Chapter 9 Orthoses for spinal deformities
Scoliosis
Pathophysiology and natural history
Scoliosis can be defined as a lateral curvature of the spine, greater than 10 degrees as measured by the Cobb method.36 Because lateral curvature of the spine is typically associated with vertebral rotation within the curve, a three-dimensional deformity occurs. There is coronal plane translation of a series of vertebrae away from midline; transverse plane deformity by way of vertebral rotation in relation to each other because of the nature of the intervertebral articulations of the posterior elements132; and, more commonly in idiopathic thoracic curves, an anterior translation in the sagittal plane, resulting in a hypokyphotic, or even lordotic relationship of the effected vertebrae.45 A host of terms is used to describe the various types of scoliosis (Table 9-1)78
Table 9-1 Glossary of terms describing different types of scoliotic curves
| Term | Definition |
|---|---|
| Adult scoliosis: | Spinal curvature present after skeletal maturity. It may be due to any cause. |
| Cervicothoracic curve: | Any spinal curvature in which the apex is at C7 or T1. |
| Compensatory curve: | A secondary curve located above or below the structural component that develops in order to maintain normal body alignment. |
| Congenital scoliosis: | Scoliosis due to bony abnormalities of the spine that are present at birth. These anomalies are classified as failure of vertebral formation and/or failure of segmentation. |
| Double curve: | Scoliosis in which there are two lateral curves in the same spine. |
| Double major curve: | Scoliosis in which there are two structural curves that usually are of similar size and rotation. |
| Double thoracic curve: | Scoliosis with a structural upper thoracic curve, a larger, more deforming lower thoracic curve, and a relatively nonstructural lumbar curve. |
| Hysterical scoliosis: | A nonstructural deformity of the spine that develops as a manifestation of a psychological disorder. |
| Idiopathic scoliosis: | A structural curve for which the cause has not been definitely established. |
| Kyphoscoliosis: | Noted as an increased round-back on the lateral radiograph, the condition may represent a true kyphotic deformity (as seen in some pathologic conditions) or it may represent such excessive rotation of the spine that the lateral radiograph is actually reflecting the scoliotic deformity. (In idiopathic scoliosis, true kyphotic deformity does not occur.) |
| Lordoscoliosis: | Structural scoliosis associated with increased swayback or loss of normal kyphosis within the measured curve; nearly always present in idiopathic scoliosis. |
| Lumbar curve: | A spinal curvature in which the apex is between L1 and L4. |
| Lumbosacral curve: | A spinal curvature in which the apex is at L5 or below. |
| Neuromuscular scoliosis: | Scoliosis due to a neurologic disorder of the central nervous system or muscle. |
| Nonstructural (functional) curve: | A curvature that does not have a fixed deformity and may be compensatory in nature. The curve may be a result of leg length discrepancy (and so disappears when the patient is supine), poor posture, muscle spasm, or other cause. |
| Primary curve: | The first or earliest curve present. |
| Structural curve: | Represents a segment of the spine that has a fixed lateral curvature. |
| Thoracic curve: | A spinal curvature in which the apex is between T2 and T11. |
| Thoracolumbar curve: | A spinal curvature in which the apex is at T12, L1, or the T12-L1 interspace. |
Idiopathic scoliosis
Idiopathic scoliosis (IS), termed as such because of the unknown cause or etiology of the deformity, is the most common form of scoliosis. A thorough physical examination by a qualified physician, including a radiographic analysis to rule out numerous potential differential diagnoses, is required to make the diagnosis. The type of IS is defined by the age of onset.83 If a scoliosis is recognized in patients less than 3 years of age, it is considered infantile idiopathic scoliosis. A scoliosis detected between the ages of 3 and 10 years of age is considered juvenile idiopathic scoliosis. The most common form of idiopathic scoliosis is adolescent idiopathic scoliosis (AIS) and is termed as such when the curve is detected after age 10 years but prior to skeletal maturity. A scoliosis that is detected after skeletal maturity is termed adult scoliosis. More recently, however, due to the relationship that exists between the rate of spinal growth and the progression of deformity, the terms early-onset idiopathic scoliosis (EIS) and late-onset idiopathic scoliosis (LIS) have come into favor. Even though scoliosis can develop at any age during growth, the two primary periods of rapid growth occur in the first few years of life and then again during the adolescent growth spurt. Mehta113 pointed out that the fastest rate of growth in children is in the first year of life, with a growth rate of 20 to 25 cm in those twelve months. This is nearly twice the growth rate of the adolescent growth spurt, where growth of 12 to 14 cm per year can be seen. An increase in height at the rate of 9 cm per year is considered a reasonable threshold to identify this peak period during adolescence.25 The increase in height during the second year of life (12 to 13 cm per year) is similar to the rate seen during the adolescent growth spurt. With regard to the specific growth velocity of the spine as measured between the T1 and L5 segments, it is greatest from birth to age 5 years, with marked deceleration between ages 5 and 10 years. Similarly, the onset of scoliosis between the ages of 5 of 10 is less common.43,48 For this reason, the term early-onset scoliosis has been used to reflect the presence of scoliosis prior to 5 years of age, including all possible etiologies, whereas the term late-onset scoliosis applies to scoliosis detected after age 5,44 and is most commonly associated with the onset of scoliosis that occurs just before puberty.
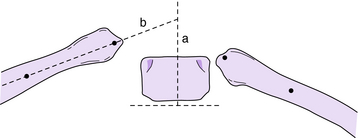
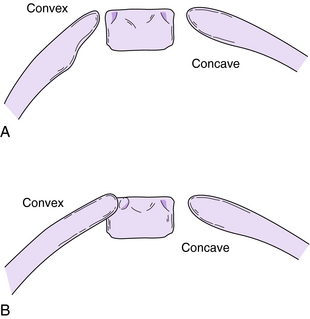
Some critical differences exist between the prognosis of patients with EIS and of those with LIS. EIS is diagnosed within the first 6 months of life in the majority of children,78 is seen more often in boys than in girls (with most having left-sided thoracic curve patterns),182 and has the capacity to spontaneously resolve in some patients.47,83,98,111,112 The most reliable indicators for differentiating resolving from progressive scoliosis are the rib-vertebra angle difference (RVAD), which is the angular difference between the concave and convex side ribs in relation to the apical thoracic vertebra, and the amount of apical vertebral rotation, as defined by Phase I and Phase II rotation as first reported by Mehta111 in 1972 (Fig. 9-1). A RVAD < 20 degrees indicates a high likelihood of curve resolution whereas curves with a RVAD of 20 degrees or greater are more likely to be progressive. A phase 2 relationship between the rib head and apical vertebra on the convex side implies that progression of the curve is almost certain (Fig. 9-2). In Mehta’s initial study, 46 of 86 patients with phase 1 curves resolved, and of those, 83% had a RVAD < 20 degrees. The average RVAD of those that progressed was 25.5 degrees (compared to 11.7 degrees in those that resolved); 84% had a RVAD of 20 degrees or greater. The usefulness of the RVAD was strongly supported by Ferreira et al.,57 who reported that 67 of 68 patients with resolving curves had a RVAD < 20 degrees, and all were classified as phase I. In 40 patients with progressive curves, 37 had a RVAD of 20 degrees or greater. Diedrich et al.47 reported on the long-term observation of resolving infantile scoliosis. In their study of 42 patients, 34 of whom were followed more than 25 years, 85% of those having a RVAD of less than 20 degrees had a resolving curve, whereas 90% of those who had a progressive curve had a RVAD of 20 degrees or more.
Pulmonary compromise is a much more significant concern in those diagnosed with EIS compared to those with LIS. This is because of the presence of a potentially progressive chest wall deformity associated with the scoliosis during the time in which the lungs are rapidly developing. There is a 10-fold increase in the number of alveoli between birth and adulthood, with the majority of this increase occurring during the first 8 years of life.53 There is also an increase in the number of respiratory branches, from 21 to 23, between the ages of 3 months and 8 years.49 The incomplete maturation of the lung and pulmonary vasculature has been reported as the primary reason for ventilation defects seen in patients with early-onset scoliosis.119 While the influence of compressive forces acting upon the lung tissue is still under investigation, there is an apparent correlation between the age of scoliosis onset and the diminished number of alveoli that develop. The most hypoplastic lungs are found in those with the earliest onset of EIS.24 The result can be a restrictive pattern of lung disease that includes reductions in vital capacity and total lung capacity. In children with EIS, the amount of vital capacity reduction is also influenced by the location and severity of the curve.67 This is unique to these young patients, as those with LIS demonstrate little or no reduction of vital capacity in response to the presence of their curve.119 Ultimately, patients with EIS who also demonstrate significant respiratory compromise due to the early age of onset and size of their curve are at greater risk for life-threatening respiratory failure at or before late middle age.24,131
Understanding the natural history of LIS is essential to clinical decision-making. This is true not only for determining when observation or treatment is indicated, but also for determining when treatment is effective. AIS is the most common form of idiopathic scoliosis, affecting 1.5% to 3.0% of children who are at least 10 years of age. Curves exceeding 20 degrees affect between 0.3% and 0.5%, and curves exceeding 30 degrees are found in 0.2% to 0.3% of adolescents.78 Curve progression is typically defined as a measured difference of 5 degrees or greater,100,167 however a 10-degree change has been reported as being required for 95% certainty that an observed change was not caused by measurement error alone, but is instead indicative of true progression.31
Less than 1% of children screened for scoliosis and less than 10% of those who are positively identified as having a curve of at least 10 degrees will require active treatment.165 The goal of an evaluating physician is to make an accurate diagnosis and to identify which patients are most likely to progress and thus require treatment, either with an orthosis or with surgery. When prescribed, the goal of the orthosis is to prevent further progression of a curve that would otherwise worsen if left untreated. Factors that have the most influence on whether or not a curve secondary to AIS will progress are patient gender, remaining growth, curve magnitude, and curve pattern.28,100,123
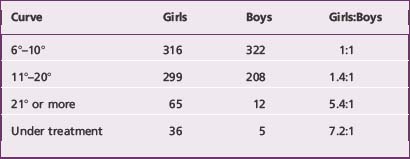
With respect to gender, the prevalence of AIS is similar in boys and girls with smaller curves, but girls are more likely to experience curve progression (Table 9-2).9,39,99,143 Boys with comparable curves have been estimated to have about one tenth the risk of curve progression as girls,165 however one report suggests the difference is less.86
Table 9-2 Prevalence of gender for idiopathic scoliosis as related to the severity of the curve in 1,222 subjects
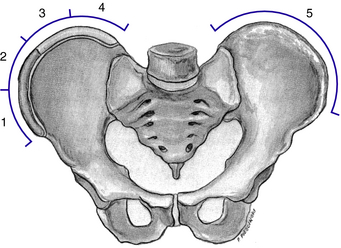
The amount of growth remaining is typically estimated by two maturity indices: the Risser sign and, in girls, the onset of menstruation; however the single most accurate indicator is to monitor growth. The Risser sign is a skeletal marker based on the ossification of the iliac apophysis.140 It is interpreted by viewing a standing posterior-anterior radiograph of the spine and pelvis, where ossification of the pelvis begins laterally and progresses medially until maturation (Fig. 9-3). The range of the Risser sign is from 0 to 5, with 0 indicating no ossification and 5 indicating a fully ossified ilium, which indicates skeletal maturity. A Risser sign of 0, 1, or, to a lesser extent, 2, is indicative of significant growth remaining, which can equate to a greater risk for curve progression in some patients with AIS. Some studies have questioned the usefulness of the Risser sign as a reliable measurement of skeletal maturity,15,81,96,97,150,152,184 including reports of differing interpretations on how the excursion of the iliac apophysis is scored.16,185 In girls, the onset of the menstrual cycle is a physiologic indicator that is helpful in estimating remaining growth. A premenarchal girl is most likely to be in a very active growth period, whereas after menarche, the girl enters the deceleration phase of growth where curve progression becomes less likely.
A third indicator of skeletal maturity, the peak height velocity, is more difficult to immediately assess than the Risser sign or menarchal status in girls, but it has gained greater recognition as a more accurate tool to assess the amount of growth remaining in the adolescent with idiopathic scoliosis. Peak height velocity (PHV) is calculated from changes in a patient’s height measurements over time, typically recorded in intervals no less than 4 and not more than 6 months. The average PHV for girls has been reported as about 8.0 cm per year and 9.5 cm per year for boys in the groups studied.25,54
Little et al.96 reported on the relationship of growth rates, as expressed in overall height velocities, to other maturity indicators in girls with AIS. The timing of peak height velocity, also known as peak growth age (PGA), was plotted against other maturity indicators, including chronological age, Risser sign, and menarchal status, to determine its usefulness as a prognostic tool for curve progression. PGA was found to have a stronger correlation with curve progression than any other maturity indicator (age, Risser sign, or menarchal status). The authors also cited the apparent relevance of the timing of PGA as related to curve size as a prognostic indicator of curve progression. Reporting on 88 of 120 girls who demonstrated progression of their primary curve despite being braced, 60 of these patients had a curve of more than 30 degrees at PGA, and in 50 (83%) of these 60 patients the curve progressed to 45 degrees or more. The remaining 28 patients had a curve of 30 degrees or less at peak height velocity, with only one curve (4%) progressing to 45 degrees or more. The authors suggested a significant relationship that exists between the size of a primary curve size, with 30 degrees as an important threshold, and the timing of PGA. Lastly, and of particular clinical interest, the median time in which PGA was achieved in this population was earlier than that of the median time of menarche and Risser 1 (Fig. 9-4). The usefulness of PGA as a clinical tool in boys with AIS has also been reported.152
The size of a curve at the time of detection combined with estimating the degree of maturity is very helpful in predicting the risk for progression in AIS. Lonstein and Carlson100 described the relationship between maturity and curve progression. In their review of 727 school-age children (575 girls, 152 boys), with initial curves of 5 to 29 degrees, they described three primary prognostic factors in predicting curve progression in a growing child: curve size, chronological age, and Risser sign. They reported that the younger the child, the lesser the Risser sign; and the larger the curve at discovery, the higher the likelihood for curve progression (Table 9-3). A scoliosis that reaches a magnitude of 25 degrees in an immature patient, even if detected during an initial visit, typically is considered a candidate for orthotic treatment.101,123
Table 9-3 Incidence of curve progression based on curve magnitude and Risser sign
| Percentage of Curves That Progressed | ||
|---|---|---|
| Risser Sign | Curves 5–19 Degrees | Curves 20–29 Degrees |
| Grade 0 and 1 | 22% | 68% |
| Grade 2, 3, or 4 | 1.6% | 23% |
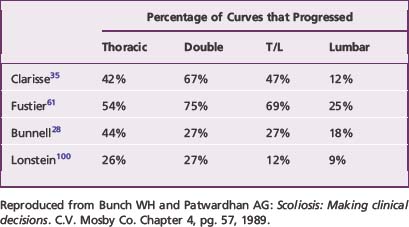
Natural history studies also have reported the usefulness of curve pattern in predicting curve progression. Opinion in the literature tends to agree that single lumbar and single thoracolumbar curves are the least likely to progress and are the most receptive to brace treatment. Compiling data from various natural history studies, Bunch and Patwardhan26 reported single thoracic and double curve patterns are more likely to progress (by as much as a factor of two) than single lumbar or single thoracolumbar curve patterns (Table 9-4).27,35,61,100
The natural history of scoliosis after skeletal maturity is reached is an important consideration in the context of appropriate use of orthoses during growth. Orthoses should be used in patients whose curve size and pattern would be both cosmetically acceptable and stable throughout adulthood if successfully stabilized with orthotic management during growth. Weinstein and Ponseti167 reported on a series of 102 untreated scoliosis patients representing 133 curves with available radiographs, with an average follow-up of 40.5 years. Sixty-eight percent of the curves progressed after skeletal maturity. Curves that were less than 30 degrees at skeletal maturity tended not to progress regardless of curve pattern. Progression of curves greater than 30 degrees appeared to be related to the amount of vertebral rotation. Curves that measured between 50 and 75 degrees at skeletal maturity, particularly thoracic curves, progressed the most; the latter at a rate of nearly 1 degree per year. Lumbar curves less then 50 degrees tended to progress when accompanied by a transitory shift between the lower vertebrae. In a follow up series, Weinstein et al.166 studied outcomes related to health and general function in patients with untreated AIS. Citing previous long-term studies as having a more heterogeneous population of both true idiopathic and non-IS patients, Weinstein et al. argued that late-onset IS (LIS) was a distinct entity with a unique natural history compared to other forms of “idiopathic” scoliosis. Defining LIS as “a structural lateral curvature of the spine arising in otherwise normal children usually during puberty,” the authors compared 117 prospectively evaluated, untreated patients with 62 age- and sex-matched volunteers. Reporting on 50 years of follow up, this review stated that those with LIS were significantly more likely to experience shortness of breath in the presence of a thoracic curve of more than 80 degrees compared to controls. LIS patients were also significantly more likely to report chronic back pain than controls. There was no significant difference, however, in the estimated probability of survival between the two groups. Others have cited no difference in mortality rate between patients with AIS and the general population.131 Thus the authors concluded that untreated adults with LIS demonstrated little physical impairment other than back pain and cosmetic concerns compared to age- and sex-matched controls. Chronic low-back pain is more common in adults with scoliosis, but it does not interfere with a patient’s ability to work or perform activities.122,166
Historical perspective
The history of using external support for spinal deformity dates back centuries. Ambroise Pare´ (1510–1590) is credited as the first to write extensively on the use of metal braces, similar to armor, to treat patients with scoliosis. In the 18th century, recognizing what the S shape the spine could assume in the growing child, Nicolas Andry (1658–1712) wrote of straightening children by “repressing” the “protuberances” that result from the underlying spinal deformity with the use of external supports.7 Throughout the 19th century the Europeans were credited with developing various orthotic designs to correct spinal deformities through the use of steel, leather, and plaster.65 In 1946, Walter Blount first described the Milwaukee brace, which was developed as an alternative to various forms of hinge and turnbuckle plaster casts such as those described by Hibbs79 and Risser139 in the operative treatment of scoliosis.19 Early designs of the Milwaukee brace were described by Richard Bidwell, a certified orthotist, in an effort to make it more reproducible.18 Moe and Kettleson116 first described use of the Milwaukee brace for nonoperative treatment of idiopathic scoliosis in 1970. They described additional refinements that decreased the overall bulk of the system, including removal of the chin pad distraction because it caused orthodontic and facial deformities.
In the 1960s and 1970s, many studies were published dealing with the effects of using orthoses in the nonoperative treatment of idiopathic scoliosis. One early report suggested that patients who were compliant with their prescriptions could expect about 25% correction of thoracic curves and 20% of lumbar curves.90 More adequate follow-up analysis, however, revealed that the dramatic improvement of some curves was offset by the substantial degeneration of others.114 One report stated that while a mean overall improvement of 2 to 4 degrees was seen when comparing curve sizes at the beginning of Milwaukee brace treatment to that of post-treatment follow up, 80% of patients demonstrated a measurable amount of curve progression after discontinuing use of the brace.32 It was becoming clear that permanent, post-treatment curve correction from orthotic treatment was not a realistic expectation; however prevention of further curve progression in the growing child or adolescent seemed possible.
Around this same time, the Boston brace was introduced as a low-profile alternative to the Milwaukee brace in the treatment of thoracolumbar or lumbar curves, and eventually for curves with apices as high as the seventh thoracic vertebra.52,84,94,164 Other low-profile, underarm thermoplastic designs, such as the Wilmington, Miami, and Rosenberger thoracolumbosacral orthoses (TLSOs), were also introduced.29,64,109 Most reports suggested that approximately four out of five adolescents treated with an orthosis for idiopathic scoliosis would not experience any significant curve progression.52,70,115 Patients were enrolled into many studies; however, the factors influencing the risk of further scoliotic curve progression had not yet been well defined. While the early brace studies had included patients at high risk for progression, those studies also included patients not sharing this risk. Despite the identification of some keen insights, such as the importance of in-brace correction to increase the likelihood of a positive outcome, the early research on a brace’s ability to halt curve progression became suspect once practitioners developed a greater understanding of the natural history of the disease.
Studies have shown that the corrective forces of a brace are passive in nature and that the predominant corrective component is the transverse loading of the spine through the use of corrective pads.6,34,63,120,129,181 Early theories suggested scoliosis braces worked partly by a kinesthetic reminder, meaning the patient would actively pull away from an irritating stimulus placed at the apex on the convex side of a curve.17,38,74 However, Wynarsky and Schultz181 reported no difference in trunk musculature electromyographic activity in patients with idiopathic thoracic curves while in and out of a Boston brace, and the electromyographic analysis while the brace was worn would not approach values that could have a significant biomechanical influence on the size of the curve.
Current issues
A number of questions for study remain regarding the use of orthoses in the treatment of idiopathic scoliosis. A consensus conference report from the American Academy of Orthotists and Prosthetists documented both the current understanding of how best to utilize orthoses in the treatment of idiopathic scoliosis and Scheuermann’s kyphosis as well as a list of research priorities to help advance understanding of this practice.1 The priorities include the need to better understand the effect an orthosis has in altering the natural history of curve progression, the best use of a variety of orthotic designs, and the most appropriate application of forces to act upon the spine in a way that is most tolerable for the patient. New designs for orthoses intended to treat spinal deformity are often introduced to the medical community and public, but often in the absence of clinical evidence verifying their usefulness compared either to designs that have been subject to significant study, or to what is understood to be the natural history of the disorder being treated.
Current research
In an effort to form a consensus from the literature on the effectiveness of bracing (including whether part-time bracing controls curve progression as effectively as full-time bracing), the Prevalence and Natural History Committee of the Scoliosis Research Society conducted a meta-analysis on more than 1,900 patients from 20 studies.144 They concluded that bracing (with TLSOs or the Milwaukee orthosis) is indeed effective in controlling curve progression in idiopathic scoliosis and that full-time (23 hours per day) bracing is more effective than part-time (8 to 16 hours per day) bracing. The latter finding is further supported by more recent studies.87,88,135,172
Evaluation of compliance with brace wearing remains very subjective and differs depending on whether the child or the parents are giving the report. Better objective means of documenting compliance would be useful in determining the effectiveness of full-time bracing in comparison to part-time bracing. Newer technology now allows objective assessment of compliance. Temperature sensors or pressure switches combined with data loggers have been imbedded into orthoses.75,76,103–105,124,125,135,156,162 In the future, when these data loggers can be economically fabricated into orthoses, then objective evidence of compliance will be routinely available. From the subjective information currently available, it appears that the highest success rate from a bracing program can be expected when a patient is instructed to wear the orthosis for 20 or more hours per day. However, it also appears that the use of orthoses specifically designed for nighttime-only use exerts a favorable influence on the natural history of adolescent idiopathic scoliosis for patients with single lumbar or thoracolumbar curve magnitudes of 35 degrees or less.38,82,88,133,134,186
Hypokyphosis in thoracic scoliosis secondary to AIS is well documented in the literature.2,41,45,107,136,141,151 Early reports on bracing suggested orthoses should decrease lumbar lordosis to enhance the reduction of a scoliotic curve.95,160,164,174 More recent research, however, has questioned the appropriateness of aiming to tuck the pelvis in an attempt to delordose the lumbar spine as a strategic orthotic maneuver in the treatment of idiopathic scoliosis, because of the positive correlation between lumbar lordosis and thoracic kyphosis. More specifically, if the goal of a scoliosis orthosis is to return the spine to a more normal alignment, further reduction of thoracic kyphosis in an already hypokyphotic spine is contrary to that goal. Some authors have suggested that forces within an orthosis need to be reequilibrated not only to decrease the amount of flattening of thoracic kyphosis that can occur with an anterior translation of the thorax,10,72,93 but even to increase lumbar lordosis72,169 in an effort to increase thoracic kyphosis, all while reducing the scoliosis in the coronal plane. The impact of altering the sagittal spinal alignment on outcome while aiming to reduce the Cobb angle in the coronal plane in the orthotic treatment of idiopathic scoliosis is not well understood. The need remains for further research on the most appropriate application of forces within an orthosis to most appropriately address the three-dimensional aspects of a scoliotic deformity.
The use of computer-assisted manufacturing (CAD/CAM) has been investigated for spinal orthoses.38,51,178,179 Initial reports on the use of CAD/CAM have focused primarily on those requiring lower-extremity prostheses. Technologic improvements that impact the means by which a digital image of a patient’s torso is captured and a greater ability to electronically manipulate the orthotic design are increasing the use of CAD/CAM for those requiring spinal orthoses for deformity. Two reports by Wong et al. suggested CAD/CAM manufacturing of spinal orthoses for AIS required less time179 than the more conventional rectification of a plaster model without compromising the amount of in-brace correction achieved.178 Use of this technology to design and manufacture custom orthoses for spinal deformity will likely increase in as it becomes more comprehensive and cost effective.
Treatment recommendations
The aim of orthotic treatment of idiopathic scoliosis may differ based on the age of onset and size of the curve. In infants with EIS in whom the curve is less than 25 degrees and the RVAD is less than 20 degrees at the time of initial evaluation, active treatment is not required and radiographic follow-up should take place every 4 to 6 months.92 Having the infant sleep in the prone position rather than supine may be of benefit. Most infantile curves that resolve do so by age 1 to 2 years.33,98,110,157 Occasionally, several years may pass before the curve has resolved.163 Follow-up should continue even after resolution, because scoliosis may recur in adolescence.
In a recent prospective study of 136 children with progressive infantile scoliosis who were treated before age 4 years, Mehta demonstrated that scoliosis could actually be reversed by utilizing the patients’ growth in combination with serial casts.112 Ninety-four of the 136 children were treated in the early stages of progression (average age 1 year 7 months), and their scoliosis resolved by the average age of 3 years 6 months. In this group of patients who were successfully managed this way, the succession of corrective plaster casts were ceased when radiographs showed a balanced trunk, minimal apical rotation, and complete or almost-complete correction of the curve. The patients were then treated with custom-molded TLSOs to maintain the correction that had been achieved through casting. Citing the critical importance of compliant wear, if after 6 months the deformity remained corrected, the patient was weaned from the orthosis, with treatment discontinued soon thereafter. No further treatment was needed in these individuals over the course of 10 years of follow-up. In those referred with larger curves (average 52 degrees), or referred for treatment at an older age (average age 2 years and 6 months), treatment could reduce but not reverse the deformity. Many of these patients eventually underwent spinal fusion, with more of them expected to need fusion in the future.
Juvenile idiopathic scoliosis is diagnosed in children ages 3 to 10 years. The female-male ratio ranges from 1.6:1 to 4.4:1, with the difference increasing with age.58,142 Convex-right thoracic curve patterns are most common in juvenile scoliosis. Relatively few patients have thoracolumbar or lumbar curves. Patients with juvenile-onset scoliosis are more likely to have curves that progress and are less likely to respond to bracing. They are more likely to require surgical treatment than those with AIS.108,176 Use of the RVAD has not been found to predict progression of curves in juvenile scoliosis,158 but may be an indication of treatment effectiveness. Patients with progressive curves have a steady increase in the RVAD, while those whose curves resolve usually show a decrease in the RVAD. If the RVAD does not improve following bracing, then it is likely that spinal fusion will be required. The level of the most rotated vertebra at the apex of the primary curve appears to be the most useful factor in determining the prognosis of patients with juvenile idiopathic scoliosis. Those with the apex of the curve at T8, T9, or T10 have an 80% chance of requiring spinal arthrodesis by age 15 years.142 The predictive value of two other factors once thought to be associated with a poor prognosis—thoracic kyphosis of less than 20 degrees, and left-sided curves in boys—has recently been questioned.
Most adolescents with idiopathic scoliosis will not require treatment because of the low probability that their curves will progress.3,100 Therefore treatment is warranted only for those patients whose scoliotic curves are at substantial risk of worsening over time or for patients with severe curves at presentation. Actively growing adolescents (Risser ≤ 2) with curves between 30 and 45 degrees should have an orthosis prescribed at the time of their initial visit.144 In the very immature patient (Risser 0 and premenarchal if female) with a curve exceeding 25 degrees, bracing should also be started immediately.101,144 While most adolescents are treated with an orthosis for curves less than 40 degrees, successful treatment of larger curves has also been reported.87,172 In most cases, growing adolescents with curves exceeding 45 to 50 degrees cannot be stabilized with an orthosis. Skeletally mature individuals with curves exceeding 50 to 55 degrees also are at risk for continued curve progression and therefore should be considered for surgical treatment.167 Possible exceptions include patients with well-balanced double curves of less than 60 degrees whose clinical appearance is acceptable to them. Continued observation is recommended to establish if further progression of their scoliosis occurs, which would necessitate surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree