Patellofemoral Syndrome: Proximal Realignment
Patient Presentation and Symptoms
The most common symptom is anterior knee pain accentuated by stair climbing or walking up an incline surface. Female patients are more common than male, and the average age at initial presentation is 18 years, although the pain can occur in any age group. The second symptom is instability of the knee associated with patellar dislocation. This also tends to occur in the younger population (ages 13 through 25 years).
Indications
The patient complains of anterior knee pain or instability with associated malalignment of the patella on a Merchant-type patellar x-ray.1
Contraindications
Stage IV (Outerbridge) chondromalacia changes of the patellar surface (usually medial facet) do not respond well to realignment. The abnormal surface is placed in contact with the sulcus of the femur and may even lead to an increase in anterior pain.
Physical Examination
The physical examination demonstrates lateral tracking (the J sign) or frank dislocation of the patella as the knee comes into full extension with an increase of the Q angle above 20 degrees. The medial and lateral facets of the patella are usually tender to palpation.
Diagnostic Tests
The primary tests are roentgenographic. The Merchant x-ray is taken with the knees flexed about 30 degrees, and the beam projects from proximal to distal with the cassette held above the feet.1 The Laurin view is another common x-ray taken with the beam projecting from distal to proximal.2 Magnetic resonance imaging (MRI) or computed tomography (CT) scan of the patellofemoral joint can also illustrate the malalignment; however, all of the techniques are dependent on the degree of flexion of the knee at the time of the examination. It is easier to control and rapidly check the position of the knee with simple x-ray techniques.
Special Considerations
Proximal realignment does correct the anatomic changes on the proximal side of the patella but does not direct any attention to the tubercle insertion, which may be externally rotated.
Preoperative Planning and Timing of Surgery
The realignment can be performed before the growth plates are closed in the adolescent knee. In the setting of the dislocating patella, if the knee has had two or more dislocations despite exercises and bracing, the proximal surgery is indicated. The procedure is most successful when there is minimal abnormality to the distal insertion of the patellar ligament (no marked external rotation of the tubercle).
Special Instruments
Because early motion is necessary to avoid extension and flexion contractures, nonabsorbable sutures, such as zero Ethibond (Ethicon, Somerville, NJ), are best for the advancement of the vastus medialis.
Anesthesia
The procedure can be performed under epidural, spinal, or general anesthesia. The quadriceps muscle should be paralyzed during the time period when the elevation of the lateral patellar facet is evaluated.
Patient and Equipment Positions
The patient is placed in the supine position with the ipsilateral hip and pelvis elevated slightly by a cloth bolster so that the anterior knee is directed straight upward toward the ceiling of the operating room. This position stops the lower leg from externally rotating on the operating room table and gives easier access to the lateral side of the patella.
Surgical Procedure
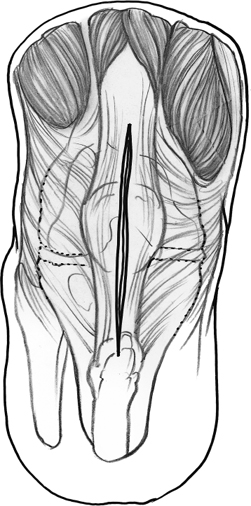
- A midline incision (Fig. 50–1) with some elevation of medial and lateral flaps is followed with a median parapatellar arthrotomy. The arthrotomy is initiated just below the lower pole of the patella and taken proximally for 10 to 12 cm along the quadriceps tendon, leaving 2 mm of the tendon with the vastus medialis muscle.
- The lateral arthrotomy incision is made 1 cm lateral to the lateral edge of the patella. The release begins just above the lateral joint line, avoiding any injury to the lateral meniscus, and is taken proximally through the synovium, dividing the superolateral geniculate and proceeding along the anterior margin of the muscle belly of the vastus lateralis for about 3 or 4 cm.
- The synovium is cleared from the posterior surface of the vastus medialis. Then, the muscle is advanced across the anterior surface of the quadriceps tendon and the patella to the edge of the lateral release incision.
- A nonabsorbable figure-of-eight suture is used to approximate the advanced muscle to the lateral margin. The muscle is advanced distally and laterally until the lateral facet of the patella is lifted upward from the lateral femoral condyle 1 cm with the knee in full extension. This elevation can be precisely controlled and measured. Once the desired lift-off is obtained, no further distal advancement is necessary.
- The vastus medialis is then sutured to the lateral margin of the lateral release from distal to proximal, closing the quadriceps tendon as a “tube” (Fig. 50–2).3,4
- The subcutaneous tissues and skin are closed in the standard fashion.
- There are two other techniques for proximal realignment that are similar to the tube realignment surgery.5,6 In the first variation the vastus medialis muscle is advanced across the anterior surface of the patella with or without a lateral release (Fig. 50–3). The tendon edge of the muscle is closed proximally along the anterior surface of the quadriceps tendon. This technique does not permit as much correction as the tube realignment. In the second variation the proximal realignment is performed in conjunction with the lateral release and the muscle is advanced across the anterior surface of the patella but not completely over to join the cut edge of the lateral release. This approach is similar to the tube realignment but also does not permit as much correction (Fig. 50–4).
- The lateral arthrotomy incision is made 1 cm lateral to the lateral edge of the patella. The release begins just above the lateral joint line, avoiding any injury to the lateral meniscus, and is taken proximally through the synovium, dividing the superolateral geniculate and proceeding along the anterior margin of the muscle belly of the vastus lateralis for about 3 or 4 cm.
Dressings, Braces, Splints, and Casts
The knee is placed in an immobilizer for the first 5 days. The dressings can be changed for comfort and showers. Crutches are used for stability for the first 1 or 2 days and are then discontinued to encourage full weight bearing as tolerated.
Tips and Pearls
The advancement of the vastus medialis should be done sequentially. As the medialis is advanced distally and laterally, the lateral patellar facet should gradually lift off from the lateral femoral condyle (Fig. 50–5). Each suture makes a significant change. The lift-off should be measured with the knee in full extension; that is, not in flexion or hyperextension. Attempts to save the superolateral geniculate vessel are futile, and even if it is entirely preserved during the surgical procedure, it will not be functional after surgery. The synovium should be divided on the lateral side as part of the lateral retinacular release because it can lead to failure of the correction and recurrent malalignment. Although it is theoretically possible to advance the medialis too far, the author has not seen a patella that dislocates medially after a proximal realignment. This overcorrection can be avoided by checking the tracking of the patella throughout the full range of motion before closing the knee.
Pitfalls and Complications
The incision into the quadriceps tendon must leave at least 2 mm of the tendon with the vastus medialis muscle. Without the tendinous margin, the muscle advancement can tear out and the instability can recur very soon after the surgery. If the lateral release is performed more than 1 cm lateral to the lateral side of the patella, there may be enough soft tissue on the lateral side to sew to the medialis without firming up the lateral capsule and without lifting up the facet at all. This emphasizes the importance of checking the facet elevation before closing the knee.
Postoperative Care
- The knee is placed in an immobilizer and the patient is discharged. Full weight bearing as tolerated with crutches is permitted.
- The dressing can be removed immediately, and motion is begun about 5 days after surgery.
- Progressive resistive exercises are started 5 to 6 weeks after the surgery when the knee should have full range of motion.
- By 4 months after surgery, the knee effusion should resolve.
- The quadriceps strength has increased to 90% of the opposite normal side.
- Sports activities can be started when the knee effusion has completely resolved and the quadriceps strength has increased to 90% of the opposite normal side.
- A patellar cutout brace is recommended for all sports activities until 1 year after the surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








