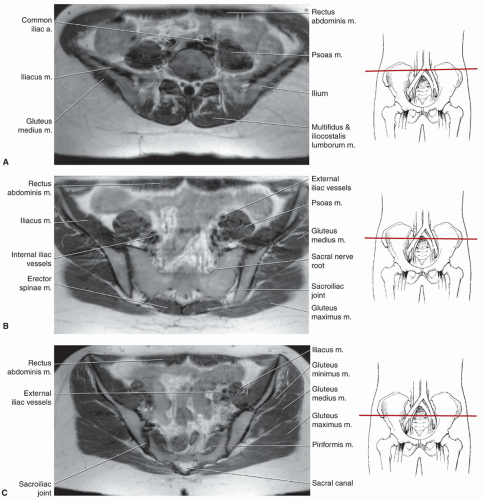
images.44,45 The bulk of the iliacus muscle run parallel to the iliopsoas tendon and attach to the proximal femur. In some cases, a small iliacus tendon runs parallel to the iliopsoas tendon as it attaches to the lesser trochanter. The iliopsoas tendon is separated from the iliacus muscle and tendon by a small amount of fatty tissue (Fig. 6.18).44,45
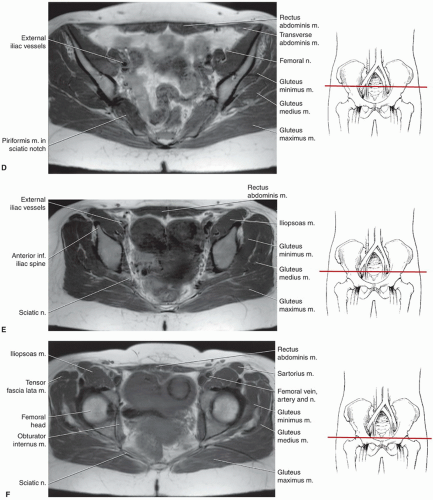
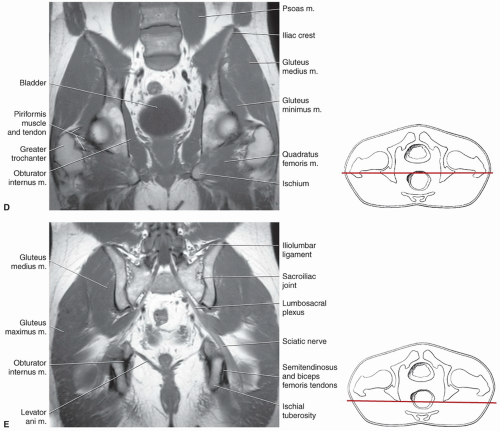
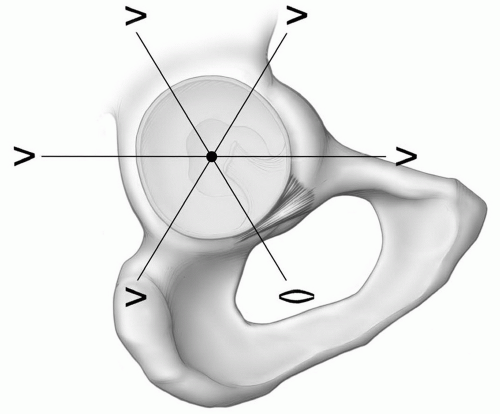
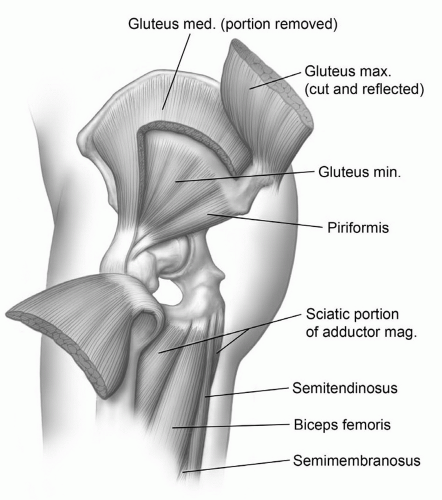
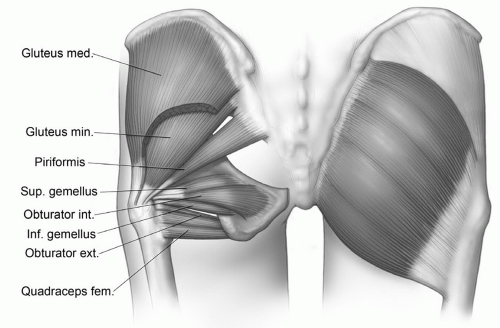
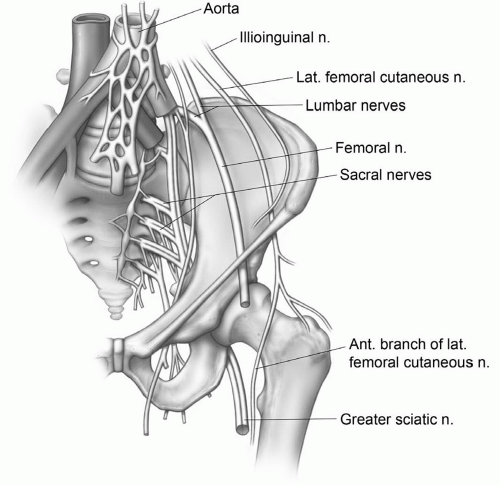
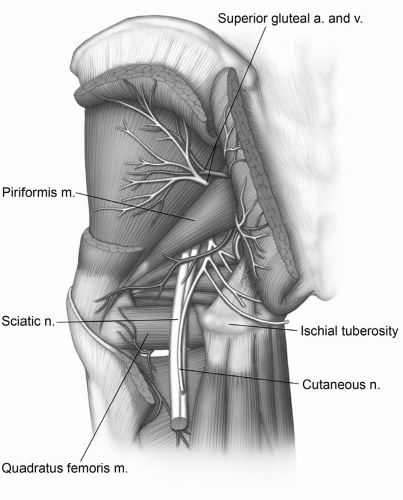
internal rotation. External rotation of the hip is accomplished by the gluteus maximus and the short rotators of the gluteal region including the piriformis, obturator internus, and the gemelli muscles (Fig. 6.19).34,38,44
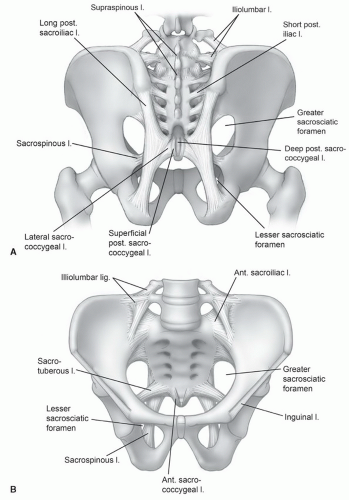 Figure 6.12 Illustration of the ligaments of the posterior sacroiliac region (A) and anterior sacroiliac region (B) and symphysis. |
these bursae are seen as well defined, high intensity lesions near the insertions (T2-weighted sequences).10,47
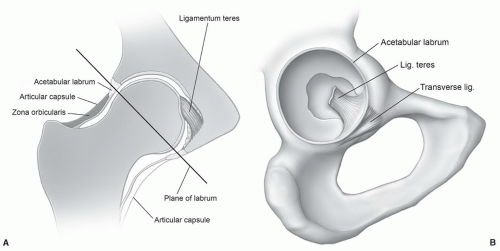 Figure 6.13 A: Coronal illustration of the hip demonstrating the major articular components and capsule and the plane (line) of the labrum. B: Enface illustration of the acetabular fossa and labrum. |
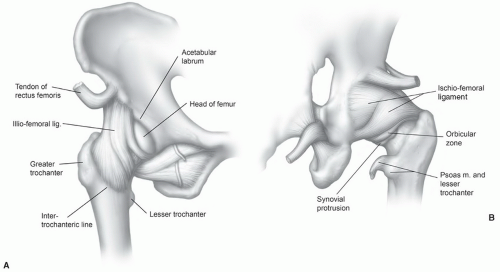 Figure 6.15 Illustration of the supporting ligaments of the hip from anterior (A) and posterior (B). |
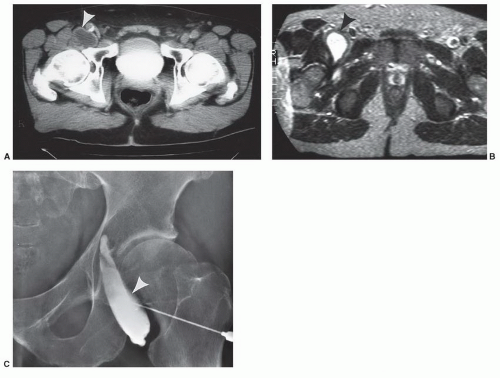
arises from the adjacent borders of the last thoracic and first lumbarvertebrae and extends along the anterolateral margin of the psoas major to insert on the iliopectineal eminence of the innominate bone. The iliacus takes its origin from the internal surface of the ilium below the iliac crest and passes slightly obliquely anterior to the hip joint, inserting with the psoas muscle in the lesser trochanter (Fig. 6.21). An important bursa (can cause clinical symptoms and local hip pain) is the iliopsoas bursa, which lies beneath the iliopsoas muscle just as it crosses the anterior surface of the hip joint. This bursa may approach 3 to 7 cm in length and 2 to 4 cm in width. The bursa communicates with the hip joint in up to 15% of patients (Fig. 6.22).34,38,44,46
Table 6.2 Muscles of the Pelvis, Hips, and Thigh | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
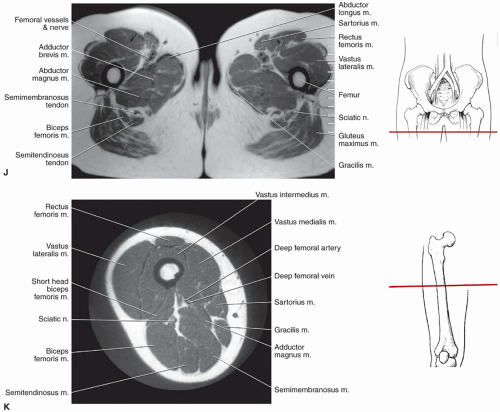
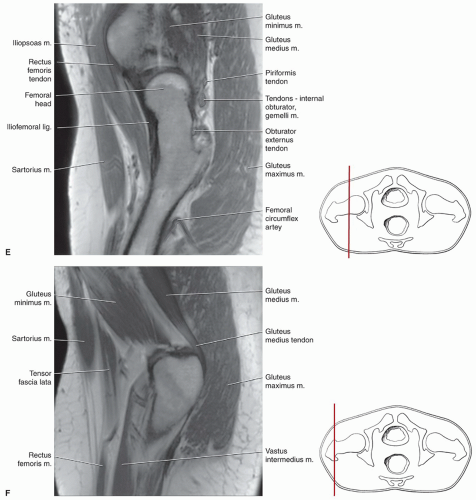
is from the femur just below the greater trochanter and posterolaterally along the margin of the linea aspera and intermuscular septum. The vastus intermedius inserts along the upper lateral margin of the patella forming a portion of the quadriceps tendon. The vastus medialis makes its origin anteriorly from just below the lesser trochanter and the medial and posterior aspect of the femur. It extends inferiorly and inserts into the medial aspect of the rectus femoris tendon. The vastus intermedius covers a major portion of the front and medial and lateral aspects of the femur (Fig. 6.21).34,37,48 It is completely covered superficially by the vastus lateralis and medialis on its sides and the rectus femoris anteriorly. Distally, its fibers fuse with the vastus medialis and lateralis to insert in the posterior upper surface of the patella.33,34,37,38
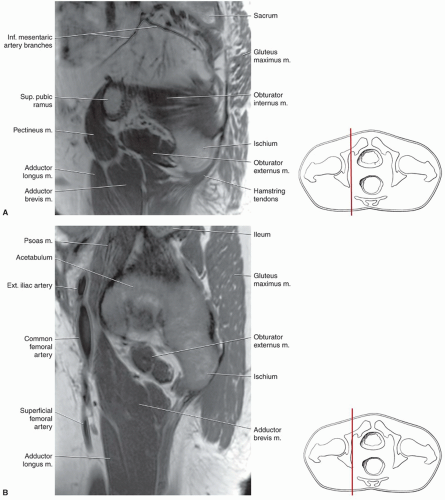
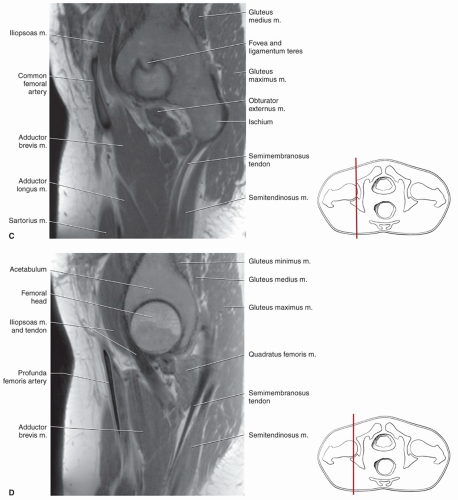
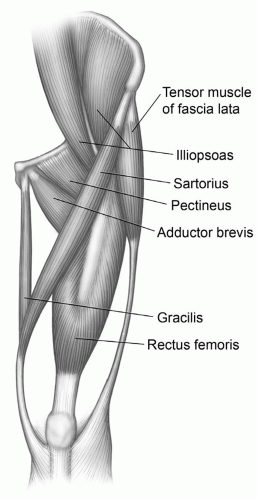
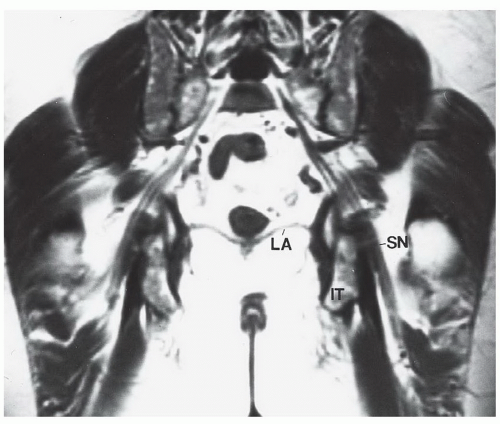
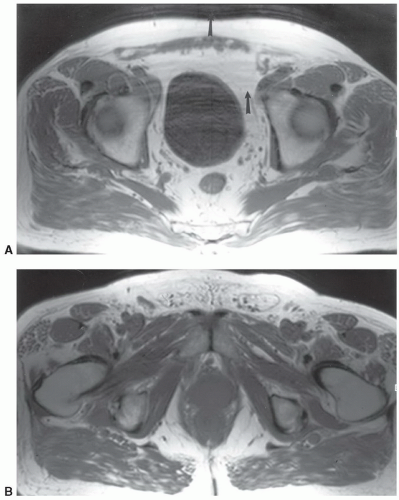
femur that extends inferiorly from the lesser trochanter to the linea aspera (Fig. 6.21).37,38 Anatomists often include the adductor brevis, adductor longus, adductor magnus, gracilis, and obturator externus in the anterior medial muscle group, as all of these muscles are innervated by the obturator nerve (Table 6.2).38 In the axial plane, the adductor longus is the most anterior of the adductor muscles in the upper thigh (Fig. 6.9). The adductor longus takes its origin from the pubic bone superiorly near the pubic symphysis and extends in a triangular fashion inferiorly and laterally to insert along the medial aspect of the linea aspera at the level of the mid femur. This muscle forms the floor of the femoral triangle along with the pectineus and iliopsoas muscle. The adductor brevis arises from a broad tendon from the body and inferior ramus of the pubis and expands in a triangular fashion to insert in the upper half of the linea aspera. It is typically seen between the adductor longus and magnus on the axial views with the gracilis running along its medial aspect (Figs. 6.9 and 6.21).10,33,34,37,38
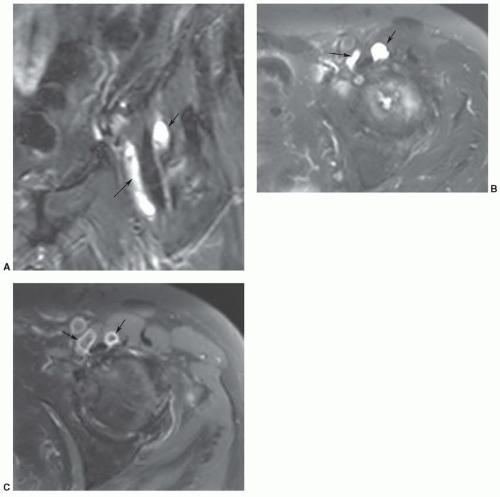
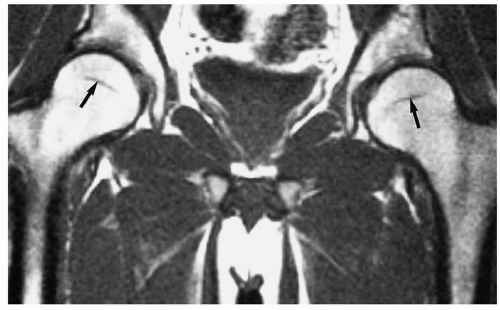
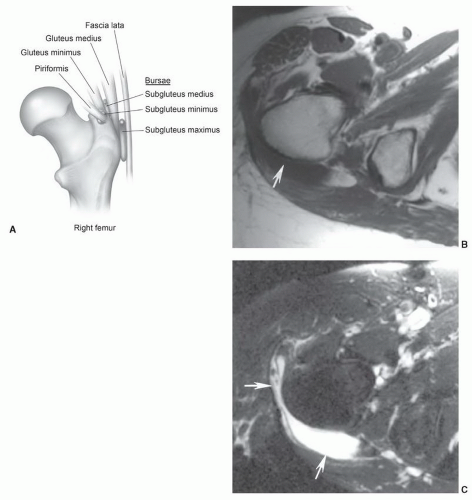 Figure 6.20 A: Illustration of bursae near the greater trochanter. Axial T1- (B) and T2-weighted (C) images demonstrating trochanteric bursitis (arrows). |
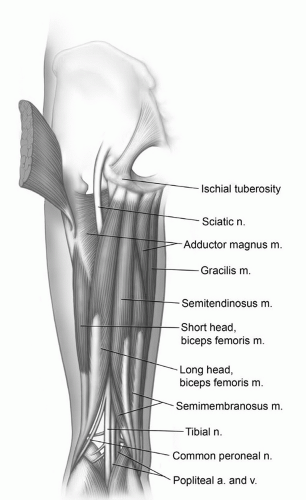
(Figs. 6.9, 6.10, and 6.21). It passes medially along the thigh, superficial to the adductor muscles (Fig. 6.10). Near the knee, it lies first between the sartorius and semimembranosus and then between the sartorius and semitendinosus. Below the knee, the tendon curves anteriorly and inserts in the upper medial anterior tibia with a bursa termed the anserine bursa intervening between gracilis, sartorius, and semitendinosus tendons and the tibia.10,34
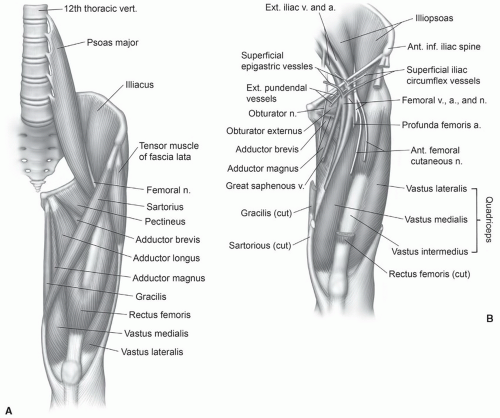 Figure 6.21 Illustration of the anterior musculature (A) and neurovascular structures of the thigh (B). |
lateral to the common origin of the biceps femoris and semitendinosus (Fig. 6.23). The muscle becomes tendinous posterior to the medial meniscus as it crosses the knee. At the level of the joint, it gives off an oblique expansion that also attaches to the medial collateral ligament. Its insertion is the posterior medial aspect of the upper tibia just below the knee.33,34,37,43,44
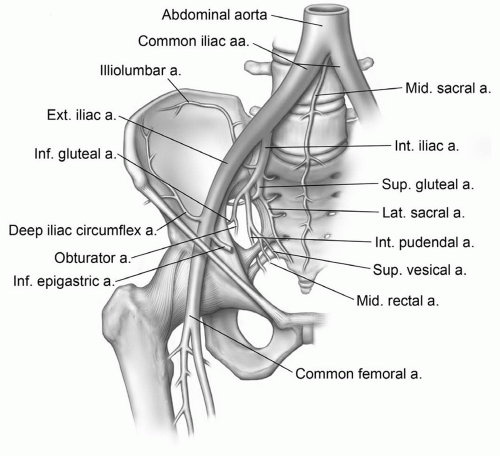
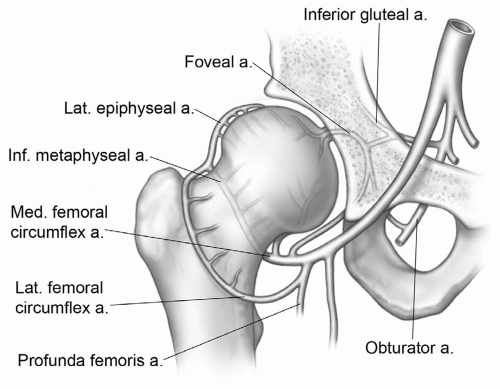
circumflex arteries and branches of the obturator artery (via ligamentum teres) supply the hip. The superficial femoral and deep femoral (profunda) arteries form slightly distal to this level (Fig. 6.24).2,38,41; they branch at about the same level as the superficial femoral and saphenous veins (Fig. 6.24). The course of the major arteries and companion veins is easily followed on contiguous axial MR images (Fig. 6.9). In the upper thigh (Fig. 6.24), the superficial femoral artery lies anterior to the adductor longus and deep to the sartorius. The profunda femoris artery and vein lie more laterally between the adductor longus and magnus near the linea aspera of the femur (Fig. 6.9). Perforating branches are usually identifiable between the adductor magnus and hamstring muscles just posterior and slightly lateral to the linea aspera of the femur.34,38 Today, MR angiography is capable of demonstrating all major vessels (Fig. 6.27).
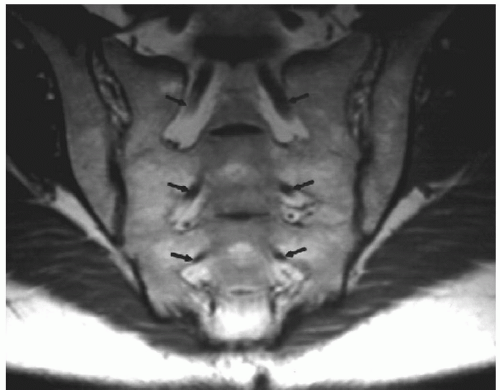 Figure 6.27 Oblique T1-weighted coronal images demonstrating the sacral nerve roots (arrows) surrounded by fat as they exit the ventral foramina. The sacroiliac joints are also well demonstrated. |
other parameters. There are new work-in-progress processing techniques that have dramatically improved the utility of MR imaging in the presence of orthopedic implants (Fig. 6.32). Titanium implants produce less artifacts than cobaltchromium alloys due to reduced ferromagnetic content.52,53 This section focuses on bone and soft tissue variants, which require further discussion.54,55
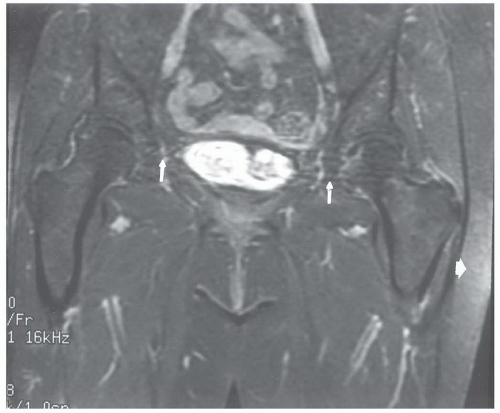 Figure 6.29 Coronal T2-weighted, fat-suppressed MR image of the pelvis demonstrating motion artifact (upper arrows) and asymmetric fat suppression (large white arrow). |
changes vary with the extent, eccentric nature, and time since the activity occurred.58 Typically, the entire muscle is involved and changes usually are not similar to neoplasms or other soft tissue pathology.
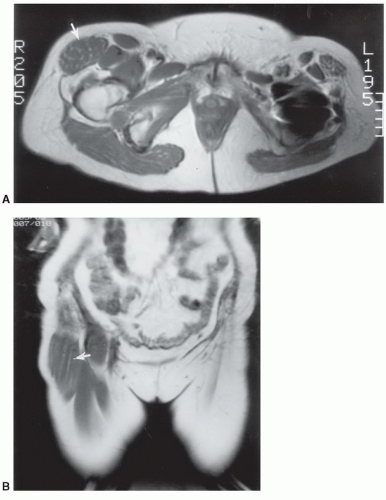 Figure 6.33 Hypertrophy of the tensor fascia lata. Axial (A) and coronal (B) T1-weighted images demonstrate marked enlargement of the muscle that was felt to be a soft tissue mass clinically. |
and femur can lead to a false-positive diagnosis such as osteonecrosis or metastasis (Fig. 6.39).64
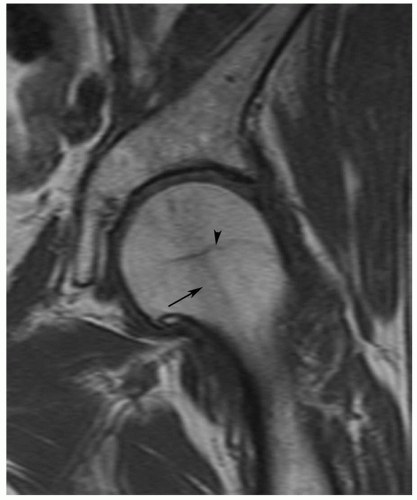 Figure 6.38 Coronal T1-weighted image of the hip demonstrating linear low signal intensity in the femoral neck (arrow) due to the normal trabecular pattern. There is also a physeal scar (arrowhead). |
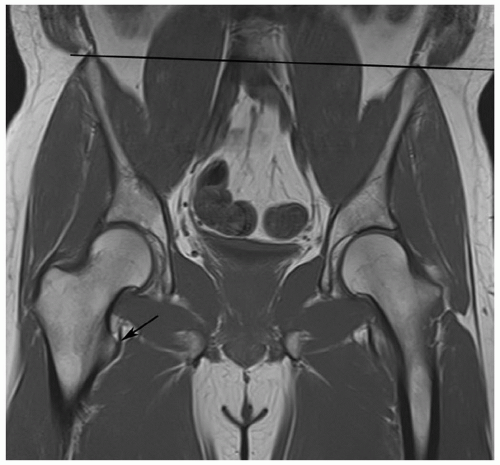
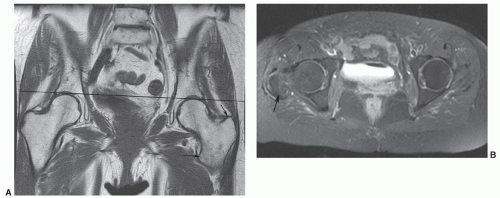
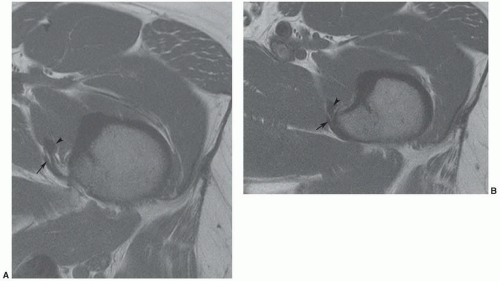
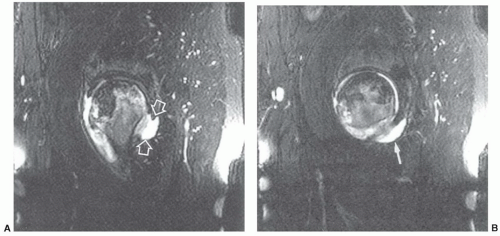
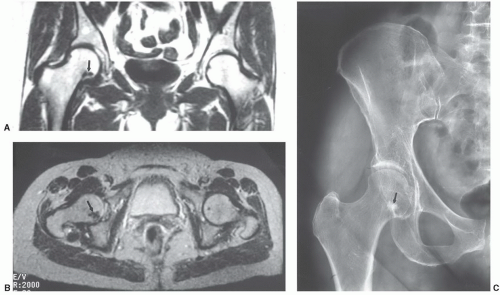
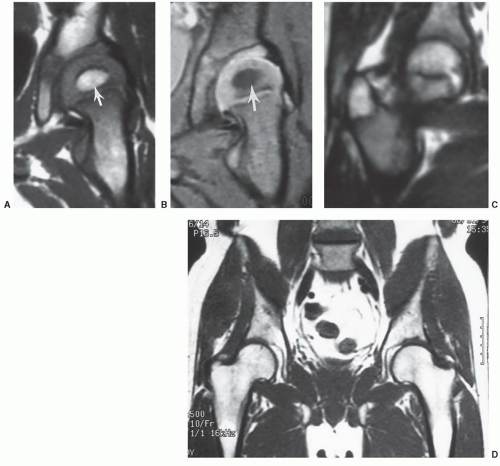
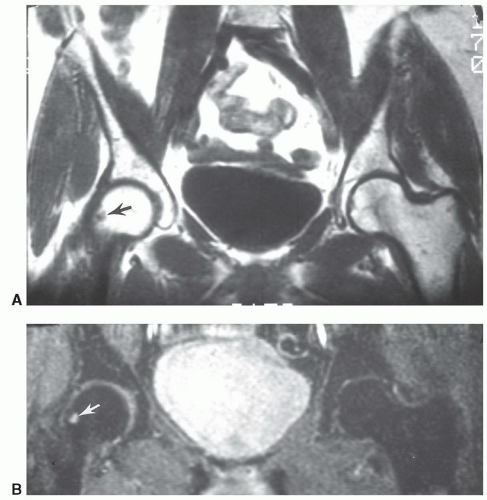 Figure 6.40 Coronal T1- (A) and axial T2-weighted (B) images of the pelvis demonstrating a typical herniation pit (arrow). |
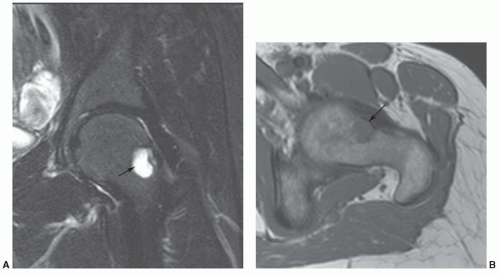 Figure 6.41 Large herniation pit. Coronal T2- (A) and axial T-weighted (B) images demonstrating a large herniation pit (arrow) on the left. |
Table 6.3 Etiology of Osteonecrosis | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
Table 6.4 Staging of Osteonecrosis of the Femoral Head | |||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||
quickly (2 to 4 minutes) using a 30- to 42-cm FOV, 4-mm-thick sections, 1 NEX, and a 256 × 256 or 192 × 256 matrix. This approach may provide a simple screening technique for high-risk patients.10 Tervonen et al.126 detected occult osteonecrosis in 6% of asymptomatic high-risk patients. More recently, Iida et al.75 demonstrated that 85% of high-risk patients (steroid, transplant, etc.) progressed from marrow edema to advanced osteonecrosis.
Table 6.5 Classification of Femoral Head Osteonecrosis | ||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||
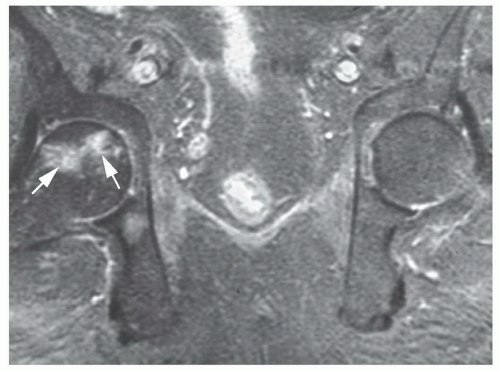 Figure 6.49 Coronal post-contrast fat-suppressed T1-weighted image demonstrates a focal area of necroses in the femoral head with surrounding enhancement or hyperemia (arrows). |
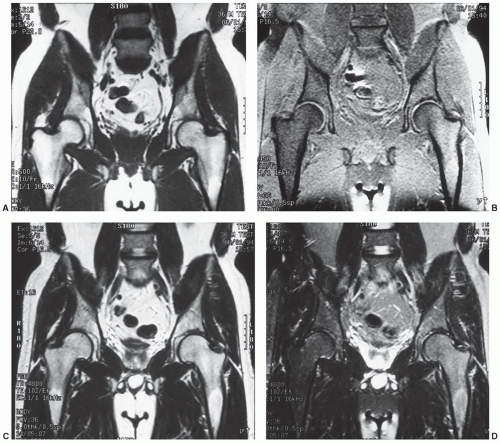
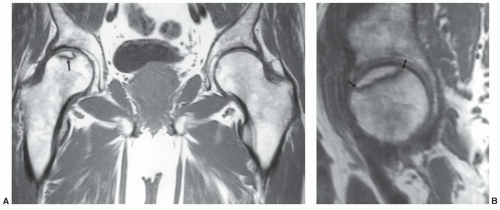
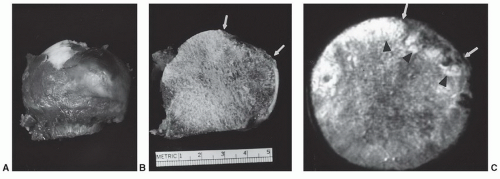
prior to fat cell necrosis.91,92 Osteocytes show necrotic changes shortly after hemopoietic cells.85 It is not unusual to demonstrate mixed necrosis and survival if changes are early. Early animal studies show MR images remain normal until about the seventh day. Beginning on the seventh day, an inhomogeneous loss of signal intensity can be demonstrated onT1-weightedimages. These changes correspondhistologically to lymphocytic infiltration.96,111 This inhomogeneity progresses over the first 16 days until day 20, when a more homogeneous loss of signal intensity in the femoral head becomes evident (Fig. 6.52). This correlates with increased lymphocyte infiltration and early fibrosis. As expected, radiographs remain normal during this time period (Table 6.4).10,114,115 Early uniform loss of signal intensity in the femoral head and neck on T1-weighted images that is similar to transient bone marrow edema has also been reported (Fig. 6.52).10,74,122,124,134,138,139 Conservative management is employed with either condition. However, follow-up studies are important in clarifying which disorder is present and to exclude other inflammatory diseases, specifically infection.74,131,134
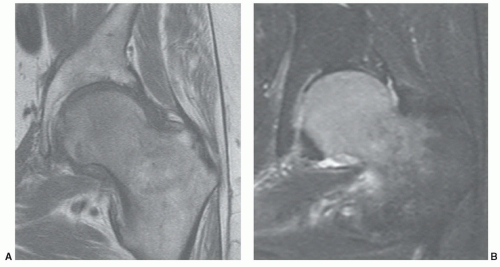 Figure 6.52 Coronal T1- (A) and T2- (B) weighted images demonstrating abnormal signal intensity in the femoral head and upper neck due to marrow edema. |
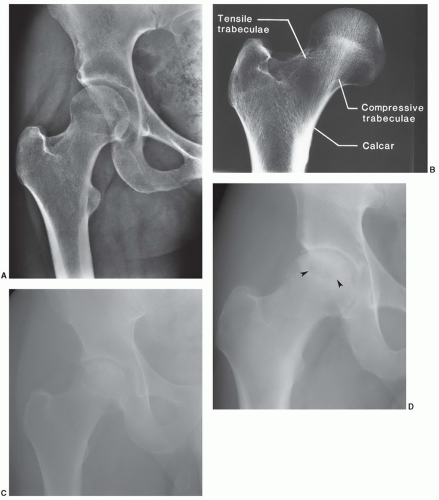
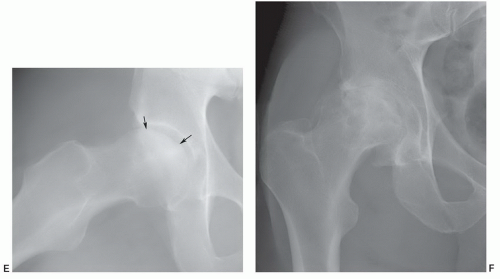
space changes are definitely more easily assessed with radiographs (Fig. 6.45D-F
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree