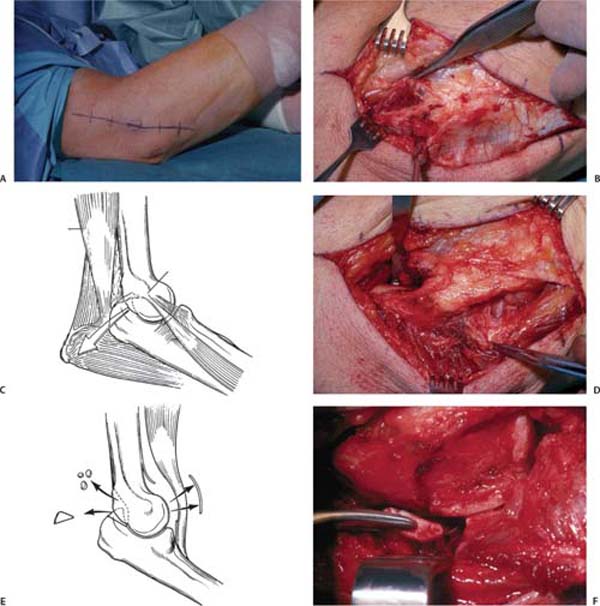
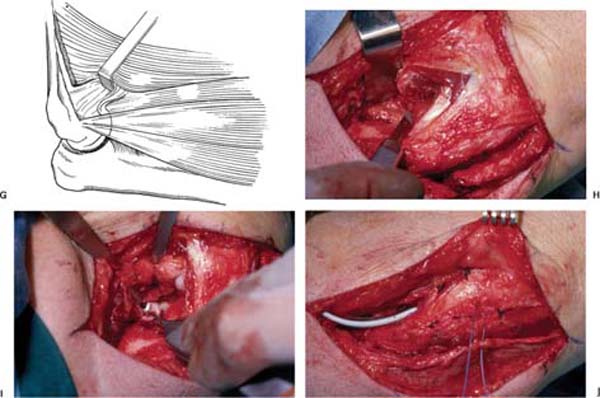
15 Reconstruction of Posttraumatic Stiffness and Instability Instability and stiffness are common complications of complex elbow trauma. Chronic lateral collateral ligament (LCL) insufficiency is unusual and is characterized by a mobile, functional elbow that is prone to intermittent symptomatic subluxation or dislocation.1 In contrast, persistent subluxation and dislocation after trauma are more common and are usually associated with articular fractures and stiffness.2 Other contributors to elbow stiffness include contractures of skin, capsule, and muscle; heterotopic ossification; nerve compression; malpositioned implants; articular damage; and fracture nonunion or malunion.3 Isolated LCL instability is effectively treated by reconstructing the ligament with a tendon graft. The treatment of stiffness, subluxation, and dislocation are less predictable and determined largely by the relative preservation of the trochlear notch and the articular surfaces. Morrey and colleagues found that 15 daily activities could be accomplished with an arc of ulnohumeral motion between 30 and 130 degrees of flexion and an arc of forearm rotation from 50 degrees of pronation to 50 degrees of pronation.4 These numbers should not, however, be used to decide when to operate on elbow stiffness. Patients can adapt to and function very well with much less motion,5 perhaps more so when the stiffness is in the nondominant elbow. Therefore, the indication for operative contracture release is a combination of diminished elbow motion and disability directly related to stiffness in a patient who understands and agrees to the operative risks. It is helpful to be aware of the details of prior trauma, burn, or central nervous system injury, as well as any prior surgeries. In patients with prior central nervous system injury, one must determine the ability of the patient to participate in a postoperative rehabilitation protocol.6 A painful contracture suggests arthritis or ulnar neuropathy. Numbness and dexterity problems suggest ulnar neuropathy. Patients with malunion, nonunion, subluxation, or dislocation are at risk of articular surface injury and progressive arthrosis. They usually have severe stiffness. Patients with chronic LCL insufficiency present with good elbow function, but either recurrent dislocation or symptomatic subluxation. The quality of the skin is important, particularly in post-burn contractures.7 The status of the skin with respect to prior injury and operative treatment will influence the operative tactics. When planning operative treatment of a posttraumatic contracture, the authors prefer to wait until the skin and scar are mobile and soft, and no longer edematous or adherent (usually about 3 or 4 months). A complete motor and sensory examination of the ulnar nerve along with Tinel’s sign and an elbow flexion test should be performed. Tests for posterolateral rotatory instability are best performed in a very relaxed or anesthetized patient. These tests are intended to provoke a clunk or a skin divot consistent with subluxation of the elbow joint. Pain alone is too nonspecific to be considered a positive test. A posterolateral rotatory stress can be applied to the elbow by applying axial compression, valgus, and supination. This can be done with the patient supine and the arm externally rotated – a position that helps to both relax the patient and to prevent humeral rotation when the stress is applied.1,8 As stress is applied, the elbow is brought from extension into flexion. A clunk indicates relocation of a subluxated elbow. Alternatively, a posterolateral rotatory stress is produced when a patient is asked to support their body weight on the maximally externally rotated and supinated arms in a sitting position.9 In our opinion and experience, unless patients have learned how to provoke subluxation with certain positions and stresses, these tests are not definitive in an awake patient. Posterolateral rotatory instability is very uncommon and elbow pain and dysfunction are very common. Therefore, only a clearly positive and reproducible test should be considered positive. Standard anteroposterior and lateral radiographs of the elbow are usually sufficient to identify and characterize arthritis, heterotopic ossification, and nonunions, but computed tomography (CT) is occasionally of use. In more complex cases, the CT scan can help with preoperative planning.6 The authors find three-dimensional reconstructions particularly easy to interpret. CT scans may be especially useful for characterizing malunion of the articular surface of the distal humerus.10 Neurophysiological testing should be considered when there is any possibility of preoperative ulnar neuropathy. In the presence of nonunion, infection should be considered and investigated with laboratory and imaging studies when appropriate, and possibly a diagnostic aspiration. Simple capsular contracture (no heterotopic bone, no malunion or nonunion, no implants blocking motion, no ulnar neuropathy, etc.) usually responds to time, reassurance, encouragement of exercises, and static progressive or dynamic elbow splinting.11 Therefore, one should never rush into operative treatment of capsular contracture as long as progress is being made: Patience and frequent visits for reassurance and encouragement are worthwhile. Obvious hindrances to motion, including heterotopic bone, malunion, nonunion, prominent implants, ulnar neuropathy, subluxation, or dislocation merit prompt operative treatment. Heterotopic ossification can be resected within 4 months of injury (when radiographically mature and the skin is mobile and has little or no edema) regardless of activity on bone scans.6,7,12,13 Stiffness associated with advanced arthrosis or unsalvageable nonunion or nonunion should be treated by interpositional or prosthetic elbow arthroplasty.3,14 Elbow capsulectomy can be performed simultaneously with débridement of a deep infection. It also forms an integral part of the treatment of malunion,10 nonunion,15 and instability.2 Unstable skin can be treated with either prior or concomitant procedures to improve soft tissue coverage.7 Patients with capsular contracture that desire extension can be treated with lateral capsulectomy.16,17 Patients with concomitant ulnar neuropathy or limitation of elbow flexion are best treated with medial capsulectomy so that the ulnar nerve can be addressed.18,19 Patients with heterotopic bone, prominent implants, or complex contracture that cannot be adequately released from medial or lateral alone may benefit from a combined medial and lateral release.7,19 Preoperative radiation therapy, a single 7-gray (700-rad) dose, is administered to patients with heterotopic bone to be excised. Direct anterior release20 is rarely the best choice because the anterior capsule can be more safely excised from medial or lateral. A posterior release with splitting of the triceps and fenestration of the olecranon fossa for access to the anterior elbow is used primarily for débridement of primary elbow arthrosis21 rather than posttraumatic stiffness or arthrosis. In this chapter, we will describe an elbow capsulectomy through lateral and medial intervals. The best candidate for an arthroscopic elbow contracture release is a patient with capsular contracture with or without osteophytes, but no ulnar nerve problem, heterotopic bone, implants, etc. Because such patients are uncommon and because arthroscopic elbow contracture release is more difficult and more dangerous than open contracture release, arthroscopic contracture release should only be done by surgeons with sufficient training and experience.22–26 Chronic posterolateral rotatory instability is treated with ligament reconstruction using a tendon graft.8 Subluxation and dislocation are treated with open realignment, reconstruction of articular insufficiency due to fractures, and ligament repair. Ligament reconstruction is not usually necessary. The reconstruction is often protected with hinged external fixation.2,27 In the presence of advanced articular injury, interposition arthroplasty may be considered. Open elbow contracture release can be performed under general anesthesia or brachial plexus block. The patient is supine and the arm is supported on a hand table. A sterile tourniquet is applied to the upper arm. The skin incision can be straight and directly over the muscle interval to be utilized or posterior28,29 with a skin flap elevated to expose the muscle interval (Fig. 15–1A). If both medial and lateral intervals are to be used, a single posterior or both medial and lateral incisions can be used. In the unusual case of a direct anterior release, a direct anterior skin incision is used and should cross the flexion crease obliquely. Hinged external fixation has not been particularly helpful and has not been necessary after elbow contracture release.30 In the stiff elbow, slight instability is well tolerated (such as that which occurs when an ossified medial collateral ligament is fractured) and does not merit hinged external fixation. Figure 15–1 Open elbow contracture release through a lateral muscular interval. (A) A lateral or posterior skin incision can be used. (B) Identification of the supracondylar ridge orients the surgeon and helps with the initiation of the release. The origin of the extensor carpi radialis longus is incised and elevated off of the anterior surface of the distal humerus. (C) The triceps and anconeus are elevated off of the posterior surface of the distal humerus. (D) The posterior capsule is exposed and excised. (E) The olecranon fossa is cleared. (F) The tip of the olecranon is excised if it is felt that this will enhance elbow extension. (G) An anterior muscle interval is developed between the extensor carpi radialis brevis and the extensor digitorum communis. (H) The anterior capsule is exposed and excised. (I)
Patient Assessment
Physical Examination
Radiographic Assessment
Laboratory Studies
Treatment
Surgical Treatment
Elbow Stiffness
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree