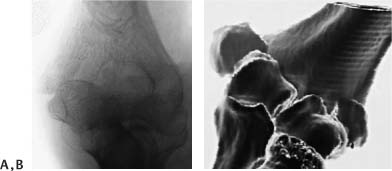
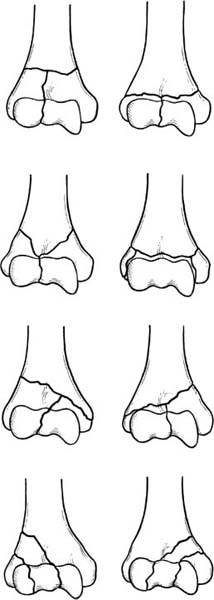
11 Complex Fractures of the Distal Humerus Injuries involving the distal humerus comprise a constellation of complex articular injuries.1–5 Although recommendations for treatment have varied,6,7 there has now been general acceptance of the advantages of operative treatment.8–28 Advances have been made in understanding the variety of fracture patterns, preoperative imaging, surgical exposures, and the techniques and technology for the internal fixation of these difficult fractures–yet several recognized difficulties and complications remain.29–39 These include loss of elbow mobility, nonunion, malunion, posttraumatic arthritis, and ulnar nerve dysfunction. In this chapter, I will concentrate on contemporary issues in the assessment and management of distal humeral fractures, as well as complex fracture patterns. These include multifragmentary articular fractures at or distal to the olecranon sulcus, chondral articular shearing fractures, fractures involving osteopenic bone, and the issues involved with the alternative of total elbow arthroplasty as definitive fracture management. Issues related to surgical exposures, new technologies for internal fixation, and postoperative rehabilitation will be highlighted. The assessment and management of complications post-fracture will be addressed elsewhere in this text. An understanding of the operative anatomy of the distal end of the humerus and its correlation to resultant fracture patterns and surgical fixation is essential.40 The distal humerus is composed of two bony columns, one medial and one lateral, which flare out distally and are separated by the olecranon and coronoid fossa and, more distally, the trochlea. The goal in the surgical reconstruction of the articular anatomy and bony support of the distal humerus is to reconstruct an equilateral triangle consisting of both columns and the intervening trochlea. Instability of the fixation of any one of these three limbs will dramatically weaken the entire surgical repair. Some of the contemporary issues regarding the type and location of plate fixation that will provide optimal skeletal repair will be discussed later. What is important to understand is the relevant relationship of the ulnar and radial nerves to the posterior aspect of the distal humerus. Approximately 10 cm proximal to the medial epicondyle, the ulnar nerve traverses the medial intermuscular septum from the anterior to posterior compartments. The nerve passes distal and posterior to the medial epicondyle enclosed in a fibrous sheath, which is the top of the cubital tunnel. Upon exiting, it courses between the two heads of the flexor carpi ulnaris traveling distally through the anterior compartment of the forearm. The radial nerve crosses the posterior aspect of the humerus ~20 cm proximal to the medial epicondyle. The nerve splits into a branch to the medial head of the triceps, the lower lateral brachial cutaneous nerve, and the posterior interosseous and superficial radial sensory nerves. The posterior interosseous nerve traverses through the lateral intermuscular septum ~10 cm proximal to the lateral epicondyle. With the exception of “simpler” fracture patterns such as the “T” or “Y” fractures, the more complex multifragmented or “smashed” fractures, or those featuring chondral shearing components are not readily appreciated from standard radiographs, even those obtained after traction applied to the arm.41 The evolution of computed tomography (CT) scanning, especially three-dimensional (3D) reconstructions, have added immeasurably to more accurately assessing the fracture patterns preoperatively (Fig. 11–1).42 The reliability and diagnostic accuracy of two-dimensional (2D) versus 3D CT in the classification and management of distal humeral intraarticular fractures was evaluated in our Hand and Upper Extremity Center. Five independent observers evaluated CT scans of 30 consecutive fractures for the presence of five fracture characteristics: a coronal plane fracture line, articular comminution, metaphyseal comminution, presence of separate entirely articular fragments, and articular surface impaction. The results showed that 3D CT reconstruction improved both the intra- and interobserver reliability for the AO/ASIF comprehensive classification and the Mehne/Malta classification systems when compared with 2D CT scans. Figure 11–1 The development of three-dimensional computed tomography (CT) scanning has greatly enhanced the preoperative understanding of complex articular fractures. (A) This shearing articular fracture is poorly visualized in standard radiographs. (B) The three-dimensional CT more accurately depicts the fracture. Figure 11–2 The Mehne and Matta classification is useful to appreciate variable patterns of bony column involvement. The historical convention of describing intraarticular distal humeral fractures as “T” or “Y” fractures has been supplanted by more detailed attempts to define the specific features of each fracture.43–46 Rather than describe the variety of classifications, I will concentrate on but a few contemporary useful classifications. Mehne and Malta based their classification on the surgical anatomy as well as the involvement of the distal humeral bony columns (Fig. 11–2).37,47 Four basic categories were identified–intraarticular, extraarticular, intracapsular, and extracapsular. The intraarticular fractures are divided into single or bicolumnar injuries, and capitellar fractures or trochlea fractures. The bicolumnar fractures can be viewed both by the slope as well as location of the fracture lines and the orientation of the intraarticular components (s). The “H” type would represent the more complex intraarticular patterns with articular fragments separated with adequate bony support. The comprehensive classification (AO/ASIF) system represents an alphanumeric system with three major types including extraarticular (type A), partial articular (type B), and complete articular (type C).48,49 Within each type are three groups and three subgroups, extending from simple to more complex fracture patterns involving both articular and metaphyseal involvement (see Chapter 13, Fig. 13–1). There continues to be an evolution in recognition and classification of the articular injuries of the distal humerus.50 A constellation of patterns of articular shearing fractures has been identified with their basic feature being little or no supporting metaphyseal subchondral bone.51–53 Understanding the specific features of the fracture patterns will play an important role in decision-making and operative tactics. Although some patterns have been identified within the comprehensive classification B3 group, the full extent of the variation and complexity has only recently been described. With the advent of 3D CT reconstruction, a more accurate representation of the fracture pattern preoperatively will permit more accurate preoperative planning of both the surgical approach as well as method of internal fixation (Fig. 11–3). The specific fracture types reflect a progression of injury severity extending from an isolated capitellum (B3.1), trochlea fracture (B3.2), or combined capitellar-trochlea (coronal shear) displaced in the frontal plane to combinations of shearing and impaction injury of both articular surface and distal metaphyseal bone.19,54 Those injuries associated with impaction may prove to be the most difficult to reduce anatomically unless the metaphyseal bony impaction is recognized and elevated. Figure 11–3 The lateral decubitus position permits excellent access to the injured limb as well as to the ipsilateral iliac crest. (A) The patient is placed in the lateral position with surgical preparation of the ipsilateral iliac crest. (B) Dependent edema of the hand and forearm is prevented by wrapping the distal limb in elastic wrap. (Case courtesy of Dr. David King.) For the more complex distal humeral fractures, patient positioning and surgical exposure is crucial to achieving a successful result.55 The patient’s position will depend, in part, upon the surgeon’s preference as well as the nature of fracture and/or associated injuries. With the exception of some chondral shearing fractures, which may be approached through a lateral incision with the patient supine and arm extended on a hand table, the preferred position would be in the lateral decubitus or prone position (Fig. 11–3). The ipsilateral iliac crest can be prepared and draped in the event that autogenous bone graft will be required. As the repair of these fractures may prove technically difficult and lengthy, general anesthesia and the use of a sterile tourniquet are preferred. Under sterile tourniquet control, a straight dorsal incision is made elevating the medial and lateral skin flaps.56 The traditional approach is to curve the incision slightly around the tip of the olecranon to avoid hypersensitivity upon contact; however, I have never found this to be necessary. How to approach and protect the ulnar nerve is a subject of continued discussion. Although it is very reasonable to expose the nerve and perhaps protect it with a nerve loop, continued traction on the nerve during the procedure will risk a traction neuritis.28,57 By the same token, will mobilization of the nerve proximally up to the medial intermuscular septum and distally through the two heads of the flexor carpi ulnaris to end up in a subcutaneous position really prevent postsurgical nerve dysfunction (Fig. 11–4)? In a preliminary study in our service comparing a cohort of patients in whom the ulnar nerve was identified at the onset of the procedure but not mobilized with a similar group of patients in whom the nerve was extensively mobilized and moved into a subcutaneous position, there was no statistically significant difference in postoperative ulnar nerve dysfunction. Although the more commonly used approaches have been both through an olecranon osteotomy or triceps splitting exposure, several additional options exist and may prove useful for specific fracture problems. Figure 11–4 Mobilization of the ulnar nerve 6 cm proximal and distal to the cubital tunnel will permit the nerve to lie in a subcutaneous position at the conclusion of the surgery. The transolecranon approach will provide excellent exposure,58 but enthusiasm for this technique has been tempered by reports identifying associated complications including nonunion, hardware prominence, or proximal migration of longitudinal Kirschner wires, which may inhibit elbow extension.59,60 In addition, when faced with multifragmented fractures in the older patient where total elbow arthroplasty would be an option, an alternative exposure will be required.61 When performing the olecranon osteotomy, several technical features will help minimize potential complications (Fig. 11–5).62 The osteotomy is preferentially done in the middle of the olecranon, where there is the least amount of articular cartilage. By elevating part of the anconeus, this can be directly visualized. The creating of a “chevron” osteotomy with the apex pointed distally will enhance later realignment and fixation. I have found that placing two Kirschner wires obliquely from the dorsal aspect of the proximal ulna to exit just medial to the ventral ridge of the ulna will avoid the wires “backing out” as well as impinging upon the radius during forearm rotation. For the tension band, I use two smaller gauge stainless steel wires (20- or 22-gauge) spaced several centimeters apart in the proximal ulna. These wires are brought under the attachment of the triceps against the very tip of the proximal olecranon. Lastly, to help prevent the Kirschner wires from migrating proximally, these are bent into two 90-degree bends and hammered into the proximal olecranon. There has been some concern regarding the stability of such fixation and whether or not early mobilization is advisable. I have not found this to be the case at all. In a consecutive series of 44 olecranon osteotomies that I performed, there were no nonunions with requirement for second procedure to gain union.63 Only 13% of patients required a second procedure to remove symptomatic wires. Figure 11–5 The technical points of performing an olecranon osteotomy. (A) By elevation of a small portion of the anconeus, direct exposure of the olecranon articular surface permits a more accurate placement of the osteotomy in the center where there is a minimal amount of articular cartilage. (B) Using a thin blade, a cut is created in a chevron pattern, stopping just at the opposite cortex. (C) The osteotomy is completed using a thin blade osteotomy. (D) Fixation of the osteotomy begins with two smooth 0.45-inch Kirschner wires, directed toward the anterior cortex of the proximal ulna and away from the proximal radius to avoid impingement. (E) Two tension wire loops enhance fixation and the proximal Kirschner wires are bent in a 90-degree fashion and impacted into the proximal olecranon. Alternative surgical exposures include the paratricipital posterior approach, triceps split exposure, triceps-reflecting anconeus pedicle (TRAP), triceps sparing elevation, and/or extended lateral exposure.64 The paratricipital posterior approach involves mobilization of the triceps from the medial and lateral intermuscular septa, as well as posterior aspect of the humerus.65,66 This exposure may be more applicable for these fractures at the supracondylar level or simple articular injuries or those complex fractures in which arthroplasty is to be performed. The paratricipital approach will be less optimal for more complex articular injuries especially those at or distal to the olecranon sulcus. The triceps-splitting approach involves splitting the triceps in the midline from the distal third of the humerus to the proximal one fourth of the length of the ulna.67 This approach may prove advantageous in open fractures in which the distal tip of the humeral shaft penetrates the triceps aponecrosis. It is critical to repair the triceps back to the proximal ulna with transosseous suture, as an inadequate repair can adversely affect elbow extension and may inhibit postoperative rehabilitation. When performed carefully, McKee and colleagues68 found no difference in the strength of elbow extension when compared with patients treated with an olecranon osteotomy. The TRAP exposure preserves the neurovascular supply to the anconeus muscle and provides an extensile exposure of the distal humerus.69 The dissection begins distally, elevating the anconeus from the ulna extending proximally toward the lateral epicondyle and the lateral column of the distal humerus. On the medial side, the dissection will extend distally to merge with the distal extent of the lateral exposure followed by sharp elevation of the triceps insertion from the ulna. The entire flap can be mobilized proximally to expose the distal humerus and articular fracture including these complex multifragmented very distal fracture patterns. The triceps elevation approach has been traditionally used when performing total elbow arthroplasty (Fig. 11–6).70,71 It may be used in those fractures in which internal fixation may not prove possible and arthroplasty is to be considered. The dissection of the triceps starts medially off the ulna as an osteoperiosteal flap and continues until the anconeus and triceps can be retracted over the lateral humeral condyle. As with the other triceps elevation procedures, a meticulous repair of the triceps mechanism with transosseous sutures is mandatory. The final alternative surgical exposure is that of the lateral approach.72,73 This exposure is most useful for lateral column fractures as well as articular shearing chondral fractures. For simpler capitellar or unicondylar fractures the lateral collateral ligament complex can be spared or elevated with an osteotomy of the lateral epicondyle extending the dissection to elevate the lateral triceps insertion from the proximal ulna. The elbow can be “hinged open” supported only on the medial soft tissues and affording excellent exposure of the entire anterior surface of the capitellum and trochlea (Fig. 11–7). At the conclusion of the procedure, the lateral soft tissues and/or epicondyle must be carefully repaired with transosseous sutures. Figure 11–6 The triceps elevation exposure is to be considered when the possibility of elbow arthroplasty exists. Although the general principles of definitive internal fixation of intraarticular fractures of the distal humerus are well recognized, the task becomes substantially more complex when faced with multifragmented articular fractures at or distal to the olecranon sulcus. Irrespective of the fracture pattern (s), the basic goal revolves around realignment of the trochlea as close as possible to its original width. By doing so, the inherent stability of the elbow is enhanced. Figure 11–7 Using an extended lateral approach for an articular shearing fracture, the elbow can be “hinged open” to expose the entire articular surface.
Anatomy
Patient Assessment
Radiologic Evaluation
Classification
Treatment
Surgical Treatment
Techniques
Internal Fixation Techniques
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree