Neuromuscular Disorders
Michael J. Botte
Orrin Franko
Neuromuscular disorders that cause foot deformities are often divided into two main types: spastic and paralytic. Spasticity develops from injury to the upper motor neurons of the central nervous system (involving the brain or spinal cord). These injuries include traumatic brain injury (TBI), stroke, spinal cord injury (SCI), and cerebral palsy (CP). Conversely, paralysis or paresis (weakness) commonly develops from injury to lower motor neurons (involving the peripheral nerves). A classic example is Charcot—MarieTooth (CMT) disease (peroneal muscular atrophy), which involves peripheral nerve demyelination and degeneration. Peripheral nerve lacerations and polio also involve the lower motor neurons and result in paralysis, not spasticity.
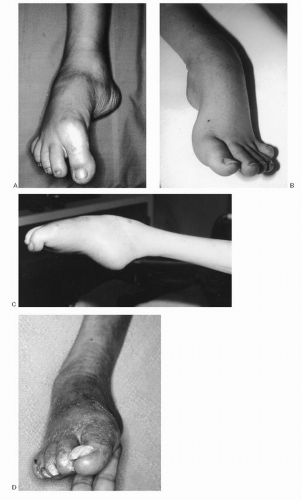
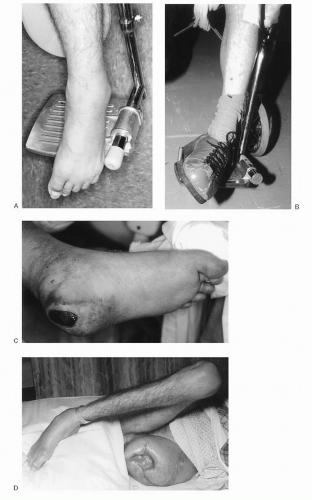
Whether an affliction results in spasticity or paralysis, the net result is muscle imbalance in the limb. With significant muscle imbalance, the stronger, more active, or mechanically advantaged muscles overpower the weaker or paralytic muscles and pull the limb into a deformity (Fig. 3.1). This leads to the several common foot and ankle deformities seen in neuromuscular disorders, including equinus, varus, equinovarus, cavus, and various toe deformities. Because of the differences of etiology, associated deformities, and methods of treatment, this chapter is divided into two sections: disorders of spasticity and disorders of paralysis.
Although the emphasis of the text is placed on the foot, the interdependence of the hip and knee for function and operative planning must also be appreciated and is discussed in association with these problems. Evaluation of the whole patient must be kept in mind and the multidisciplinary team approach is stressed.
DISORDERS OF SPASTICITY
PATHOGENESIS
Etiology
TBI is commonly caused by a direct blow to the skull, penetrating injury, or an anoxic episode. A direct blow results in immediate local neural disruption, which can be compounded by subsequent ischemia from subdural or epidural hematoma. Common events associated with TBI are motor vehicle and motorcycle accidents, assaults, and gunshot wounds. Anoxic injuries are caused by near drowning, chemical asphyxia, drug overdose, and myocardial infarction. Brain damage is global in these patients and the prognosis is often poor. Near-drowning accidents are the most common cause of acquired spasticity in children. In addition, brain injury can occur from severe inflammation, infection, neoplasm, metabolic causes, or other vascular afflictions or malformations that result in neuron death.
Stroke or cerebrovascular accident (CVA) is the result of interruption of the oxygenation of the brain by thrombosis, emboli, or hemorrhage. Cerebral thrombosis accounts for nearly three-fourths of patients with stroke. Arteriosclerosis and smoking history are known predisposing factors for thrombosis. The risk of ischemic stroke in current smokers is about double that of nonsmokers after adjustment for other risk factors. Spontaneous intracerebral or subarachnoid hemorrhage, for which hypertension is a predisposing factor, accounts for approximately one-sixth of patients sustaining CVAs. Emboli account for one-tenth of cases of CVA and are usually associated with extracranial pathology such as atherosclerosis or arrhythmias. Atrial fibrillation increases the risk of stroke by about 5-fold.
In the case of SCI, the most common cause is trauma, usually from direct injury, compression, or hematoma following fractures or dislocations of the spine. Common causes by percentage of SCI are motor vehicle accidents (40% to 48%), falls (8% to 21%), acts of violence (15% to 37%), sports injuries (14% to 15%), and miscellaneous causes (3%). Of the sports injuries, diving and surfing comprise about 70% of injuries, followed by football, snow skiing, gymnastics, wrestling, and horseback riding. Other causes include compression from neoplasm and myelopathy from infection, inflammation, or vascular disorders.
Spastic CP includes a spectrum of brain injury caused before or during birth or in the immediate postnatal period. These injuries are associated with hypoxia, trauma, metabolic or infectious causes, and congenital malformations. Injuries of hypoxia that occur before birth include those from interruption of blood flow through the umbilical cord (associated with prolapse or torsion), placental
abnormalities (e.g., placenta previa or placental infarction), coagulopathies, and maternal cardiopulmonary disease. At birth, a difficult delivery can result in brain injury from trauma or from a hypoxic episode. Birth hypoxia has been estimated by the Center for Disease Control (CDC) to account for less than 10% of CP cases. A difficult delivery is more common with abnormal fetal position or presentation, or prolonged labor. Neonatal apnea (failure to breathe after birth) can be related to prematurity, hypoxia during pregnancy or delivery, or fetal cardiopulmonary insufficiency (from atelectasis, bronchial obstruction, pulmonary edema, or anatomic malformation). Fetal injury may also occur from toxic injury, toxic accumulation of naturally occurring substances (e.g., Rh incompatibility), abnormal metabolic conditions (e.g., maternal uremia and diabetes), or infectious causes. Infection of the placental membranes (chorioamnionitis) may account for 12% of spastic CP among children born full term and 28% born prematurely.
abnormalities (e.g., placenta previa or placental infarction), coagulopathies, and maternal cardiopulmonary disease. At birth, a difficult delivery can result in brain injury from trauma or from a hypoxic episode. Birth hypoxia has been estimated by the Center for Disease Control (CDC) to account for less than 10% of CP cases. A difficult delivery is more common with abnormal fetal position or presentation, or prolonged labor. Neonatal apnea (failure to breathe after birth) can be related to prematurity, hypoxia during pregnancy or delivery, or fetal cardiopulmonary insufficiency (from atelectasis, bronchial obstruction, pulmonary edema, or anatomic malformation). Fetal injury may also occur from toxic injury, toxic accumulation of naturally occurring substances (e.g., Rh incompatibility), abnormal metabolic conditions (e.g., maternal uremia and diabetes), or infectious causes. Infection of the placental membranes (chorioamnionitis) may account for 12% of spastic CP among children born full term and 28% born prematurely.
Epidemiology
Epidemiologic aspects of these neuromuscular diseases demonstrate the magnitude of these problems and their importance to so many patients, their families, and society in general.
The Centers for Disease Control and Prevention estimated in 2011 that 1.7 million people in the United States sustain TBI annually. Of these, 52,000 do not live, leaving a large number of survivors with spasticity. TBI is the leading cause of acquired spastic limb deformity in young adults. It is also the cause of death in 55% of multiple trauma patients dying within the first 2 days of hospitalization. Males between 15 and 25 years of age are the most common victims of TBI, with children aged 0 to 4 and adults older than 65 years comprising other common age groups. Despite the severe deficits sustained, many patients with TBI survive long enough and achieve adequate function to justify aggressive rehabilitation and operative reconstruction. Because most traumatic injuries to the brain occur in young adults, those who survive commonly have a normal life span despite the injury. Foot and ankle deformities and gait disturbances are frequent problems in this population.
The CDC estimated in 2011 that 795,000 people in the United States have a stroke annually. About half of these survive each year. Approximately 610,000 of these are first or new strokes, and about 185,000 people who survive a stroke go on to have another. Nearly three-quarters of all strokes occur in people older than 65 years, although stroke can occur at any age. Stroke is the third leading cause of death in the United States (behind heart disease and cancer) and is the leading cause of adult hemiplegia. More than 2 million people currently have permanent neurologic deficits following stroke, and the average patient who survives a stroke beyond the first few months has a life expectancy greater than 5 years. It has been estimated that 10% of stroke patients have spastic deformities that could benefit from surgery, providing a patient population of 20,000 to 25,000 new surgical candidates per year. In addition, there are already approximately 2.5 million surviving stroke patients in the United States, adding to this large number of patients who could benefit from operative management.
The Foundation for Spinal Cord Injury Prevention, Care, and Cure notes that SCI occurs in 12,000 people per year in the United States, with 200,000 people currently living with SCI in the United States. Reported average ages at injury are 16 to 30 years, with a median age of 28.7 years. Males comprise 80% of cases. Motor vehicle accidents, falls, acts of violence, sports injuries, and miscellaneous causes account for the majority of SCI. Occurrence of SCI increases with increased daylight hours and with increased temperature, usually associated with summer seasonal activities and outdoor sports. Fifty-three percent of all injuries occur on weekend days (Friday through Sunday). Gunshot spinal cord injuries appear to have a higher incidence in undeveloped and developing countries. In sports injuries, about 5% of SCIs have resulted in incomplete paraplegia, 4% in complete paraplegia, 47% in incomplete quadriplegia, and 45% in complete quadriplegia.
The most common motor disability acquired during childhood is CP. Population-based studies from around the world report prevalence estimates of CP ranging from 1.5 to more than 4 per 1,000 live births. Regional estimates show that CP occurs in 1.7 to 2 per 1,000 one-year-olds in the United States, 0.93 to 1.28 per 1,000 in China, and 2.08 per 1,000 in Europe. Usually, one in seven children with CP does not survive the first year of life. Males are involved 1.2 times more frequently than girls. Spastic CP is the most common type of CP, found among approximately 80% of CP children. Spastic diplegia occurs in 7% to 36% of cases. In 2006, 56% of children with CP were able to walk independently, whereas 33% had limited or no walking ability. About 20% of CP children have severe intellectual deficits that contribute to their inability to walk. Prematurity and associated low birth weight are associated with higher incidences of CP; in infants weighing less than 1,500 g at birth, the rate of CP was more than 70 times as high as that in infants weighing 2,500 g or more.
Pathophysiology
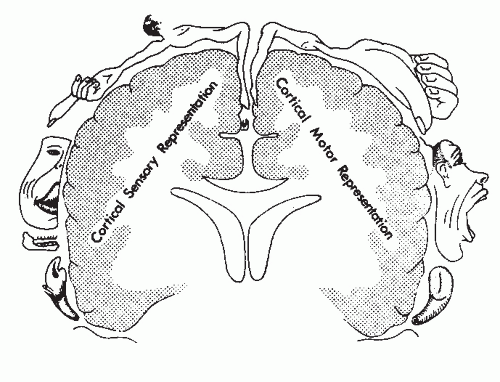
Spasticity develops from interruption of upper motor neuron inhibitory pathways from the brain to the spinal cord (Fig. 3.2). With the loss of the inhibitory pathways, the muscle reacts more to the influence of the spinal reflex, resulting in spasticity, which can cause muscle imbalance and lead to extremity deformities. In the foot and ankle, the most common deformity is equinus and varus.
Dynamic Nature of Spasticity
In disorders of acquired spasticity (TBI, CVA, and incomplete SCI), there is an initial dynamic (i.e., changing) nature, which is important to appreciate for proper planning and timing of surgical procedures. In these disorders, immediately following the initial central nervous system insult, there is usually a brief period (from hours to weeks) of flaccid paralysis or paresis, hypotonia, and depression of stretch reflexes of the neurologically impaired limb. The neural injury, which disrupts the inhibitory pathways of the brain to the muscles, allows the muscles to become influenced by or come under the control of the spinal reflex arc. When influenced by the reflex arc, the muscles become hypersensitive to passive stretch, resulting in reflexive contraction.
Therefore, following the initial period of hypotonia, there is a period of increasing muscle tone. The stretch reflexes return and there is a progression to hyperactive reflexes, which culminate in spasticity. Muscle tone and hyperreflexia reach a peak within a few days or weeks. Besides increased tone, muscles may exhibit hyperreflexia, clonus, or rigidity. Clonus is an abnormal repetitive rhythmic muscle contraction following initial stretch. Volitional control is often impaired, and there may be overall residual weakness and loss of dexterity. Spastic paralysis is seen in severely afflicted muscles.
Therefore, following the initial period of hypotonia, there is a period of increasing muscle tone. The stretch reflexes return and there is a progression to hyperactive reflexes, which culminate in spasticity. Muscle tone and hyperreflexia reach a peak within a few days or weeks. Besides increased tone, muscles may exhibit hyperreflexia, clonus, or rigidity. Clonus is an abnormal repetitive rhythmic muscle contraction following initial stretch. Volitional control is often impaired, and there may be overall residual weakness and loss of dexterity. Spastic paralysis is seen in severely afflicted muscles.
Because upper motor neurons have some capacity to recover, there is a long period of spontaneous neurologic improvement during which spasticity improves and muscles return to a more normal, less hypertonic state. Strength, coordination, and volitional control as well as sensory and cognitive function all improve to varying degrees during this recovery phase. The duration of recovery varies among the different types of acquired spasticity (Table 3.1).
Operative procedures for reconstruction should usually be delayed until a patient is no longer neurologically recovering (or making improvement in a rehabilitation program). Thus the data listed in Table 3.1 can act as a rough guide for timing the surgical procedures if deformity exists and recovery has reached a plateau (discussed further under surgical treatment).
TABLE 3.1 NEUROLOGIC RECOVERY TIMES IN DISORDERS OF SPASTICITY | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
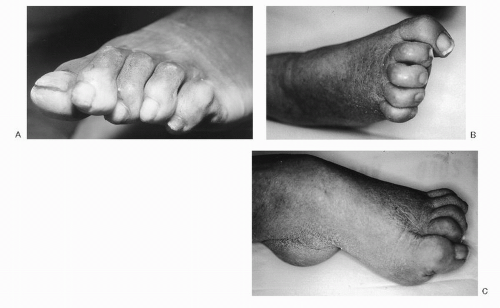
Limb Deformity from Spasticity
With spasticity, the stronger or more hyperactive muscles or those with mechanical advantage overpower the weaker or paralytic muscles and pull the limb into a deformity. This leads to the common foot and ankle deformities seen in neuromuscular disorders, most often equinus or equinovarus along with toe flexion deformities (Figs. 3.1 and 3.3). The equinus component of the deformity is usually from spasticity of the gastrocnemius and soleus, with additional contributions from the tibialis posterior, flexor hallucis longus (FHL), and flexor digitorum longus (FDL). The majority of the varus component of deformity is from the tibialis anterior (in TBI or CVA) or from the tibialis posterior (in CP) and is possibly worsened in both by any associated weakness of the peroneus longus and brevis. The differences in the tibialis anterior contribution to the varus in TBI and CVA compared with the tibialis posterior contribution in CP are important because these muscle differences have implications in operative correction when addressing the specific muscles at fault. Cavus deformity is less often seen in TBI, CVA, and CP, and is usually associated with weakness of the intrinsic muscles of the foot (seen more commonly in paralytic disorders; see later discussion).
Anatomic Correlations between Area of Brain Injured and Severity of Limb Involvement
Different clinical presentations result from different areas of brain involvement. The midcortex of the brain in the sagittal plane controls sensory and motor functions predominantly in the lower extremity and foot (see Fig. 3.2). The anterior cerebral artery supplies this area. A stroke involving the anterior cerebral artery usually results in hemiplegia with deficits in the lower extremity. Severe foot deformities can occur from injuries to this part of the brain (Figs. 3.1 and 3.3). More commonly, however, a CVA involves the middle cerebral artery, which supplies the cerebral cortex, which controls the face, upper extremity, and trunk. These patients have hemiplegia with more speech and upper extremity deficits than lower extremity involvement, but lower extremity
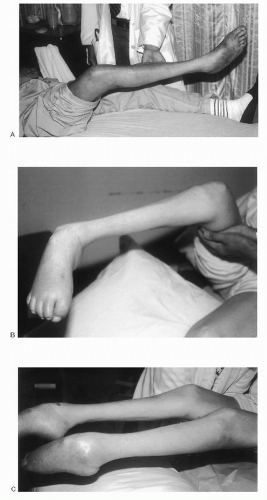
involvement may also be significant. Often, TBI also involves this area of the cerebral cortex, and a patient can have similar deficits as those with a CVA (Fig. 3.4). Anoxic injuries, which are usually more global cerebral insults, produce a wide spectrum of bilateral upper and lower extremity deficits. The entire brain and brainstem may be involved, producing the most severe clinical picture of spastic quadriplegia and mental retardation. In CP, because of the many possible etiologies and mechanisms for brain injury, several clinical presentations and various dyskinesias can develop, including athetosis and ataxia. Athetosis is marked by continuous slow, involuntary writhing movements, especially in the hands. Ataxia is exemplified by loss of muscular coordination, irregularity of muscular action, intention type tremor, and marked unsteadiness in standing or ambulation. Ataxia is commonly seen with cerebellar involvement.
involvement may also be significant. Often, TBI also involves this area of the cerebral cortex, and a patient can have similar deficits as those with a CVA (Fig. 3.4). Anoxic injuries, which are usually more global cerebral insults, produce a wide spectrum of bilateral upper and lower extremity deficits. The entire brain and brainstem may be involved, producing the most severe clinical picture of spastic quadriplegia and mental retardation. In CP, because of the many possible etiologies and mechanisms for brain injury, several clinical presentations and various dyskinesias can develop, including athetosis and ataxia. Athetosis is marked by continuous slow, involuntary writhing movements, especially in the hands. Ataxia is exemplified by loss of muscular coordination, irregularity of muscular action, intention type tremor, and marked unsteadiness in standing or ambulation. Ataxia is commonly seen with cerebellar involvement.
Classification
Spastic disorders can be grouped using several classification schemes and descriptive terms. These are based on acquired versus static spasticity and the limb or limbs involved. In addition, spasticity has been classified according to the degree of spasticity, the muscle groups involved, the type of movement disorder, and the types of deformities present.
Classification Based on Acquired versus Static Spasticity
The acquired spasticity group includes TBI, stroke, and SCI, where spasticity is acquired in a previously normal limb. The static spasticity group includes CP, in which the neurologic insult occurs at birth or in the perinatal period. Acquired spasticity differs from static spasticity in that the acquired spasticity may change (decrease) over time as a result of neurologic recovery following the initial brain or spinal injury. The spasticity of CP is static and does not usually change over time. (Deformities in CP, however, may change over time, especially during periods of rapid growth or as a result of chronic effects of spasticity on the immature skeleton.)
Classification Based on Extremity Involved
Spasticity can be described as spastic monoplegia or monoparesis involving one extremity, paraplegia or paraparesis involving both lower extremities, quadriplegia or quadriparesis, and tetraplegia or tetraparesis involving all four extremities. The suffixes plegia and paresis denote paralysis and weakness, respectively. The term diplegia is often used to describe more involvement in the lower extremities than in the upper extremities. Hemiplegia and hemiparesis denote involvement of one upper and lower extremity on the same side. In CP, diplegia accounts for about 50%, hemiplegia for about 30%, and quadriplegia for about 20% of those with spasticity.
Classification Based on Degree of Deformity
Goldner originally classified CP according to degrees of deformity to include mild, moderate, and severe types. A mild deformity implies slight spasticity in the gastrocsoleus muscle group, voluntary action of the tibialis anterior, and minimal or no muscle imbalance owing to muscle weakness caused by cortical cell damage. Minimal spasticity of the adductors and mild tightness of the hamstrings may coexist with equinus. A moderate deformity indicates a greater degree of muscle tension, significant soft tissue, or fixed contracture in the calf muscles; unequal activity or overactivity of the invertors or evertors of the foot; and no voluntary
control of the dorsiflexors of the foot. A severe deformity indicates fixed contracture of the calf muscles, atrophy of the muscle mass, equinus uncorrectable by manipulation, muscle imbalance with overpull of the invertors or evertors, and no voluntary or involuntary action of the dorsiflexors. The hip flexor muscles and adductor muscles are often contracted, along with the hamstring muscles, producing hip flexion, adduction deformity, and knee flexion contracture.
control of the dorsiflexors of the foot. A severe deformity indicates fixed contracture of the calf muscles, atrophy of the muscle mass, equinus uncorrectable by manipulation, muscle imbalance with overpull of the invertors or evertors, and no voluntary or involuntary action of the dorsiflexors. The hip flexor muscles and adductor muscles are often contracted, along with the hamstring muscles, producing hip flexion, adduction deformity, and knee flexion contracture.
Classification of Cerebral Palsy Based on Movement Disorders
More recently, CP has been classified on the basis of the type of movement disorder. This classification places the patients into two main groups: those with spasticity (about 80%) and those with extrapyramidal or dystonic movements (about 20%). The extrapyramidal group includes those with injury to the basal ganglia of the brain, who exhibit athetosis, chorea, ballismus, ataxia, or hypotonia (Table 3.2). Athetosis consists of involuntary persistent writhing movements, usually of the hands and trunk. Chorea is characterized by a ceaseless involuntary variety of rapid, highly complex, jerky movements. Ballismus involves dyskinetic flinging or violent movements usually caused by contractions of proximal limb muscles. Ataxia is noted by loss of coordination and notably impaired balance with associated gait disturbances. Hypotonia is an abnormal loss or decrease in muscle tone. This classification is clinically relevant in that classic spasticity responds more to conventional methods of muscle relaxants (e.g., benzodiazepines) and to muscle lengthening or recession, whereas the extrapyramidal movement patterns may react less predictably to either medical or operative management.
Classification Based on Deformity
Spastic foot deformities are usually classified as equinus, varus, equinovarus, valgus, and planovalgus. Equinovarus is the most common form. Associated toe deformities are variable, but can be grouped into intrinsic minus (claw toe deformity, characterized by extension at the metatarsophalangeal [MTP] joint, and flexion of the proximal and distal interphalangeal [DIP] joints), hammer toe deformity (characterized mainly by extension at the MTP joint and flexion at the proximal interphalangeal [PIP] joint), and mallet toe deformity (characterized chiefly by flexion at the DIP joint).
TABLE 3.2 EXTRAPYRAMIDAL MOVEMENT DISORDERS SEEN IN CEREBRAL PALSY | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
DIAGNOSIS
History and Physical Examination
It is important to establish the etiology and type of neurologic involvement as well as the time elapsed (days, months, or years) from the original affliction. Note whether the affliction is one of acquired or static spasticity. The patient’s cognitive involvement (with memory problems, agitation, or retardation) may require the assistance of family members and healthcare workers as well as a review of the patient’s medical record. If the spasticity is acquired (e.g., from TBI or stroke), one should determine whether the patient is still neurologically recovering or has reached a plateau in improvement (see Table 3.1).
When gathering the history, determine the rehabilitation treatment and the results received to date, including type and amount of physical therapy, use of splinting and orthoses, current or past medications or injections (Botulinum or phenol) used to decrease spasticity, and any previous operative management.
For specific foot and ankle involvement, functional capabilities can, in part, be established from the history, such as whether the patient has retained volitional control of the foot and whether the patient is able to ambulate, perform transfers, dress, place the foot plantigrade on the wheelchair footrest or floor, or bear weight. Determine whether the contracture is painful.
Establish whether an orthosis can be worn, whether shoe wear is prevented, whether the foot can be placed on a plantigrade wheelchair footrest, and whether there are problems with calluses or skin breakdown.
Clinical Features
The most frequent foot and ankle deformities in spasticity disorders are equinus of the ankle and varus of the hindfoot, thus resulting in the commonly seen equinovarus deformity. Various toe deformities often coexist and usually include toe flexion attitudes. The hallux is often flexed at the MTP and interphalangeal joints. The hallux may, however, develop an extension deformity at the MTP joint with flexion of the interphalangeal joint, producing a type of claw toe or “cockup deformity.” Less common deformities are foot planovalgus or cavus, or various toe extension deformities. The hip and knee are often afflicted as well in spasticity disorders. The most common hip deformities are flexion and adduction. Flexion of the knee is the most common knee deformity.
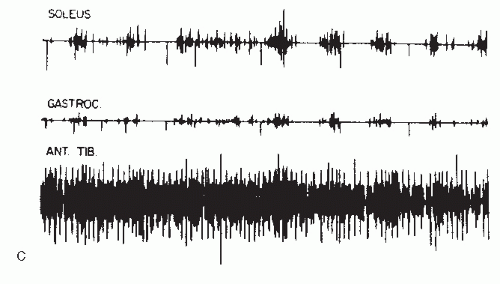
Several clinical problems develop from these deformities. Functional problems include impairment of ambulation or stance for wheelchair transfers, problems with positioning the foot on the wheelchair footrest (Fig. 3.5), inability to wear shoes or protective shoe wear, and difficulty dressing. The deformities can lead to development of painful callosities, skin maceration, and pressure sores; difficulty in patient hygiene; and extremity pain. Equinovarus often results in painful callosities of the lateral plantar foot from concentrated pressure beneath the fifth metatarsal
head or metatarsal styloid process of the fifth ray. Callosities also develop on the tips of the toes from toe flexion deformities where the toes press against the floor. Callosities may develop on the dorsum of the PIP joints where extension at the MTP joint or acute flexion of the PIP joint may result in increased pressure against the shoe. Severe varus can produce maceration and skin breakdown within the skin folds of the medial foot. Long-standing deformities, if not mobilized, lead to fixed soft-tissue contractures. Joint subluxation and dislocation can occur with chronic imbalance. Severe foot deformities that prevent use of shoe wear for comfort or protection may also be so severe as to preclude the fitting of orthotic devices. Pressure sores of the hindfoot, lateral foot, and between the toes have led to development of osteomyelitis and amputation.
head or metatarsal styloid process of the fifth ray. Callosities also develop on the tips of the toes from toe flexion deformities where the toes press against the floor. Callosities may develop on the dorsum of the PIP joints where extension at the MTP joint or acute flexion of the PIP joint may result in increased pressure against the shoe. Severe varus can produce maceration and skin breakdown within the skin folds of the medial foot. Long-standing deformities, if not mobilized, lead to fixed soft-tissue contractures. Joint subluxation and dislocation can occur with chronic imbalance. Severe foot deformities that prevent use of shoe wear for comfort or protection may also be so severe as to preclude the fitting of orthotic devices. Pressure sores of the hindfoot, lateral foot, and between the toes have led to development of osteomyelitis and amputation.
Besides the functional problems, foot deformities are of concern to the patient and family for physical appearance and social acceptance. Cognitive deficits, aggressive behavior, and other personality changes, often seen following TBI or CVA, further contribute to the difficulty in clinical assessment and treatment.
Clinical evaluation of motor impairment includes assessment of muscle tone, presence of patterned reflexes or volitional control, and development of clonus, rigidity, or fixed contractures. Assessment is made of motor strength, muscle phasic activity, and degree of flexibility, with active and passive range of motion. If spasticity is mild, quantitative evaluation of muscle strength can be assessed.
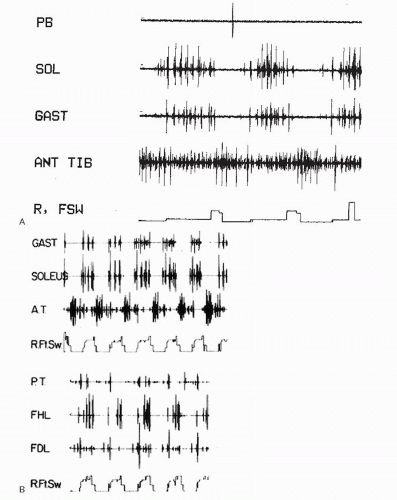
Dynamic electromyography (EMG) provides information on phasic muscle activity (Fig. 3.6). Electrical activity is recorded as the patient ambulates. The test shows the presence of normal (phasic), overactive (spastic), or silent (paralytic) activity. Dynamic EMG is particularly useful to evaluate activity of muscles difficult to assess by physical examination alone. It is useful in determining which muscles are contributing to a deformity, especially when multiple muscles may be responsible.
A fixed limb deformity may be caused by severe spasticity or by fixed soft-tissue contracture, which may be difficult to differentiate. Deformity caused by spasticity may exhibit clonus with sudden stretch or show some correction over a few minutes with prolonged stretch. Deformity caused by softtissue contracture does not show noticeable correction with passive stretch. Additional determination may be achieved with a lidocaine nerve block to the involved muscles with deformity caused by muscle spasticity improving after a block. Nerve blocks can be given to the femoral nerve for hip flexion, obturator nerve for hip adduction, and tibial nerve at the level of the knee for equinovarus and toe flexion.
Evaluation of the potential to ambulate, stand, or sit is an important aspect of the clinical assessment. Following a stroke, 20% to 30% of patients regain normal ambulation, and 75% return to some level of ambulation. Requirements for ambulation in an adult with acquired spastic hemiplegia include the following:
Voluntary hip flexion
Active hip flexion to 30 ° is usually required for limb advancement.
Occasionally, adductors can substitute for weak flexors to assist limb advancement, which is an important consideration before the release of the adductor muscles for hip adduction deformity.
Adequate sitting and standing balance
Patients often lean over the unaffected side to support the body with a cane held in the unaffected hand. Because of upper extremity involvement in hemiplegia, use of a walker is often not feasible.
The double limb support standing test popularized by Perry assesses balance by noting alignment of the trunk and the amount of spontaneous support given by the hemiplegic limb as the patient stands with the aid of a cane. Even with severe hemiparesis, a patient should be able to stand by shifting the body weight over to the unaffected side. Falling toward the hemiparetic side suggests a problem known as body neglect rather than limb disability as the cause of inability to ambulate.
Balance may also be impaired when there is loss of proprioception at the hip or knee.
Limb stability
Stability at the hip, knee, and ankle must be adequate to support body weight during stance phase.
Single limb stance on the hemiparetic limb is carefully tested, while protecting the patient in case of limb collapse.
Forward lean of the trunk implies weakness of the hip extensors. Flexion of the knee with ankle dorsiflexion may be indicative of soleus weakness. Knee flexion during stance also demonstrates good preservation of quadriceps strength, when the quadriceps are able to support the body weight on the flexed knee. Hyperextension of the knee usually indicates weakness of the quadriceps or occurs with an ankle equinus contracture.
Even though a patient may not be able to ambulate, standing is an important function for wheelchair transfers or dressing. Prerequisites for stable upright posture in stance are plantigrade feet and ankles, ability to extend the knee and hip, and adequate balance of the trunk, head, and neck.
Sensibility of the foot can be severely impaired following stroke or brain injury. Evaluation is performed with touch, pinprick, monofilament testing, and proprioception evaluation. Sensibility evaluation is often difficult in the patient with cognitive deficits who is unable to fully cooperate. Sensibility deficits add to the risk of skin breakdown.
Persistent extremity pain is a common sensory aberration following brain injury or stroke. Although poorly understood, this pain is often referred to as “pain of central origin”—characterized by diffuse, poorly localized, and at times severe leg or foot pain on the affected side. Ipsilateral upper extremity pain may also be present. Pain of central origin may represent a form of a complex regional pain syndrome (previously referred to as reflex sympathetic dystrophy) or a variant of other regional pain syndromes. Other causes of foot pain include muscle pain from chronic tension or chronic joint position from spasticity or contracture, joint subluxation from muscle imbalance, heterotopic
ossification (HO; seen in the hip or knee; rare in the foot and ankle), occult acute or stress fractures, and peripheral neuropathy from nerve stretch in a deformed limb. Pain in an extremity should be evaluated with appropriate examination, standard radiographs, and imaging and electrodiagnostic studies as appropriate. Testing for sympathetic nerve dysfunction includes lumbar sympathetic nerve blocks and triple-phase technetium bone scan. Suspected HO can be further assessed by technetium bone scan or by measuring serum alkaline phosphatase levels.
ossification (HO; seen in the hip or knee; rare in the foot and ankle), occult acute or stress fractures, and peripheral neuropathy from nerve stretch in a deformed limb. Pain in an extremity should be evaluated with appropriate examination, standard radiographs, and imaging and electrodiagnostic studies as appropriate. Testing for sympathetic nerve dysfunction includes lumbar sympathetic nerve blocks and triple-phase technetium bone scan. Suspected HO can be further assessed by technetium bone scan or by measuring serum alkaline phosphatase levels.
Body neglect is a clinical condition seen in TBI or CVA patients where a portion of the side of the patient’s body is not recognized. Evaluation is made by examining the hemiplegic patient during standing or attempted ambulation. Ambulation is difficult when the patient does not accommodate the weight of the unrecognized side. Patients often fail to look across their midline toward the affected side, and they have a tendency to lean or fall toward that side. Self-drawings sketched by these patients usually show omissions of extremities on the neglected side. Body neglect usually has a poor prognosis for ambulation.
Assessment of cognitive impairment of a patient with neuromuscular foot deformities is helpful in selecting those who are candidates for aggressive rehabilitation and in determining realistic goals, prognosis, and expectations. Cognitive abilities (in TBI and CVA) are evaluated by appropriateness of response to questions, ability to follow commands, psychological testing, and direct testing of learning ability in a rehabilitation setting. Decreased learning ability and loss of short-term memory may become apparent only with testing. Cognitive deficits may be severe in patients with frontal lobe injury who otherwise have few motor or sensory deficits. These patients show clinical features similar to senility, with lack of attention span and little motivation for recovery.
Aphasia is the loss of the ability to communicate. It may be expressive or receptive, and commonly occurs with lesions of the left cerebral cortex. Receptive aphasia has a poor prognosis for some aspects of rehabilitation (such as ambulation retraining) because the patient cannot understand instructions. Expressive aphasia, however, may be compatible with rehabilitation, if the patient is able to comprehend instructions.
Apraxia is the impairment of execution of a learned purposeful movement in the absence of motor impairment. It is characterized by a loss of ability to perform a routine task, such as tying shoelaces, ambulating, or using stairs. Apraxia occurs more often with right hemispheric involvement. The prognosis for ambulation with severe apraxia is usually poor.
Behavioral and psychological aberrations occur following CVA and TBI, including hostility, resentment, depression, withdrawal, or emotional instability. The behavior is often a reflection of premorbid personality traits, such as aggressive behavior. Psychiatric consultation assists evaluation. An understanding of premorbid states helps in coping with the difficult patient and establishing a functional prognosis from a psychological standpoint.
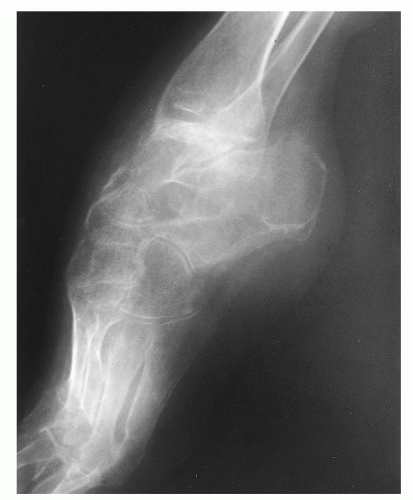
Radiologic Features
Standard AP, lateral, and oblique radiographs of the foot and ankle are usually obtained to assess and document the degree of deformity.
Weight-bearing views are often difficult and may require assistance from the radiologic technician to support or position the patient (Fig. 3.7).
Standard radiographs are also used to assess other skeletal causes of the deformity. These are particularly indicated if the patient has a rigid fixed deformity, has had prior operative procedures on the foot and ankle, or has sustained concomitant lower extremity skeletal trauma.
Standard radiographs of the hip and knee can establish the presence of neurogenic HO in fixed contractures. Neurogenic HO is rare in the foot and ankle, but relatively common in the hip and occasionally in the knee with TBI and SCI.
Computed axial tomography (CAT scan) is occasionally done for further evaluation if there is concomitant skeletal injury, if there is concern regarding integrity of joint surfaces, or if the patient has had previous operative procedures.
CT scans of the hip and knee are also helpful in establishing the three-dimensional extent of HO. Please confirm whether it should be CT or CAT scan in this instance
Three-phase technetium bone scans are helpful in establishing the presence of coexisting complex regional pain syndromes.
Technetium bone scans, along with serum alkaline phosphatase levels help establish the maturity or activity level of neurogenic HO.
MRI of the foot and ankle is seldom obtained in the patient with spasticity because it can be difficult
for the patient to remain still or to tolerate the test. An MRI is occasionally done if the integrity of specific soft tissues (such as tendons or ligaments) is in question.
Arteriograms of the limb can be obtained if integrity of the posterior tibial or dorsalis pedis artery is in question, especially when the patient has sustained previous trauma or has had prior operative procedures. Many adult patients with CP will have had several previous foot and ankle procedures in childhood.
TREATMENT
Nonsurgical Treatment
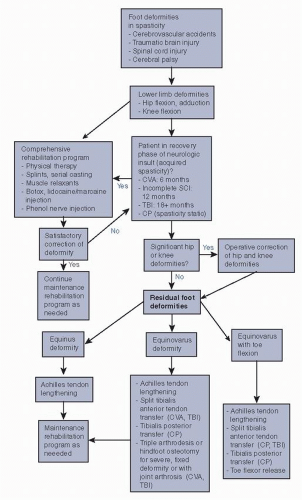
General rehabilitation strategies (Algorithm 3.1)
Initial treatment is usually nonoperative, especially when the patient is in the recovery phase of the neurologic insult (see Table 3.1).
Nonoperative treatment consists of a comprehensive rehabilitation program that usually includes physical
therapy, splinting or serial casting of deformities, muscle relaxants, and nerve blocks.
When nonsurgical efforts are not successful in preventing problematic contractures and the patient is beyond the period of neurologic recovery, operative management is considered.
Physical therapy
Physical therapy provides passive stretching, strengthening of weak antagonistic muscles, static splinting (including static progressive splinting), corrective or serial casting, biofeedback, functional retraining (for balance, stance, transfers, and ambulation), and desensitization of the painful limb.
Adjunct therapy includes functional electrical muscle stimulation and can be used to strengthen weak antagonist muscles, assist mobilization of the joints, and inhibit the spastic agonist.
Muscle relaxants
Baclofen, dantrolene sodium, and diazepam are common muscle relaxants that are effective initial methods for decreasing mildly spastic muscle tone.
Baclofen is usually given orally, but can be administered intrathecally when spasticity is severe.
Diazepam has potent muscle relaxant properties; however, side effects of lethargy and somnolence and the potential addictiveness make its use less optimal in many patients, especially when long-term therapy is needed.
These medications also have potential hepatotoxicity and warrant periodic liver function tests.
Mobilization, splinting, and orthoses
Mobilization and splinting provide the most important initial steps in a comprehensive rehabilitation program to treat spastic deformities.
Contractures do not develop in a joint that is passed through a full range of motion daily. Range of joint motion exercises that elongate shortened muscles should be performed several times daily.
In equinovarus deformities, stretching is performed by passive mobilization into maximal dorsiflexion and hindfoot valgus. Extending the knee during ankle mobilization further stretches the gastrocnemius. During Achilles tendon stretching for equinus, the hindfoot should be “locked” by placing the foot in inversion to prevent midfoot collapse and resulting in a rocker bottom foot. The stretching should be gentle, prolonged, and maintained. A “stretch and hold” method is an effective method, commonly used by physical and occupational therapists.
Muscle strengthening with active motion against resistance is incorporated when there is adequate volitional control.
The ankle is maintained in proper position by static splinting with well-padded bivalved casts, molded splints, or static ankle—foot orthoses (AFOs; Fig. 3.8). The double-upright metal and leather AFO is often needed for the more severe spasticity; the lightweight synthetic AFO is feasible when spasticity is mild. The well-padded “boot” type orthoses are also effective and readily available in several sizes to fit the patient.
Toe flexion deformities can be minimized with daily stretching and maintained by the incorporation of a well-padded toe plate into the AFO.
Static splints and “inhibitive casts” also decrease spastic muscle tone by decreasing motion, which lessens stimulation to the stretch reflex and, in turn, decreases spasticity.
Dynamic splints or traction devices must be used with caution in the spastic limb because the continuous stretch may provide stimulation that increases spasticity or perpetuates clonus.
Several commercial dynamic splints are available for ankle and knee deformities, allowing a set amount of traction to be placed across a joint.
Dynamic splints are usually more effective when a fixed contracture exists but spasticity is minimal. Even though they are well designed and well padded, these devices must be closely monitored for pressure areas or potential skin breakdown, especially when contractures are severe.
Serial casting
If a fixed joint contracture has developed, serial casting can be an effective means of slowly stretching soft tissues to correct a deformity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree