Chapter 68 Nerve Injuries
This chapter includes the essentials of treatment of nerve injuries in the digits, palm, and wrist. Although many of the principles discussed here can be applied to injuries in the forearm and arm, more detailed discussions of more proximal nerve injuries can be found in Chapter 62 on peripheral nerve injuries. Nerve entrapments and compression neuropathies also are discussed in detail in Chapter 62. Reconstructive procedures including tendon transfers are discussed in Chapter 34, and an expansion of the discussion of microsurgical technique can be found in Chapter 63.
Evaluation
Preoperative Assessment
Type of Injury
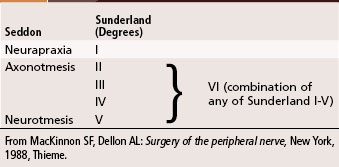
Nerve injuries seen in a civilian practice commonly are caused by one of several mechanisms, including direct trauma (blow to the limb, fracture, missile wound), laceration, traction or stretching, and entrapment or compression. To help determine the type of treatment and to arrive at tentative prognostic projections, it is helpful to recall the classification of nerve injuries according to Seddon and Sunderland (Table 68-1). Common injuries such as bumping the “funny bone” (ulnar nerve at the elbow) fall easily into the category of neurapraxia (type I injuries), and lacerations are classified as neurotmesis (type V injuries); however, closed injuries with partial nerve deficits are not classified as easily, and the prognosis may not be as well defined. The extent to which the nature of the injuring agent determines primary and secondary repair is discussed in this chapter under their respective headings. Additional discussion of extent of injury may be found in Chapter 62.
TABLE 68-1 Classification of Nerve Injury
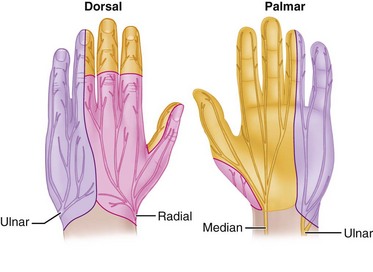
From MacKinnon SF, Dellon AL: Surgery of the peripheral nerve, New York, 1988, Thieme.
Sensibility Evaluation
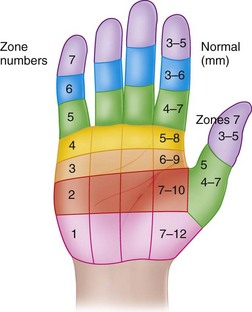
When evaluating the injured hand for sensibility, in addition to an awareness of the classic sensory distribution of the median, radial, and ulnar nerves (Fig. 68-1), it is helpful to recall the autonomous sensory distributions of the median, radial, and ulnar nerves in the volar pulp of the index finger, the volar pulp of the little finger, and the thumb-index web space. If the injury is a laceration, and the nerve has been transected, the examination usually is more definitive than in closed injuries or in lacerations in which the depth may not be fully known. Even if a wound is to be explored to determine the extent of the nerve injury, it is helpful to document the clinical deficit before surgical exploration. Careful evaluation, especially in the presence of a closed injury, defines the initial deficit, allowing for assessment of progress if observation of the injury is elected rather than exploration of the nerve. Closed partial rupture of a common digital nerve in the palm requiring MRI and surgical exploration for diagnosis was described. The customary methods used to evaluate damaged sensory nerves include the use of a sharp pin to assess pain, a cotton-tipped applicator or a finger eraser to assess light touch, and the tips of a paper clip or commercially prepared tool to assess two-point discrimination. Normal two-point discrimination usually is 6 mm or less. If the nerve is transected, a patient would not feel light touch, would not appreciate the pin as a sharp stimulus, and would be unable to discriminate between one and two points. Patients with closed injuries or partial injuries to nerves may show spotty appreciation of light touch and pain and have markedly widened two-point discrimination (Fig. 68-2).
Motor Function
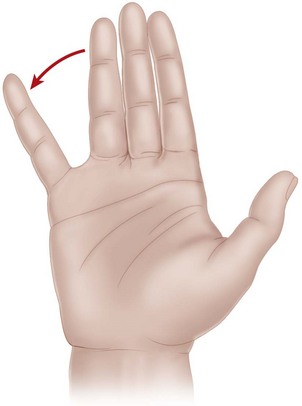
The muscles proximally innervated by the ulnar nerve include the flexor carpi ulnaris and flexor digitorum profundus tendons to the ring and little fingers. In the hand, the ulnar-innervated muscles of interest include the flexor pollicis brevis, adductor pollicis, abductor digiti minimi, flexor digiti minimi, opponens digiti minimi, and all the interosseous muscles. When testing for motor function of the ulnar nerve in the hand, the usual motions mediated by the ulnar intrinsic muscles include active abduction of the middle finger from the ulnar to the radial side with the palm resting on a flat surface. This motion should be observed carefully to exclude the functions of the long flexor tendons, which tend to converge the digits and confuse accurate interpretation of the function of the volar interosseous muscles, and the long extensor tendons, which tend to diverge the fingers and confuse accurate interpretation of the dorsal interosseous muscles. Additionally, thumb adduction usually is tested by having the patient maintain a piece of paper tightly in the thumb-index web, squeezing the paper between the thumb interphalangeal joint and the base of the index finger proximal phalanx. If the adductor is weak or paralyzed, the patient is unable to hold the piece of paper against resistance. The function of the abductor digiti minimi also may be tested by having the patient abduct the little finger against resistance and by palpating the muscle belly of the abductor digiti minimi (Fig. 68-3). Although clawing of the little and ring fingers may not be seen at the time of an acute injury, it is present sometimes, and careful observation of the hand should reveal this finding. The first dorsal interosseous muscle may receive an anomalous innervation from the median nerve in about 10% of hands. The posterior interosseous or superficial branches of the radial nerve also may supply the first dorsal and the second and third dorsal interosseous muscles in some hands.
Postoperative Assessment
Sensibility Evaluation
Two-Point and Moving Two-Point Discrimination Testing
 The hand should be warm, and the instrument should be at room temperature.
The hand should be warm, and the instrument should be at room temperature.
 Rest the hand on a flat surface, palm up.
Rest the hand on a flat surface, palm up.
 Apply a blunt, two-pointed caliper or paper clip distally over the distal pulp in the longitudinal axis on the radial or ulnar side (Fig. 68-4). The pressure applied should be just slightly less than blanching pressure. Test each area three times. Start at a width of 10 mm, and gradually decrease the distance.
Apply a blunt, two-pointed caliper or paper clip distally over the distal pulp in the longitudinal axis on the radial or ulnar side (Fig. 68-4). The pressure applied should be just slightly less than blanching pressure. Test each area three times. Start at a width of 10 mm, and gradually decrease the distance.
 Perform the moving two-point discrimination test in a similar fashion. Apply the caliper in an axial direction, and move it from proximal to distal along the digital pad. Two of three correct answers are considered proof of perception with either test.
Perform the moving two-point discrimination test in a similar fashion. Apply the caliper in an axial direction, and move it from proximal to distal along the digital pad. Two of three correct answers are considered proof of perception with either test.
Nerve Regeneration
After a nerve injury, the response in the proximal elements of the peripheral nerve includes an increased rate of metabolic activity and proliferation from the nerve cell bodies distally, resulting in the sprouting of axonal processes at the injury site within the first 1 to 3 weeks. The response distally consists of the elements of wallerian degeneration, including disruption of the myelin sheath and phagocytosis, and preparation of the distal segment to receive the regenerating elements of the proximal axons. A more detailed discussion of this response is presented in Chapter 62.
Suturing of Nerves
For additional discussion of surgical techniques, see Chapter 62 on peripheral nerve injuries and Chapter 63 on microsurgery. Generally, the principles that apply to the suture of other peripheral nerves also apply to suturing of the peripheral nerves of the hand. Important considerations include (1) mixed versus pure motor or sensory nerves, (2) internal arrangement of the nerves, (3) incisions to be used, (4) amount of mobilization and limb positioning required for tension-free apposition, (5) suture materials to be used, (6) nature of the suture arrangement, (7) magnification, and (8) postoperative management.
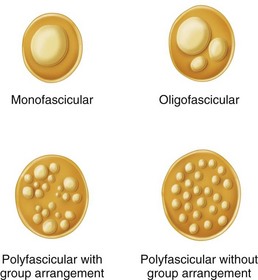
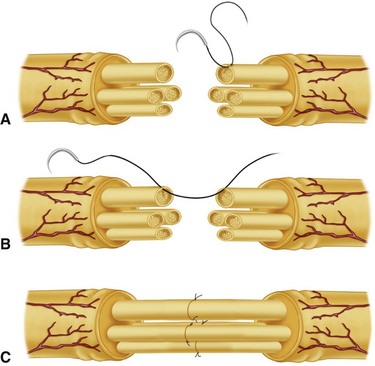
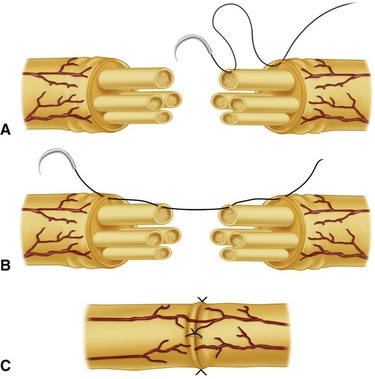
Careful technique is crucial to provide the best restoration and repair of the anatomy. The internal arrangement of the nerve in the palm and digits usually is oligofascicular as described by Millesi (Fig. 68-5). In the median and ulnar nerves at the wrist, an intraneural polyfascicular or group arrangement is found. The outlook is better after repair of common digital and proper digital nerves because of their internal arrangement, their pure sensory function, and the short distance from the injury to the end organ.
Incisions to expose the nerve and mobilize the nerve proximally and distally should be made in accordance with proven principles of skin incisions in the palm. They should not cross flexion creases at right angles, skin flaps should not be devascularized, and additional neurovascular injury should not be created in extending the skin incisions. The exact extent to which a nerve can be mobilized without creating ischemia is unknown. Generally, within the digits, palm, and wrist, extensive mobilization of the nerve from its surrounding tissues is insufficient to cause harm. Magnification is extremely helpful to permit the most precise and accurate restoration of the anatomy. In the palm and fingers, the magnification achieved by 2.5× to 4.5× magnifying loupes usually is sufficient to allow accurate repair. More proximally, magnification achieved with an operating microscope is more helpful in allowing satisfactory anatomical repair. The operating microscope also may be extremely helpful in repair of the terminal branches of the proper digital nerves distal to the distal flexion crease of the finger. Suture materials reflect the amount of tension to be applied to the nerve repair. Generally, in the forearm, wrist, and hand, 8-0 and 9-0 monofilament nylon sutures are used. Usually in the palm and digits, a repair using a pure perineurial neurorrhaphy (fascicular) (Fig. 68-6) or a combination epiperineurial-perineurial neurorrhaphy (Fig. 68-7) is sufficient for satisfactory anatomical repair.