Chapter 11 Orthoses for osteoporosis
Pathophysiology of osteoporosis
An understanding of the potential role of orthotic management of vertebral compression fractures (VCFs) begins with an understanding of osteoporosis itself. Osteoporosis is a disorder in which mineralized bone density is below normal, resulting in a bone structure that is vulnerable to fractures. The compromised bone structure is characterized by a reduction in bone mass that is related to an imbalance in bone formation and resorption. Osteoporosis is the most common of the metabolic bone diseases described as osteopenia, meaning “too little bone.”11 A decrease in bone mass normally begins in a person’s early thirties and continues throughout life. Osteoporosis is defined as a bone mineral density greater than 2.5 standard deviations below the young adult mean for normal bone mineral density. It results from an imbalance in bone turnover such that the amount of new bone production cannot keep up with the amount of bone resorption, that is, bone resorption is greater than bone deposition.
The majority of primary osteoporosis can be described as type I or type II. Type I affects women and is associated with estrogen deficiency occurring 5 to 10 years after menopause (Table 11-1). Trabecular osteogenesis is primarily affected and results in a diminished capacity to support compressive loads. As a result, vertebral bodies, the distal radius, and the hip are common sites at greater risk for fractures. Type II osteoporosis affects both males and females. It is due to calcium deficiency and is associated with aging. In type II osteoporosis, both trabecular and cortical bone are affected. Because cortical bone provides support, especially for bending and torsional loads, the femoral neck, proximal tibia, humerus, pelvis, and vertebral bodies are at higher risk for fractures.
Table 11-1 Classification of osteoporosis
| Classification | Clinical course | Remarks |
|---|---|---|
| Primary | ||
| Involutional | ||
| Type I (postmenopausal) | Affects women only within menopause, lasts 15–20 yr | Predominantly trabecular bone loss in axial skeleton |
| Type II (age-associated) | Men or women > 70 yr | Proportional loss of trabecular and cortical bone |
| Idiopathic juvenile | Age 8–14 yr, self-limited (2–4 yr) | Normal growth; consider secondary forms |
| Idiopathic young adult | Mild to severe, self-limited (5–10 yr) | |
| Secondary (type III) | ||
| Dependent on underlying cause | Usually reversible to some extent after treatment of primary disease | |
| Regional | ||
| Reflex sympathetic dystrophy | Three overlapping clinical stages: typical course lasts 6–9 mo, followed by spontaneous or assisted resolution | Radiographic changes may be seen in the first 3–4 wk as patchy demineralization of affected area; triple-phase bone scan shows increased uptake in involved extremity before radiographic changes; brief tapering dose of corticosteroids often warranted |
| Transient regional osteoporosis | Localized, migratory, predominantly involves hip, usually self-limited (6–9 mo) | Rare; diagnosis by clinical suspicion, radiograph, and bone scan; treatment similar to that for reflex sympathetic dystrophy |
From O’Young BJ, Young MA, Stiens SA, editors: Physical medicine and rehabilitation secrets, ed 2, Philadelphia, 2002, Hanley & Belfus.
Osteoporosis is a significant public health problem, with 100 million people at risk worldwide and 28 million people at risk in the United States alone.21 An estimated 1.5 million fragility fractures occur annually, including 700,000 spine, 300,000 hip, 250,000 wrist, and 250,000 other fractures related to osteoporosis. Even more compelling is the economic cost associated with osteoporotic fractures. In 1995 the United States spent over $13.8 billion on hospital and nursing home direct costs ($38 million daily). Projected expenditures for 2030 are more than $60 billion, or $164 million per day.36 More than 260,000 patients with a first-time symptomatic VCF are diagnosed each year. There are more than 150,000 hospitalizations per year, with an 8-day average stay and $12,300 average charge.37 Typically, there are 14 hospital bed days per VCF, which is comparable to the 18 hospital bed days for hip fractures. Moreover, there is increased long-term morbidity and mortality in patients with VCF.13
VCFs can present with acute pain, or they can be silent and have no associated pain. Nearly one third of the latter patients will experience chronic pain.5 A large percentage of cases go undiagnosed. VCFs typically are caused by falls, but they may result from something as innocuous as a cough or sneeze. The risk for VCFs is amplified as these events occur in the presence of compromised bone integrity. Eighty-four percent of patients with radiographic evidence of VCF report associated back pain. VCFs lead to progressive sagittal deformity (hyperkyphosis), and the changes in spinal biomechanics increase the risk of further fractures in the vertebrae above or below the fracture site.24
Hyperkyphosis is a common postural deformity secondary to VCF. The degree of kyphosis correlates with physical function and mobility (independent of pain), pulmonary function, mental well-being, and risk of new fractures.14,27,35 Lung function in patients with thoracic and lumbar VCFs is affected and leads to increased mortality.39 Hyperkyphosis can lead to ligamentous stretching, diminished functional vital capacity, inferior costal margin and pelvic rim contact and discomfort, chronic low back pain, abdominal crowding, depression, muscle imbalance, and painful, chronic intravertebral pseudarthrosis. In the case of muscle imbalance, the kyphotic deformity progressively elongates the paraspinal muscle extensors and leads to overall muscle weakness. Involutional muscle loss, called sarcopenia, is common in the elderly and can be an important factor contributing to muscle weakness.9,38,47 The severity of the VCF and associated pain can lead to diminished function, decreased mobility, physical deconditioning, and consequently accelerated bone loss.
Clinical signs of VCF include sudden onset of back pain with little or no trauma,23 loss of height, spinal deformity (dowager’s hump), protuberant abdomen, and diminished vital capacity. In patients with thoracic or lumbar VCF, lung function (forced vital capacity, forced expiratory volume in 1 second) is significantly reduced. One thoracic VCF causes 9% loss of vital capacity.26 A prospective study of 9575 women followed for more than 8 years demonstrated that patients with VCF have a 23% to 34% increased mortality rate compared to patients without VCF. The most common cause of death is pulmonary disease, including chronic obstructive pulmonary disease (COPD) and pneumonia (hazard ratio 2.1).21
VCFs and their secondary effects remain a constant challenge for the medical team and should be addressed as quickly as possible. In particular, strategies addressing postural deformity reduction should be a major orthotic consideration because a person’s ability to function on a daily basis can be dramatically improved and pain medication reduced.
Historical perspective
Treatment of osteoporosis is divided into pharmacologic, nonpharmacologic, and surgical options that address either the acute pain from a recent VCF or the chronic pain that may follow.45 The distinction is essential because the treatment goals, methods, and timeline are different for each category. Historically, for orthotic treatment, it appears that devices originally intended for acute pain have been used often for chronic pain. This situation has contributed to disappointing failures of orthotic treatment of VCFs from osteoporosis and should be avoided.
Much interest has focused on developing effective pharmacologic treatments to reduce bone loss, which is the hallmark of osteoporosis and the primary underlying cause of fractures. Options include drug therapies such as bisphosphonates to decrease bone resorption, estrogen/hormone replacement to counteract the postmenopausal increased rate of bone loss, and calcitonin to reduce osteoclastic bone resorption.21 However, the efficacy of pharmacologic treatments in reducing the risk of falls, fractures, and skeletal deformities is unclear and “should not be overrated.”45
The primary types of nonpharmacologic treatments of osteoporosis include exercise, physical management of pain, orthotic treatment, and gait training.45 The goals are to reduce the rate of bone resorption, improve the strength of bone, and enhance the overall quality of life. Improving muscle strength, especially in the lower extremities, can reduce the risk of falls.28 There is general agreement that preventing fractures is preferable to treating the complications that may arise from them. Thus, prevention programs, including screening for osteoporosis, are now being emphasized.6
As a consequence of diminished bone strength, many patients with acute VCFs from osteoporosis are not candidates for spinal fusion, and less invasive procedures such as vertebroplasty and kyphoplasty have been developed.20 These procedures can relieve pain and stabilize the fracture, but the long-term benefits in preventing additional fractures are not well understood.10
Orthotic management of VCFs from osteoporosis is used as part of nonpharmacologic treatment. Few studies have investigated the efficacy of specific orthotic interventions in spinal osteoporosis.16,17,32 Thus, there is a substantial need for research addressing this issue. Traditional orthotic approaches (e.g., three-point bending orthoses) have concentrated on preventing excessive spinal flexion to reduce pain from VCFs. These orthoses do not substantially correct the anteroposterior standing imbalance that often is present, nor do they provide stability in the transverse plane. However, correcting standing posture has been found to be a more fruitful approach.12
Current issues
Prevention of osteoporotic vertebral compression fractures
Osteoporosis often goes undiagnosed until after the first painful fracture occurs. At that point, attention is focused on resolving the acute pain and returning the patient to the activities of daily living, which can be an expensive undertaking. Given that preventing a fracture is preferable to treating one, screening for osteoporosis is an important consideration for the patient. Although opinions vary on the value of screening for osteoporosis based on bone mineral density measurements alone,2,8 there is general agreement that taking steps such as exercising more, increasing calcium intake through dietary and/or pharmacologic means, smoking cessation, and lowering alcohol consumption help to prevent bone degradation.6
Efficacy of treatment options
Sinaki et al.45 reported several studies on nonpharmacologic treatment of vertebral fractures. Nonpharmacologic treatment is intended to relieve pain and return function to the patient. It may include exercise, orthotic management, and gait training. Orthotic management options are limited, and few studies on the effectiveness of specific orthoses have been reported.
Pharmacologic treatment of osteoporosis is intended to treat pain and to slow or reverse the progression of disease.21 Calcitonin and bisphosphonates inhibit osteoclasts and slow bone resorption. Several substances have been shown to increase bone mass, including sodium fluoride, anabolic steroids, testosterone, and parathyroid hormone. However, they may have serious side effects if not used correctly. For pain control, the choices are nonsteroidal antiinflammatory drugs and opioids. Possible side effects of opioids that may compromise orthotic management include drowsiness and dizziness.
Augmentation of VCF with bone cement has emerged as a minimally invasive surgical treatment for patients who have not responded to other therapies. There are two distinct procedures: vertebroplasty, in which bone cement is percutaneously injected into the fractured vertebral body to stabilize it but does not correct the deformity, and kyphoplasty, in which bone cement is injected after percutaneous reduction of the vertebral body deformity using inflatable bone tamps (balloons). The goals of these treatments are to reduce pain and to restore the normal weight-bearing function of the spine so that the risk of future fractures is reduced.10,33
Vertebroplasty can result in pain reduction, but it does not correct spinal alignment, and complications are associated with cement leakage. Increased risk for new VCFs has been reported after vertebroplasty.24 The excessive kyphosis leads to increased forward bending moments, which can lead to paraspinal muscle fatigue and increased strain at the facet capsules, contributing to chronic pain. Some patients attempt to improve standing posture by flexing their knees to counterbalance the increased forward bending moments. However, this can lead to muscle contractions, impaired gait velocity and balance, and increased risk of falls. The presence of two or more VCFs can increase the risk of hip fractures, independent of bone mass. In contrast, kyphoplasty can reduce the vertebral deformity and restore normal spinal alignment, but it requires more surgical expertise and is much more expensive.
Current research
Pharmacologic treatment studies
Improving pharmacologic treatments of osteoporosis is a topic of ongoing research. Variability in the response to pharmacotherapy makes difficult the prediction of success or failure in an individual patient. Moreover, the outcome of pharmacologic treatment may not be known for years. The emerging field of pharmacogenomics of osteoporosis aims to use genetic information to predict the outcomes of pharmacologic treatments and could lead to new drug therapies for osteoporosis.31
Surgical treatment of vertebral compression fractures from osteoporosis
Several studies have reported on the risk of adjacent fractures after vertebroplasty and kyphoplasty. This risk is significantly increased in patients with severe secondary osteoporosis and is greater in the first 30 to 60 days after both vertebroplasty and kyphoplasty.24 However, the available studies do not allow definite conclusions because of the lack of good-quality prospective randomized trials. As a result, the potential therapeutic benefits of vertebroplasty and kyphoplasty procedures in altering the fracture risk in adjacent, nonaugmented vertebral bodies are not well known.
A well-recognized risk factor for adjacent fracture is the kyphotic deformity24 consisting of vertebral deformity of the fractured vertebra caused by a loss of anterior height and regional kyphotic deformity that contributes to increased forward bending moments. The reported percentage of vertebral kyphosis reduction ranges from 39% to 65%,22,34 whereas the restoration of vertebral body height ranges from 35% to 68%.7,11 Spinal extension inducing “postural reduction” of VCFs also has been reported. In a prospective study of 41 consecutive patients with 65 VCFs who underwent vertebroplasty, McKiernan et al.29 achieved improvement of kyphotic deformity in 23 fractures using spinal extension. In a prospective clinical study, Kim et al.18 described the ability of postural reduction to achieve significant correction of anterior vertebral body height and vertebral kyphotic deformity in 90% of patients with acute VCFs of onset less than 8 weeks.
A cadaveric study showed that spinal extension was effective in recovering the anterior height loss.10 However, the middle height of the fractured vertebra was better restored by balloon inflation. The combination of balloon inflation and extension resulted in improved correction of both the vertebral and segmental kyphotic deformities, better than achieved with individual modalities alone. Therefore, based upon knowledge gained by studying vertebroplasty and kyphoplasty, spinal orthoses may have a role in postural reduction of VCF deformity. They also may prove useful as an adjunct to vertebroplasty and kyphoplasty. This finding supports further clinical studies assessing the efficacy of spinal orthotic devices in the treatment of osteoporotic VCFs.
Treatment recommendations
Posture training support
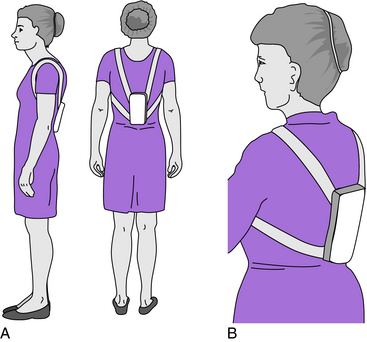
The posture training support (PTS) is one of two spinal orthoses for osteoporosis that have any scientific study supporting or refuting their efficacy.17,45 The PTS, called a “weighted kypho-orthosis,” provides a weight suspended just inferior to the scapulae (Fig. 11-1). The weight can be increased to as much as 2.5 lb in several increments. Patients are encouraged to try different levels of weight to determine which is most effective. Too much weight will not benefit the patient, and compliance will suffer.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree