Patellofemoral Syndrome: Anteromedialization of the Extensor Mechanism
Patient Presentation and Symptoms
Patellofemoral problems are ubiquitous, and they are not isolated to only young or athletic individuals. Patellofemoral patients usually present insidiously. The symptoms progressively worsen and are aggravated by activities such as stair climbing, bicycle riding, and other activities that apply stress to the patellofemoral joint. There can be an effusion, but it is not always present. Commonly, clicking, popping, or an increasing amount of crepitance within the patellofemoral joint is noted.
Indications
Patients with patellofemoral subluxation and symptomatic distal and/or lateral articular lesions that are unresponsive to conservative management
Contraindications
- Patients with significant proximal patellar articular surface damage
- Tricompartmental arthritis
- Medial trochlear groove irregularities
- Smokers and excessively obese patients
Physical Examination
- Examine the entire lower extremity. Pes planus, hyperpronation, genu varum, or genu valgum can aggravate patellofemoral symptoms.
- Evaluate the lateral retinaculum. Lateral retinacular nerve irritation or inflammation is often overlooked and can sometimes be easily treated.
- Determine site of joint irregularity by examining the knee through the entire range of motion. More proximal lesions are painful further in flexion. Distal lesions (which are best treated with this procedure) are symptomatic in early flexion.
- Evaluate quadriceps strength and flexibility with emphasis on the vastus medialis oblique (VMO).
- Iliotibial band tightness with consequent lateral retinacular tightness should be evaluated with the Ober test.
Diagnostic Tests
- Standard radiographs are appropriate including weight-bearing anteroposterior (AP) x-rays, a true knee lateral view, and an axial Merchant view (maximum 30 to 45 degrees of knee flexion).
- Computed tomography (CT) scans are not necessary but can be helpful in difficult cases.
- Magnetic resonance imaging (MRI) demonstrates plical bands and effusions but is also not necessary.
- Bone scans are helpful but also not necessary in most cases.
Special Considerations
Complete diagnosis and treatment are necessary. When ligamentously lax individuals are being treated, special care to work on muscle tone and external support for the patella is warranted. This often includes the use of orthotics with arch supports and medial posting as well as patellar buttress braces.
Preoperative Planning and Timing of Surgery
Physical therapy is appropriate in almost all instances as the first line of treatment for these patients. Multiple different approaches are possible and vary according to therapist and patient. Coordinated hamstring and quadriceps firing must be achieved. This is done after range of motion and stretching establishes normal patellofemoral mechanics and a reduction in the irritation of the joint. Patellar bracing and taping can be helpful. Prone quadriceps mobilization after warm-up is essential. In addition to these more traditional therapeutic steps, we have placed an increased emphasis on hip rotator strengthening and core stability. Adding this into the early regime has made both conservative and operative care of these patients more successful.
The patellofemoral articulation has different configurations that may cause problems. The classification scheme by Schutzer et al.1 divides these configurations into three categories: (1) patellar tilt only, (2) subluxation of the patella as defined by the patellar apex plane slightly lateral to the nadir of the trochlear groove, and (3) patellar tilt and subluxation. Treatment of patellar tilt may be a soft tissue procedure such as a lateral retinacular release. When there is subluxation, medial repair, arthroscopically or open, is indicated. In some situations, soft tissue procedures as well as tibial tubercle transfers may be required.2
Special Instruments
In addition to standard arthroscopy and open surgical instruments, we utilize anteromedialization Tracker instruments (Depuy Inc., Indiana). These allow the osteotomy angle to be preset prior to it being performed. The set also includes a large, flat retractor that can be placed behind the posterolateral corner of the tibia to protect neurovascular structures. A sagittal saw and a set of osteotomies are used to perform the osteotomy.
Anesthesia
Although the procedure can be performed under spinal or epidural anesthesia, we suggest to patients that general anesthesia is more appropriate. This reduces the anxiety associated with the noise and vibration of the sagittal saw. Postoperative femoral nerve blocks for patients requesting it or when recovery room pain is not easily controlled are often helpful.
Patient Position
Anteromedialization procedures are performed with the patient in the supine position. The preosteotomy arthroscopy can be done with or without an arthroscopy leg holder and is determined by the amount of intraarticular work that is necessary. Taking the patient out of the hemilithotomy position and out of the leg holder without reprepping has not been an issue for us.
Surgical Procedure
Patients who fail conservative management may be brought to the operating room. At the time of arthroscopy, the location of patellofemoral disease can be identified arthroscopically. Patients who have proximal medial patellar irregularities or significant medial trochlear lesions must be identified, as proceeding with an isolated anteromedialization procedure is unwarranted in these situations. If the patellar wear is on the distal patellar surface and minimal trochlear wear exists, an anteromedialization is often beneficial. Meniscal pathology as well as chondral damage is more easily treated prior to making a skin incision and is therefore completed arthroscopically. Chondroplasty, where appropriate, is performed as well as microfracture in areas of exposed bone. We do not, however, recommend performing microfracture of the patellar surface itself.
The anteromedialization procedure is described below and should be modified to address irregularities within the joint. Anteromedial tibial tubercle transfer (anterome-dialization) is predominantly a technique to realign when unloading is also indicated.
Osteotomy Technique
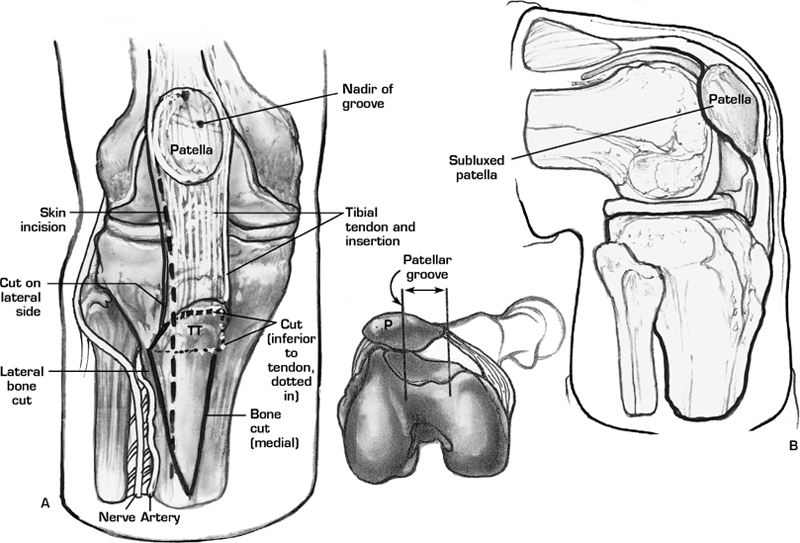
- Skin incision: midpatella to 4 to 5 cm distal to tibial tubercle (Fig. 51–1A)
- Deep incision: lateral retinacular release to vastus lateralis muscle
- Expose posterolateral corner of tibia to allow protection of neurovascular structures by carefully reflecting anterior tibialis muscle
- Isolate patellar tendon and mark the anteromedial aspect of the tibial tubercle
- Choose angle of osteotomy: standard cut to establish both anteriorization and medialization (Fig. 51–2)
- Steeper osteotomy for treatment of chondral irregularities (i.e., more anteriorization) (Fig. 51–3A)
- Predrill osteotomy using Tracker or external fixator guide as desired and cut with a sagittal saw.
- A steeper osteotomy may require back-cut on posterolateral surface for neurovascular structure protection (Fig. 51–3A)
- Angle proximal coronal cut to avoid bony impingement as tubercle is elevated (Fig. 51–2C)
- Create stress riser at the distal end of the osteotomy (taper distal osteotomy to anterior tibia).
- Slide the tubercle along the osteotomy plane to the desired location (Fig. 51–4).
- Secure with two bicortical screws using the lag technique and countersinking (Fig. 51–4B).
- No need to close anterior compartment
- Skin is closed in a layered fashion.
Dressings, Braces, Splints, and Casts
At the conclusion of the procedure, we immobilize the leg in a long leg immobilizer over a well-padded postoperative dressing. Patients remain non–weight bearing until their first follow-up visit. Once sutures are removed, daily range-of-motion exercises are begun, but otherwise the brace is worn at all times for 6 weeks.
Tips and Pearls
The patellofemoral joint remains a source of significant pain for patients and enigma for many surgeons. Careful diagnosis of all mechanical and anatomic issues relating to a patient’s patellofemoral problem preoperatively helps increase the rate of successful outcomes. However, even more importantly, once surgical intervention is decided on, addressing all associated problems is imperative.
Two commonly encountered problems are the overutilization of lateral releases and the lack of care for full-thickness trochlear lesions. A lateral release functions primarily to correct problems associated with patellar tilt and not subluxation. A lateral release performed on a hypermobile or postdislocation patient often fails. Trochlear lesions are most accurately diagnosed at the time of preosteotomy arthroscopy. When seen they should be treated by marrow stimulating or cartilage preservation procedures. The long-term results of an isolated anteromedialization when a trochlear lesion exists have not been as rewarding as for isolated patellar lesions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








