the anatomy and characterize the lesion (Table 11.1). An effective screening examination can be accomplished by the beginning with either a coronal or sagittal scout (SE 500-400/10-20). This should include the full area of the hand and wrist to be examined. The sequences and image planes vary with clinical indication. One can begin with a standard screening examination and add additional sequences or gadolinium when indicated. T1- and T2-weighted sequences are performed. We use conventional spin-echo T1-weighted sequences and turbo spin-echo (FSE) T2-weighted sequences with fat suppression in most cases (Table 11.1). Conventional short TI inversion recovery (STIR) sequences have been replaced with FSE inversion recovery sequences. Fluid and pathologic tissues have high signal intensity in comparison to suppressed marrow and fat signal.
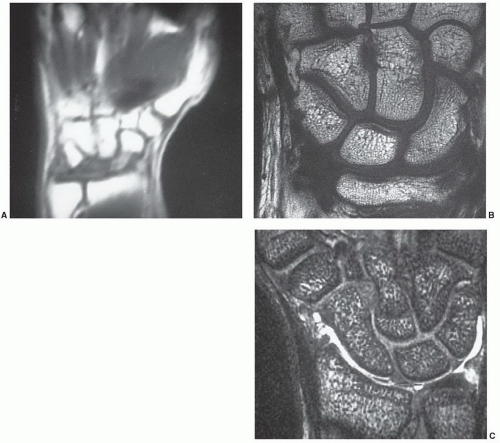
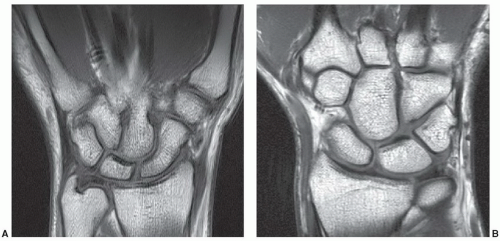
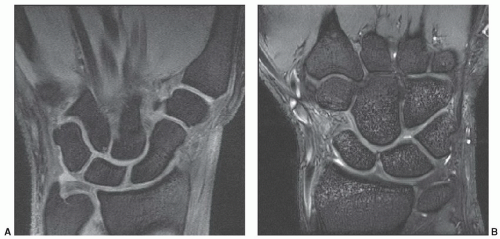
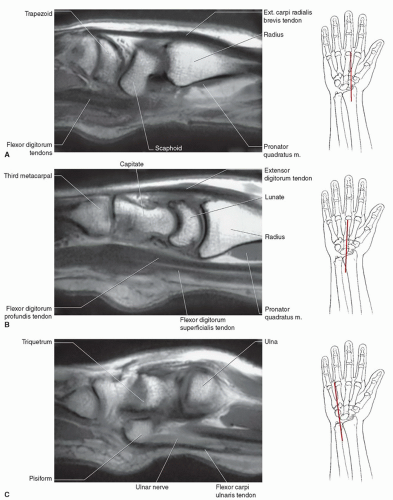
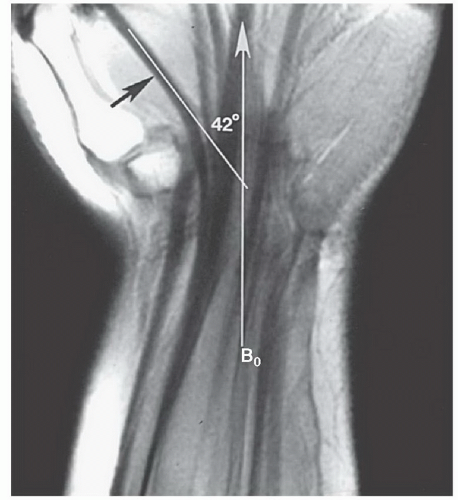
anatomies, oblique planes are useful (Table 11.2). This is particularly true for the carpal bones (Fig. 11.8) and individual digits of the hand.
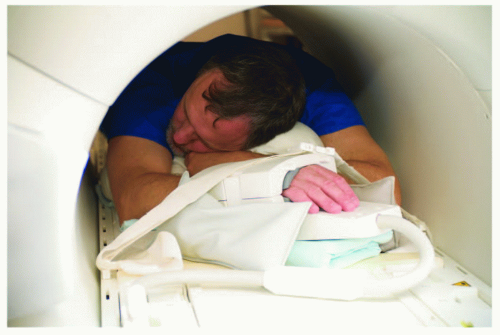
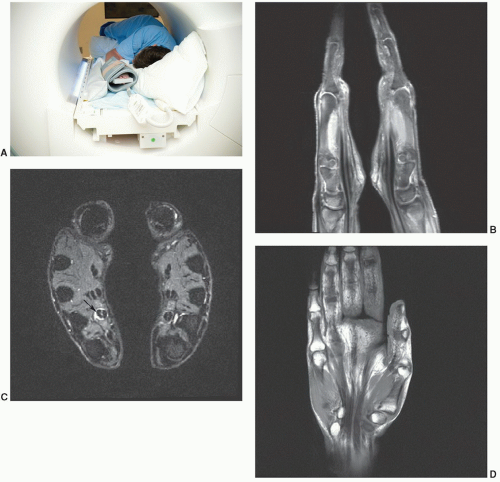
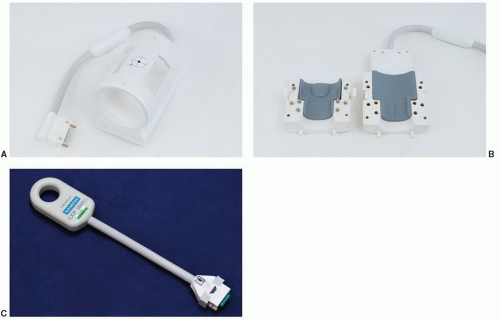 Figure 11.4 Coils for hand and wrist imaging. A: Volume quadrature coil. B: Opening volume coil. C: Digital coil for isolated wrist or finger imaging. |
Table 11.1 MR Techniques for Hand and Wrist Imaging at 1.5 T | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Table 11.2 MR Imaging of the Hand and Wrist: Image Planes | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
injected. We begin with the most symptomatic region or area of suspected pathology.7,35,36,37
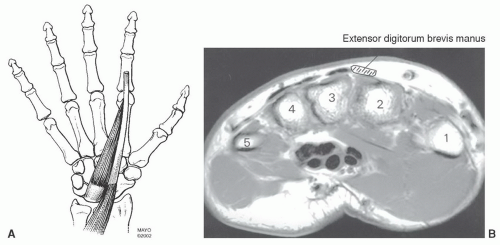
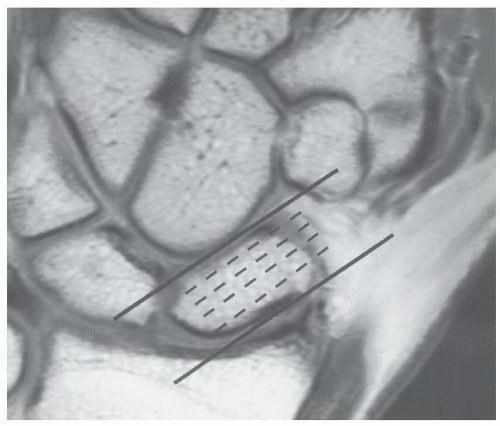 Figure 11.8 Coronal T1-weighted image demonstrating selection of oblique sagittal images to evaluate the scaphoid. |
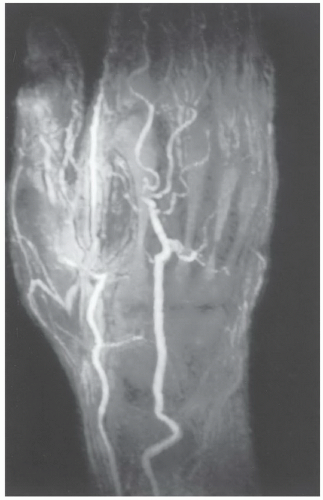 Figure 11.11 MR angiogram of the hand and wrist in a patient with vasculitis. There are multiple occlusions and vascular irregularities. |
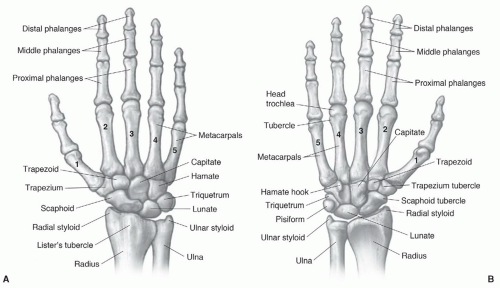 Figure 11.12 Osseous structures of the hand and wrist seen dorsally (A) and from the palmar surface (B). |
a ranking of 8 (range 1-9). Similar rankings are achieved for chronic wrist problems and soft tissue injuries.44,45
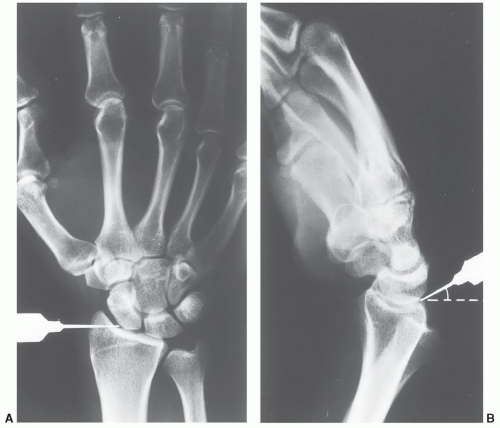
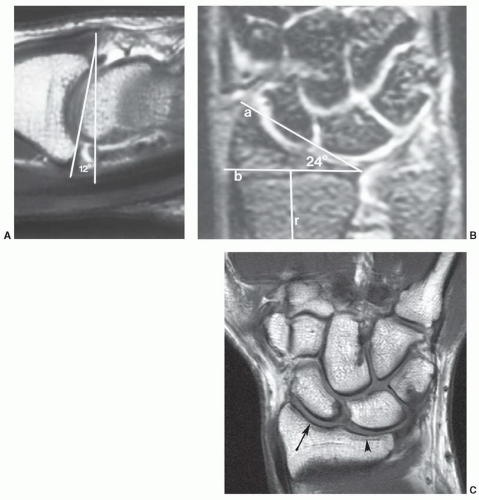
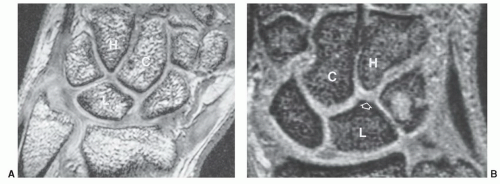
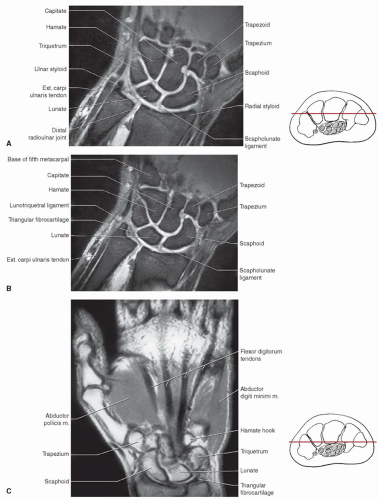
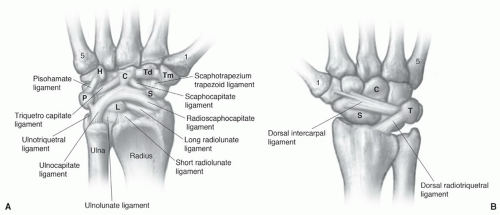
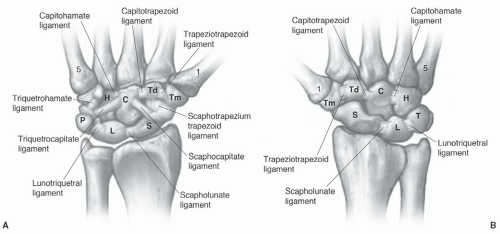
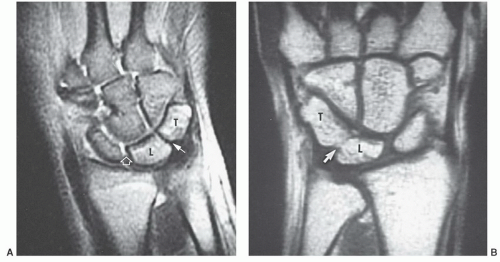
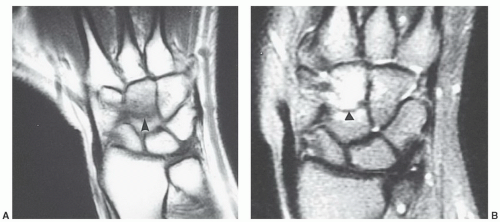
surfaces of these bones should form a smooth, unbroken arch in the coronal plane. In the sagittal plane, the angle formed by the scaphoid and lunate should be between 30° and 60°. A second osseous anatomic group, or the distal carpal row, consists of the trapezoid, capitate, and hamate. The third compartment is composed of the trapezium and five metacarpals.21,46,56,58
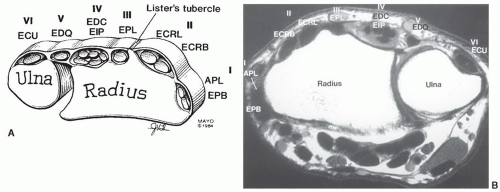
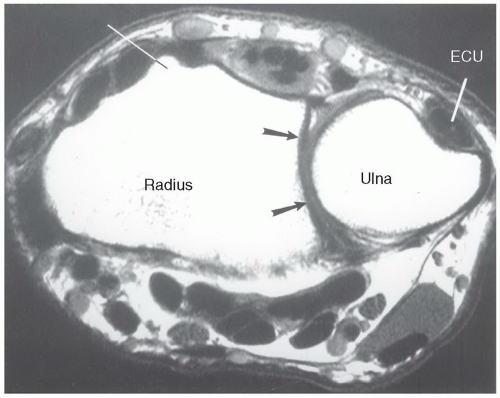 Figure 11.14 Axial T1-weighted image of the wrist demonstrating Lister tubercle, the sigmoid notch (arrows), and the groove in the dorsal ulna for the ECU. |
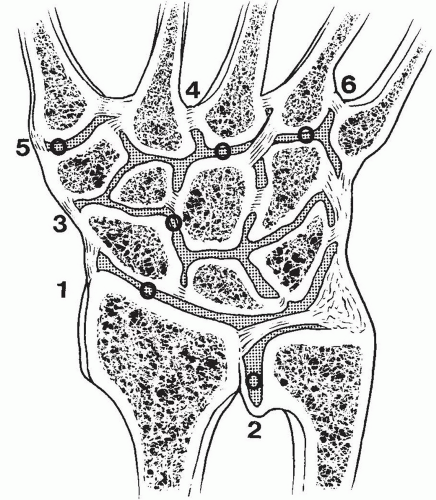
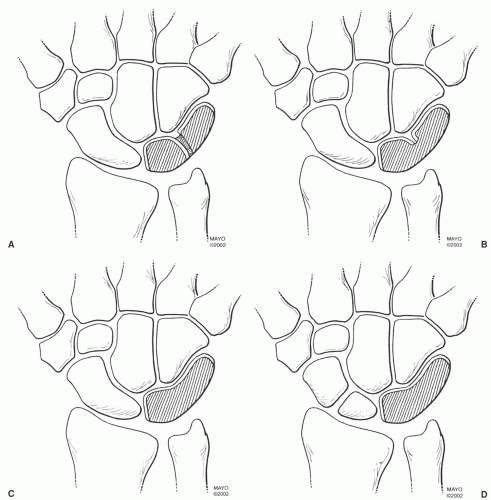
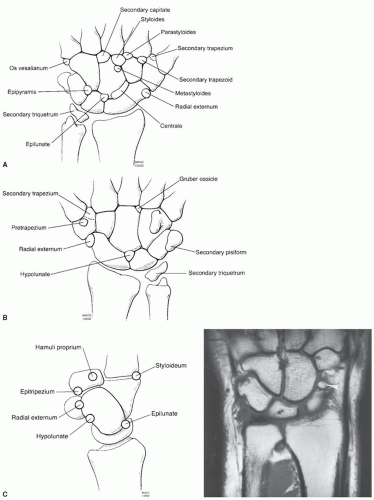
capitate and hamate. These may be fibrous, cartilaginous, or osseous.62,64 A more complete discussion of osseous variants is included in the Pitfalls section of this chapter.
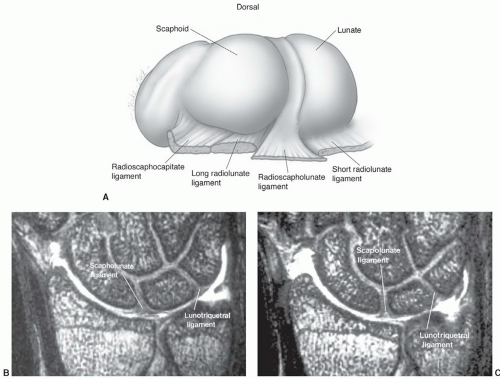
radioscapholunate were demonstrated in 66% and 26%, respectively. Three-dimensional techniques were used.
of patients. An amorphous appearance was noted in a few patients by Smith and Snearly (Fig. 11.24).50 Signal intensity is not always uniformly low, similar to variations described in the scapholunate ligament (Fig. 11.24).50,52
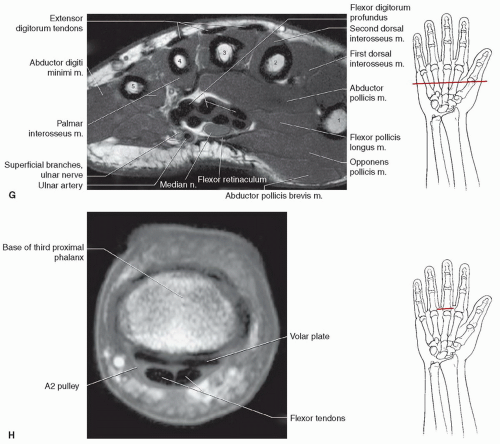
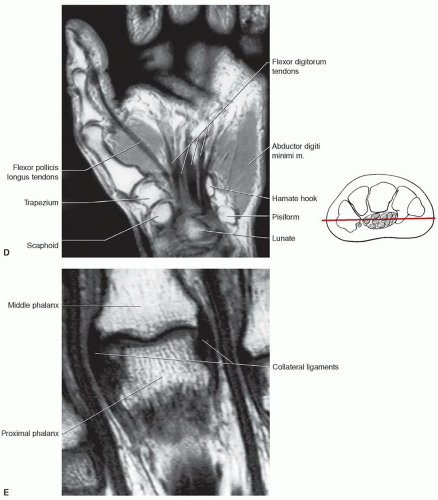
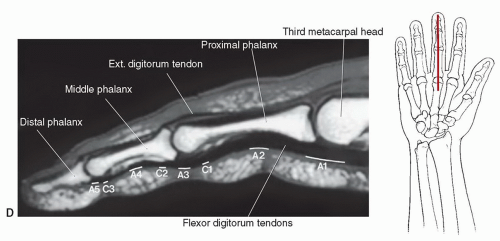
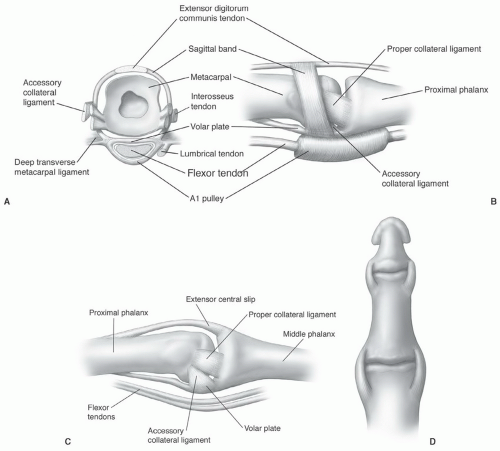
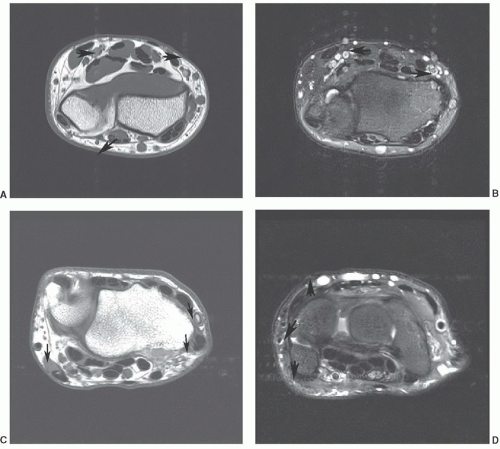
(Figs. 11.18E and 11.26).21,76 These ligaments are tight in extension and relax with flexion of the joints. The collateral ligaments are seen on axial and coronal MR images (Figs. 11.17 and 11.18). The palmar plate is clearly seen on axial and sagittal images.76
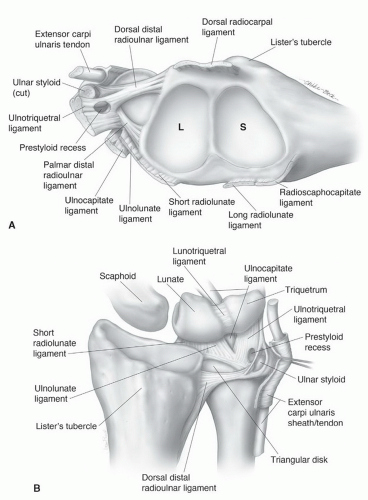 Figure 11.20 A: Distal radius including the scaphoid (S) and lunate (L) fossae and the TFCC. B: Ulnocarpal ligament complex and TFCC are seen dorsally. |
 Figure 11.23 Signal intensity patterns in the scapholunate ligament described by Smith.52 Type I, uniform low signal intensity; type II, central intermediate signal intensity; type III, distal intermediate signal intensity; type IV, proximal intermediate signal intensity; type V, intermediate signal intensity extending through the ligament. |
 Figure 11.24 Signal intensity variations in the lunotriquetral ligament described by Smith and Snearly.50 Type I, homogenous low signal intensity; type II, distal intermediate signal intensity; type III, intermediate signal intensity extending through the ligament; type IV, proximal intermediate signal intensity. |
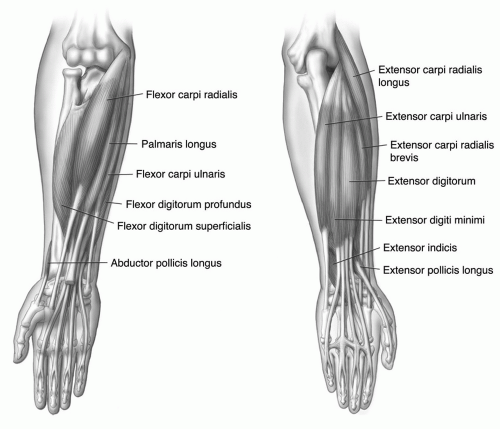
trapezoid. The muscle extends distally to form a tendon that inserts on the radial flexor side of the base of the proximal phalanx of the thumb. The primary function is flexion and rotation of the thumb. The opponens pollicis is partially covered by the abductors and flexors of the thumb and arises from the flexor retinaculum and trapezium to insert on the radial surface of the diaphysis of the first metacarpal. The adductor pollicis arises with both oblique and transverse heads. The transverse head arises from the ulnar surface of the third metacarpal diaphysis and the oblique head from the base of the third metacarpal and flexor aspects of the trapezium, trapezoid, and capitate. The triangular muscle extends to insert at the base of the proximal phalanx of the thumb. This muscle serves to adduct the metacarpal and flex the MCP joint of the thumb (Table 11.3).46,56
Table 11.3 Muscles of the Hand | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
the hand to insert along the ulnar side of the base of the fifth proximal phalanx. This muscle abducts the little finger at the MCP joint. It acts along with the dorsal interosseous muscle to assist in abduction or spreading of the fingers. The flexor digiti minimi brevis arises more distally than the abductor digiti minimi and takes its origin from the hook of the hamate and flexor retinaculum. Thismuscle passes more obliquely and medially and inserts in the same position as the abductor. The main function of this muscle is as flexor of the fifth MCP joint. The third and final muscle of the deep hypothenar group is the opponens digiti minimi. This muscle is the deepest and arises deep to the abductor and flexor from the flexor retinaculum and distal hook of the hamate, taking an oblique course to insert along the ulnar aspect of the fifth metacarpal diaphysis. This muscle draws the fifth metacarpal anteriorly. All of the hypothenar muscle groups is innervated by the deep branch of the ulnar nerve (Table 11.3).46,56
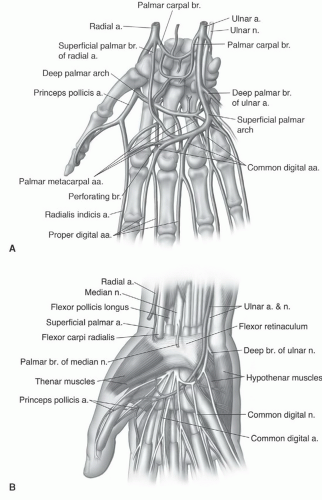
the pisiform level, the nerve and accompanying vascular structures lie between the volar carpal ligament and flexor retinaculum in a space commonly known as the Guyon’s canal.54,56 Lesions proximal to or within the canal can produce both sensory and motor abnormalities in the ulnar nerve distribution.54,56
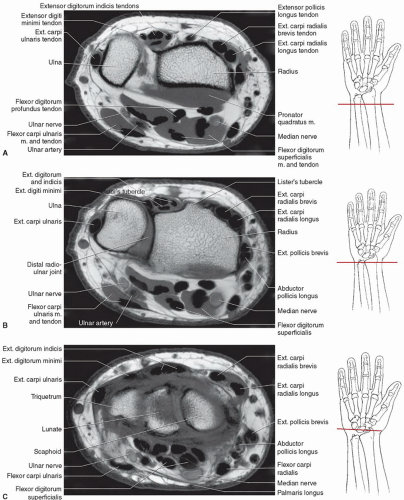
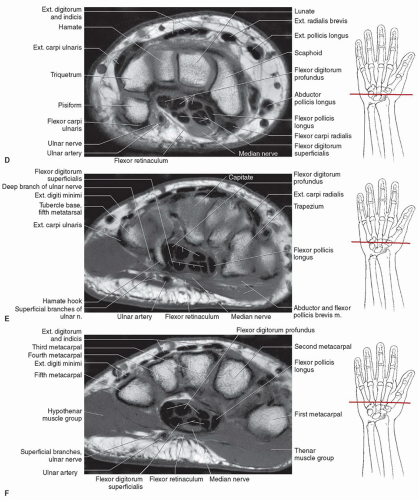
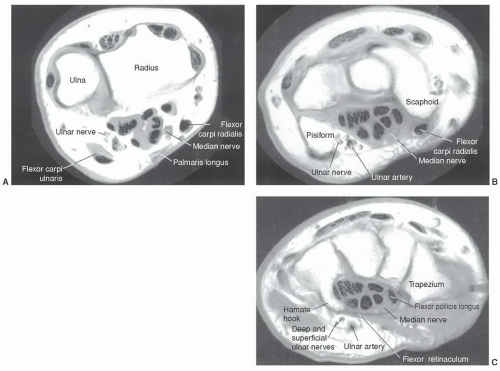 Figure 11.29 Axial MRI demonstrating the relationships of the ulnar and median nerves at the level of the distal radioulnar joint (A), pisiform (B), and hamate hook (C). |
do occur, they involve the most commonly fractured carpal bone, the scaphoid.56,62 The most common appearance is two separate ossicles separated at the waist, a common site of scaphoid fractures. The capitate and hook of the hamate may also develop from multiple ossification centers. When this occurs, differentiation from fracture may be difficult with MRI.63 Hypoplastic hamate hooks have been described in females.63,97
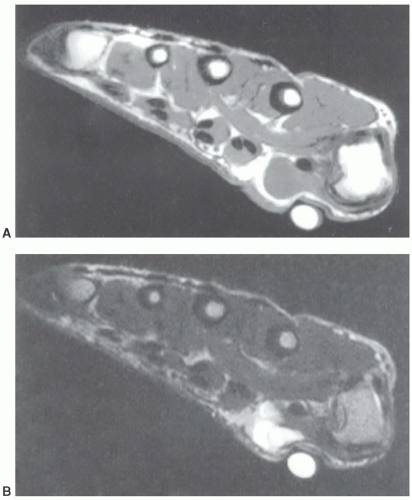 Figure 11.30 Axial T1- (A) and T2-weighted (B) images. The large vitamin E capsule compresses and distorts the underlying anatomy and ganglion cyst (arrow). |
Gruber-Ossiculum lies between the capitate, hamate, and the third and fourth metacarpal bases.62,64
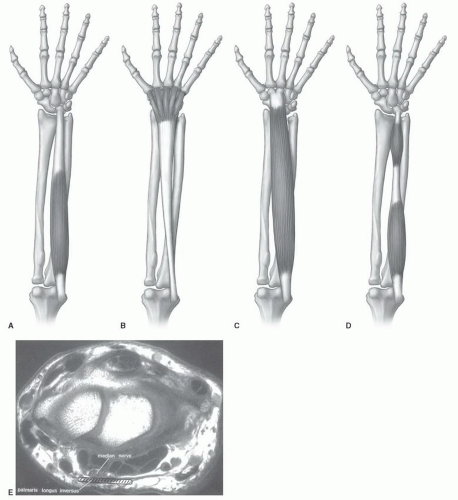
Muscle anomalies most commonly involve the abductor digiti minimi, palmaris longus, flexor carpi ulnaris, and flexor digitorum superficialis.96 Muscle anomalies are most often incidentally noted and do not cause symptoms.62,96
Table 11.4 Common Ossicles of the Hand and Wrist | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
aspect of the fifth proximal phalanx. Ulnar and median nerve symptoms have been associated with this anomaly (Fig. 11.39B).56,82,96
infection. Also, confusion of tenosynovitis with a ganglion can occur. Most often, the common flexor tendon sheath ends in the mid palm (71.4% of the population). The digital sheaths in the fingers do not usually communicate with the common flexor tendon sheath.56
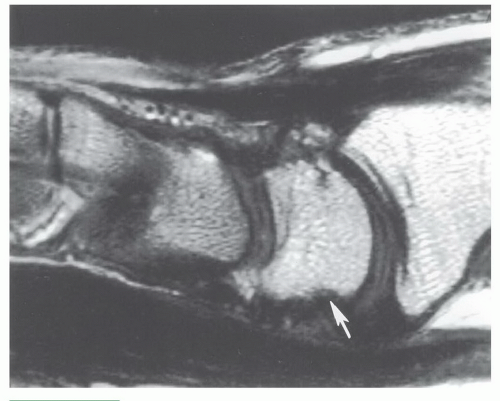 Figure 11.35 Sagittal T1-weighted image demonstrating volar irregularity of the lunate (arrow) due to normal ligament attachments. |
Table 11.5 Muscle Variants of the Hand and Wrist | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||
 Figure 11.36 Coronal gradient-echo image demonstrating an elongated ulnar styloid with faint signal intensity increase (arrow) due to a partially fused lunula. |
in imaging other conditions in the hand and wrist. However, experience is still evolving in these areas.27,43,118,119,120
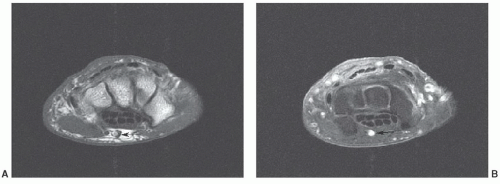 Figure 11.38 Axial T1-weighted (A) and post-contrast fat-suppressed T1-weighted (B) images demonstrating a persistent median artery (arrow). |
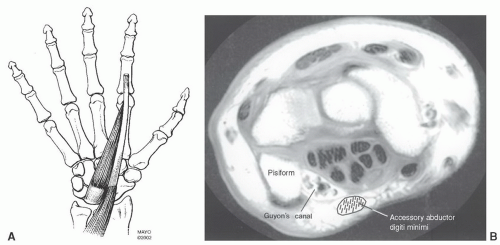 Figure 11.39 A: Accessory abductor digiti minimi. B: Axial MR image demonstrating the relationships of the muscle to Guyon’s canal. Normally, there is no muscle in this region. |
include incomplete fractures, complete fractures, physeal fractures, stress fractures, and bone bruises.21,128,130,132,133
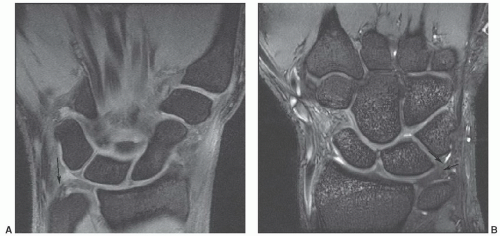 Figure 11.42 Coronal DESS images at 1.5 T (A) and 3.0 T (B) demonstrating intermediate to increased signal near the ulnar attachment of the triangular fibrocartilage in normal asymptomatic patients. |
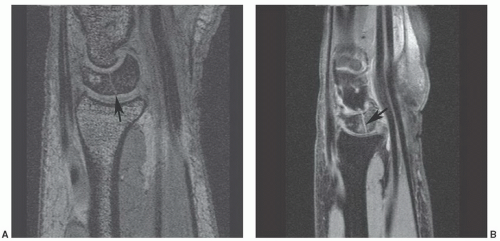
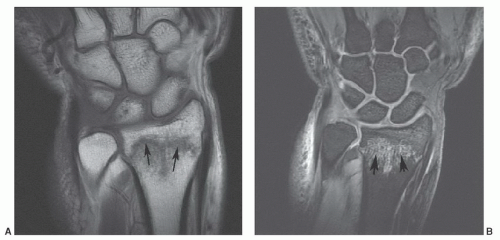 Figure 11.43 Distal radial fracture. Coronal T1- (A) and sagittal DESS (B) images demonstrate an undisplaced distal radial fracture (arrows) with marrow edema. |
carpal bone in adults and children. However, in children, scaphoid fractures account for only 2.9% of hand and wrist fractures. In adults, scaphoid fractures most commonly involve the waist, while in children the distal third is the most common fracture site (Fig. 11.44).134,138 Fractures of the triquetrum are the second most common carpal fracture followed by the capitate (Fig. 11.45) and lunate (Fig. 11.46).7,134
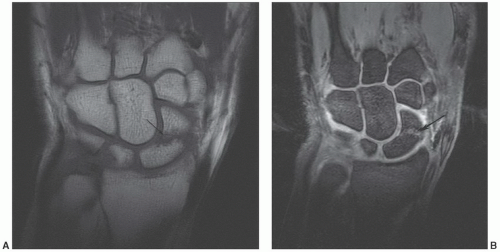 Figure 11.44 Scaphoid fracture. Coronal T1- (A) and DESS (B) images demonstrating a scaphoid waist fracture (arrow). |
important for the scaphoid (Fig. 11.48). Sagittal image planes aligned with the scaphoid are important to exclude “hump back” deformity.7
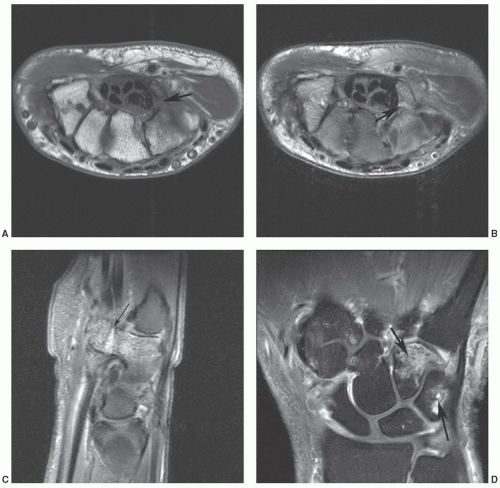 Figure 11.47 Hook of the hamate fracture with associated bone contusion in the triquetrum. Axial T1- (A) and axial (B) and sagittal (C)
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|