Chapter 5 Arthrodesis of the Hip
Techniques
Arthrodesis with Cancellous Screw Fixation
 Through an anterolateral approach, perform an anterior capsulotomy.
Through an anterolateral approach, perform an anterior capsulotomy.
 Dislocate the femoral head and denude both sides of the joint of articular cartilage and necrotic bone.
Dislocate the femoral head and denude both sides of the joint of articular cartilage and necrotic bone.
 Place the leg in a position that allows maximal contact between the femoral head and acetabulum, and insert one or two cancellous screws into the inner surface of the ilium to engage the femoral head.
Place the leg in a position that allows maximal contact between the femoral head and acetabulum, and insert one or two cancellous screws into the inner surface of the ilium to engage the femoral head.
 Before tightening the screws to compress the femoral head into the acetabulum, perform an intertrochanteric osteotomy to decompress the long lever arm of the femur.
Before tightening the screws to compress the femoral head into the acetabulum, perform an intertrochanteric osteotomy to decompress the long lever arm of the femur.
Arthrodesis with Cobra Plate Fixation
 Place the patient supine with a sandbag under the ipsilateral buttock. Prepare and drape both lower extremities and anterior superior iliac spines to allow access to both iliac crests and both ankles.
Place the patient supine with a sandbag under the ipsilateral buttock. Prepare and drape both lower extremities and anterior superior iliac spines to allow access to both iliac crests and both ankles.
 Make a linear longitudinal midlateral incision along the femoral diaphysis to a point 8 cm distal to the tip of the greater trochanter (Fig. 5-1A).
Make a linear longitudinal midlateral incision along the femoral diaphysis to a point 8 cm distal to the tip of the greater trochanter (Fig. 5-1A).
 Open the fascia lata in line with its fibers for the length of the wound; identify and protect the sciatic nerve throughout the procedure.
Open the fascia lata in line with its fibers for the length of the wound; identify and protect the sciatic nerve throughout the procedure.
 Maintain exposure with a self-retaining retractor. Incise the origin of the vastus lateralis, and reflect it off the greater trochanteric flair and the linea aspera for a distance of 6 cm.
Maintain exposure with a self-retaining retractor. Incise the origin of the vastus lateralis, and reflect it off the greater trochanteric flair and the linea aspera for a distance of 6 cm.
 Identify the anterior and posterior margins of the gluteus medius.
Identify the anterior and posterior margins of the gluteus medius.
 Use an oscillating saw to make a greater trochanteric osteotomy so that the proximal fragment includes the insertion of the gluteus medius and minimus (Fig. 5-1B).
Use an oscillating saw to make a greater trochanteric osteotomy so that the proximal fragment includes the insertion of the gluteus medius and minimus (Fig. 5-1B).
 Elevate the hip abductors with the greater trochanteric fragment, and hold them superiorly with two large Steinmann pins hammered into the iliac wing (Fig. 5-1C).
Elevate the hip abductors with the greater trochanteric fragment, and hold them superiorly with two large Steinmann pins hammered into the iliac wing (Fig. 5-1C).
 Perform a superior hip capsulotomy.
Perform a superior hip capsulotomy.
 Elevate the periosteum of the outer table of the iliac wing superiorly to the retracting Steinmann pins, anteriorly to the anterior superior iliac spine and the anterior inferior iliac spine, and posteriorly to the sciatic notch.
Elevate the periosteum of the outer table of the iliac wing superiorly to the retracting Steinmann pins, anteriorly to the anterior superior iliac spine and the anterior inferior iliac spine, and posteriorly to the sciatic notch.
 Place one blunt Hohmann retractor in the sciatic notch subperiosteally to protect the sciatic nerve and the superior gluteal artery and one anterior to the iliopectineal eminence.
Place one blunt Hohmann retractor in the sciatic notch subperiosteally to protect the sciatic nerve and the superior gluteal artery and one anterior to the iliopectineal eminence.
 Make a transverse innominate osteotomy between the iliopectineal eminence and the sciatic notch at the superior pole of the acetabulum.
Make a transverse innominate osteotomy between the iliopectineal eminence and the sciatic notch at the superior pole of the acetabulum.
 Remove a corresponding 0.5-cm wafer of bone from the superior pole of the femoral head.
Remove a corresponding 0.5-cm wafer of bone from the superior pole of the femoral head.
 Make the iliac cut with an oscillating saw, and complete it with an osteotome. Use osteotomes and curets to remove any remaining cartilage and sclerotic cortical bone from the superior weight-bearing surface of the femoral head and from the acetabulum.
Make the iliac cut with an oscillating saw, and complete it with an osteotome. Use osteotomes and curets to remove any remaining cartilage and sclerotic cortical bone from the superior weight-bearing surface of the femoral head and from the acetabulum.
 Displace the distal hemipelvic fragment and the proximal femur medially 100% of the thickness of the innominate bone by placing a curved, blunt instrument in the osteotomy and levering the distal hemipelvis 1 cm.
Displace the distal hemipelvic fragment and the proximal femur medially 100% of the thickness of the innominate bone by placing a curved, blunt instrument in the osteotomy and levering the distal hemipelvis 1 cm.
 Remove the sandbag and place a Steinmann pin into each of the anterior superior iliac spines; use the pins and a long-limbed protractor to determine adduction and abduction of the limb.
Remove the sandbag and place a Steinmann pin into each of the anterior superior iliac spines; use the pins and a long-limbed protractor to determine adduction and abduction of the limb.
 Evaluate internal and external rotation by observing the patella and the malleoli relative to the two vertical Steinmann pins.
Evaluate internal and external rotation by observing the patella and the malleoli relative to the two vertical Steinmann pins.
 Position the hip in 25 degrees of flexion, neutral internal and external rotation, and neutral adduction and abduction.
Position the hip in 25 degrees of flexion, neutral internal and external rotation, and neutral adduction and abduction.
 Contour a nine-hole cobra plate, and secure the proximal portion to the ilium with a 4.5-mm cortical screw.
Contour a nine-hole cobra plate, and secure the proximal portion to the ilium with a 4.5-mm cortical screw.
 Test hip flexion with the Thomas test.
Test hip flexion with the Thomas test.
 Distal to the plate, attach an AO tensioner to the lateral femoral cortex with a single unicortical 4.5-mm cortical screw (Fig. 5-1D).
Distal to the plate, attach an AO tensioner to the lateral femoral cortex with a single unicortical 4.5-mm cortical screw (Fig. 5-1D).
 Insert a screw in the most distal hole of the plate, hook the tensioner to the plate, and apply compression force across the hip joint to ensure good bony apposition.
Insert a screw in the most distal hole of the plate, hook the tensioner to the plate, and apply compression force across the hip joint to ensure good bony apposition.
 Secure the plate to the lateral femur with 4.5-mm bicortical screws in eight of the nine holes, and remove the tensioner.
Secure the plate to the lateral femur with 4.5-mm bicortical screws in eight of the nine holes, and remove the tensioner.
 Insert 4.5-mm cortical screws in the proximal plate, taking care to protect the neurovascular structures on the inner table of the pelvis.
Insert 4.5-mm cortical screws in the proximal plate, taking care to protect the neurovascular structures on the inner table of the pelvis.
 Remove the retractors and the Steinmann pins holding the greater trochanter, and drill a 4.5-mm hole in the center of the proximal greater trochanteric fragment.
Remove the retractors and the Steinmann pins holding the greater trochanter, and drill a 4.5-mm hole in the center of the proximal greater trochanteric fragment.
 Drill and tap a 3.2-mm bicortical screw in the proximal femur through the third or fourth hole of the cobra plate.
Drill and tap a 3.2-mm bicortical screw in the proximal femur through the third or fourth hole of the cobra plate.
 Reattach the greater trochanter with a 4.5-mm cortical screw and washer (Fig. 5-1E and F). A trochanteric grip plate with wires may provide superior fixation if necessary.
Reattach the greater trochanter with a 4.5-mm cortical screw and washer (Fig. 5-1E and F). A trochanteric grip plate with wires may provide superior fixation if necessary.
 Pack any remaining corticocancellous bone around the hip joint, and obtain an anteroposterior pelvic radiograph to check the position of the plate, screws, and hip joint (Fig. 5-1G).
Pack any remaining corticocancellous bone around the hip joint, and obtain an anteroposterior pelvic radiograph to check the position of the plate, screws, and hip joint (Fig. 5-1G).
 Thoroughly irrigate the wound, and close the soft tissue in layers over drains.
Thoroughly irrigate the wound, and close the soft tissue in layers over drains.
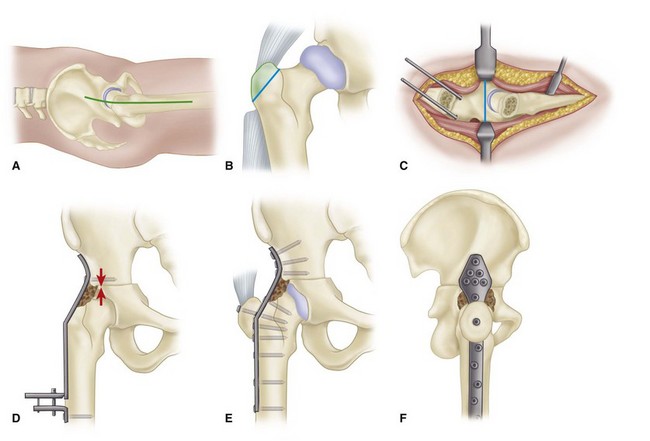
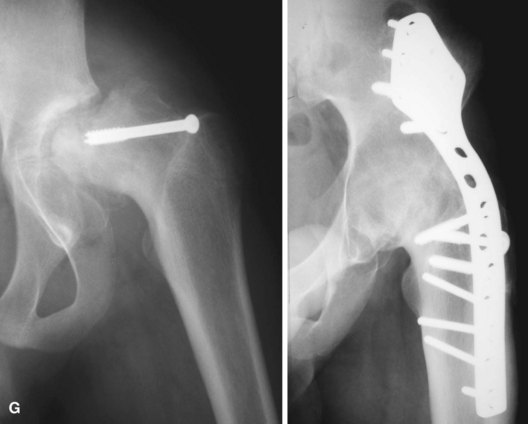
Figure 5-1 Hip arthrodesis with cobra plate fixation (see text). A, Longitudinal midlateral incision. B, Osteotomy of greater trochanter. C, Transverse innominate osteotomy. D, Cobra plate contoured and attached with two screws for application of compression force. E, Final fixation of plate. F, Lateral view of plate and reattachment of greater trochanter. G, Hip fusion with cobra plate. SEE TECHNIQUE 5-2.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









