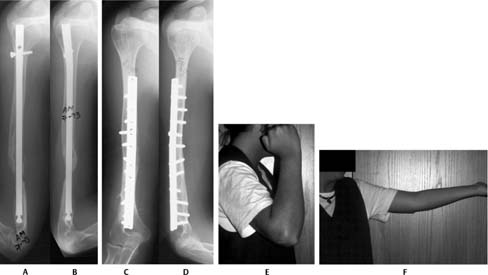
10 Nonunions of the Humeral Shaft The humeral shaft consists of the region between the superior border of the insertion of the pectoralis major to a location just above the supracondylar ridge.1 Fractures of this region account for 3 to 5% of all fractures; most can be managed nonoperatively with good to excellent results.1–4 In a study of 620 patients with humeral shaft fractures treated in a functional brace, nonunion rates were 2% for closed fractures and 6% for open fractures. Varus-valgus and anteroposterior angulation were maintained within 5 degrees.2 Perfect alignment is not essential; 20 to 30 degrees of angulation and up to 3 cm of shortening can be tolerated in the upper extremity without significant functional impairment.1 Angulation can be compensated for functionally by motion at the shoulder and elbow and aesthetically by the musculature and subcutaneous tissues of the arm. A nonunion of the humeral shaft is said to be present when the healing process, which should be completed by 4 months, fails to progress.1 If union is not observed by 24 to 32 weeks after injury, the fracture is unlikely to heal and is considered a nonunion.1,3 Humeral shaft nonunions occur in up to 10% of fractures treated nonoperatively and in up to 15% of fractures treated surgically.1–4 As a nonunion develops, fracture lines will become wider and the edges will become sclerotic. With persistent motion at the fracture site, a synovial pseudoarthrosis or “false joint” may form with a synovium-like cavity and fluid.5 The type of nonunion that develops depends on the blood supply to the fracture. If there is good vascularity, periosteal cartilaginous callus will form. With continued motion, endosteal callus will accumulate and seal off the medullary canal. This hypertrophic nonunion has biological healing potential, but lacks mechanical stability. Hypertrophic nonunions should be treated with rigid stabilization to provide mechanical stability; supplemental bone grafting is unnecessary. If there is poor vascularity at the fracture edges, such as after excessive surgical periosteal stripping, little callus will form and an atrophic nonunion results. In addition to providing mechanical stability, these nonunions require bone grafting to provide biological healing potential. Several factors contribute to the development of a humeral shaft nonunion. These can be broadly grouped into factors related to the personality of the fracture, patient characteristics, and the type of treatment rendered. Factors related to the personality of the fracture include pattern, location, and soft tissue disruption. Certain fracture patterns, such as the transverse, short oblique, or comminuted fractures, are probably more difficult to heal and are likely to go on to nonunion. There is less surface area for healing in these fractures and increased strain, with greater likelihood for displacement and granulation tissue formation.1,3 Recently, a long lateral butterfly fragment of the humeral shaft was been described as a fracture pattern associated with nonunion.6 The fracture originated at the junction of the proximal and middle third of the diaphysis as a hemitransverse medial fracture, which extended with a large, lateral butterfly third fragment. Eight of nine of these fractures progressed to nonunion after nonsurgical management. The healing pattern was identical in all eight: The proximal humeral fragment healed with the proximal portion of the butterfly fragment, but a nonunion between the proximal humeral fragment, the distal humeral fragment, and the distal portion of the third fragment developed.6 Location of the fracture may also predispose to delayed union or nonunion. Fractures at the junction of the middle and distal thirds of the humeral diaphysis may disrupt the primary nutrient artery to the humerus, which may result in problems with fracture healing.3 Blood vessels, nerves, and soft tissue can be interposed at the fracture site, resulting in nonunion and neurovascular compromise.1,3,4 Open fractures of the humeral diaphysis are more likely to go onto nonunion than closed fractures. This is likely due to the soft tissue disruption and periosteal stripping, which occur with the open injury. These types of injuries also predispose to infections that can result in sequestrum formation, osteolysis, implant loosening, and impaired fracture healing.1,3–5,7 Patient factors may also predispose to the development of nonunion. Obesity may predispose a patient to development of nonunion because of difficulty immobilizing the obese arm.3,8 Alcoholism, malnutrition, and smoking may contribute to poor healing potential.1,3,4 Stiffness or ankylosis at the shoulder or elbow can result in increased motion at the fracture site, thus inhibiting union.4 Finally, the type of treatment the patient receives, operative or nonoperative, may determine the healing potential of the humeral shaft fracture. Closed reduction with soft tissue interposition or overdistraction with a hanging arm cast may predispose patients to develop nonunion.1 However, nonunions of the humeral shaft are more likely to occur after operative treatment, with rates varying according to the specific surgical intervention. Excessive surgical exposures with periosteal stripping will disrupt the vascularity and biological healing potential of fractures.5 Treatment of humeral shaft fractures with intramedullary nailing has been reported to result in nonunion rates of 0 to 23%. Risk of nonunion remains significant following plating ranging from zero to 13%.9–14 Irrespective of the type of implant, fixation with inadequate stabilization results in persistent motion at the fracture site. Mechanical instability will result in implant failure before fracture union.1,3,5,7,13,15 Poor quality bone, such as in osteoporosis or pathologic fractures, may make it difficult to achieve rigid stability with internal fixation necessitating alternative techniques to achieve stability and eventually union.4,16 Patients with a humeral shaft nonunion may present with limitations in function and pain that prevent them from performing activities of daily living. In general, this problem should be treated operatively. There are, however, limited indications for the nonoperative treatment of humeral shaft nonunions. If patients have little pain and functional disability or have medical comorbidities that may place them at unacceptable risk for surgical intervention, they may be managed nonsurgically in a functional brace.2,4 Patients with a painless synovial pseudoarthrosis may require the motion at this site to compensate for stiffness at the shoulder and elbow; hence, correcting the pseudoarthrosis in these patients may result in significant loss of function of the extremity.5,7 Electrical stimulation of humeral shaft nonunion has a success rate of 40 to 50% and is therefore not indicated.17 Low-intensity pulsed ultrasound and extracorporeal shock wave therapy have been reported to have inconsistent results on the healing of a nonunion.18,19 Furthermore, these treatments cannot correct deformity; thus, they may not be able to address the functional impairment associated with nonunion. The goals of surgical treatment include correction of deformity and achieving union to relieve pain and restore function of the upper extremity. There are several different surgical techniques that have been described to treat humeral nonunions, including plating, intramedullary nailing, and external fixation. Generally, plating techniques are preferred to treat humeral shaft nonunions. The need for débridement of the nonunion site, bone grafting, and additional techniques to improve vascularization is determined by the biological healing potential of the nonunion (i.e., atrophic versus hypertrophic). Special techniques and implants that do not depend on screw purchase into host bone for stability may be required to treat nonunions in osteoporotic bone. Compression plating, with or without bone grafting, is widely considered the gold standard for treatment of humeral shaft nonunions. The humeral shaft may be approached through several exposures. The anterolateral (Henry) approach may be used to expose the proximal aspect of the shaft.20 A posterior triceps-splitting approach may be used to expose the middle and distal aspects of the humeral shaft.20 A modified posterior approach to the humeral shaft has been described in which the medial and lateral heads of the triceps muscle are subperiosteally elevated and retracted medially with the radial nerve.21 With the standard posterior triceps-splitting approach without mobilization of the radial nerve, the proximal dissection can expose the distal 55% of the humerus. With the modified posterior approach, the distal 94% of the humerus can be exposed. In addition to the greater visualization of the posterior aspect of the humerus, this approach reflects the medial head of the triceps as a unit, thus maintaining continuity of the fibers and preserving triceps function. In a series of 7 patients who underwent treatment of acute humeral shaft fractures or nonunion using this approach, none had evidence of radial nerve dysfunction or triceps weakness at follow-up.21 A medial approach, though rarely used, may reduce potential injury to the radial nerve in patients who have had previous postero-or anterolateral exposures with associated scarring. If a microvascular bone transfer is required, this approach allows access to the brachial artery and its vena comitantes.8 Humeral shaft nonunions treated with rigid 4.5-mm compression plating, lag screw fixation when possible, débridement of the fracture edges, and supplemental autogenous bone grafting have been demonstrated to achieve high union rates (Fig. 10–1).9,15,22–25 A minimum of eight cortices of fixation proximal and distal to the fracture site should be obtained. Union rates after compression plating and bone grafting have been reported to be as high as 100%.8,16,23,24,26 In 10 patients with humeral shaft nonunions, Foster and colleagues observed an 80% union rate with compression plating. A 73% union rate was seen in 11 humeral shaft unions treated with a Kuntscher nail. Subacromial impingement and decreased shoulder motion were seen in the majority of patients who underwent nailing.9 Figure 10–1 (A) Anteroposterior and (B) lateral radiographs of a nonunion of the humerus. The fracture was previously treated with a retrograde intramedullary device. The patient underwent an antegrade exchange nailing, but failed to heal and an atrophic nonunion developed. (C) Anteroposterior and (D) lateral radiographs of the humerus taken 3 years after treatment with a single posterior plate. (E,F) The nonunion healed completely with an excellent functional result. (From Rubel IF, Kloen P, Campbell D, et al. Open reduction and internal fixation of humeral nonunions: a biomechanical and clinical study. J Bone Joint Surg Am 2002;84:1315-1322. Reprinted by permission.) For humeral shaft nonunions, double plating may be indicated in cases of poor bone quality, persistent micro-motion after application of one plate, and to counteract significant deformity. In biomechanical studies, the combination of a posterior limited-contact dynamic compression plate and a lateral 3.5-mm reconstruction plate with or without an interfragmentary screw demonstrated greater axial and rotational stiffness than a posterior limited-contact dynamic compression plate alone.23 In a clinical study of 37 patients plated for humeral shaft nonunions, 18 cases were double plated because of concerns about the adequacy of the stability after application of the single plate construct. No significant differences in healing rate were noted between single- and double-plating techniques; the overall union rate was 92% at an average of 4.8 months postoperatively (Fig. 10–2).23 Thus, the use of a two-plate construct may be helpful when bone quality is poor, or when micromotion is still evident at the nonunion site after application of the first plate. Although excessive soft tissue stripping is a potential concern with double plating, the dissection needed to correct deformity and debride the fibrous tissue allowed application of the second plate without additional exposure. Furthermore, the addition of the second plate did not decrease healing rates.23
Etiology
Treatment
Nonsurgical Treatment
Surgical Treatment
Techniques
Plating Techniques
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree