Chapter 80 Surgical Techniques
Surgical Techniques
Preoperative Preparation
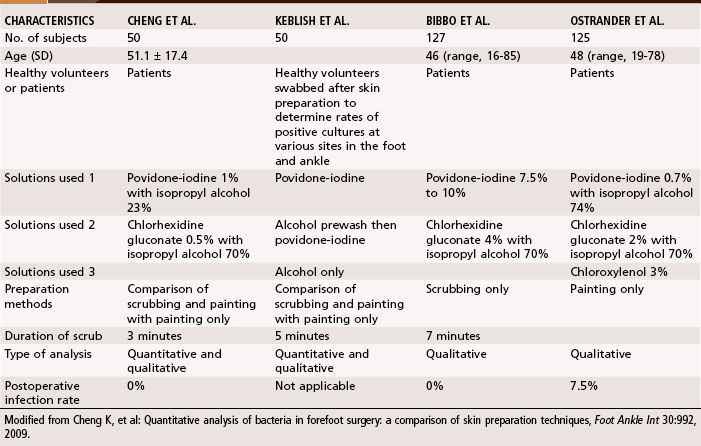
Because of the normal bacterial flora residing on the foot, particularly in the web spaces, which often are moist because of confinement in hosiery and shoes, the extremity to be operated on is scrubbed for 8 to 10 minutes from toes to knee with an antibacterial soap of the surgeon’s choice that the patient’s skin can tolerate. Particular attention is directed to the web spaces. After this cleansing, the extremity is wrapped sterilely with a cloth that is secured with a gauze wrap. This is not removed until the patient is on the operating table, at which time the skin is prepared again with an antiseptic solution. Goucher and Coughlin, however, found no benefit in covering the toes during hindfoot or ankle surgery after skin preparation with chlorhexidine gluconate and isopropyl alcohol. Only two of 40 patients had positive cultures after surgery, and neither developed an infection. Forefoot procedures are worrisome because of the high bacterial counts between the toes. Bacteria resides in colonies between the stratum corneum, in the follicles of the sebaceous glands, and in the hair. Presently, no consensus has been reached for the best skin preparation in foot and ankle surgery, although several studies have compared different types of solutions and preparation methods (Table 80-1). Quantitative analysis of positive cultures have shown significant reductions in heavy bacterial growth when bristled brushes are used with povidone-iodine and isopropyl alcohol.
Tourniquet
Application of a Tourniquet
 Have an assistant hold the end of the wrap at 45 degrees to the foot, placing tension on the free end, while the surgeon’s thumb holds the wrap firmly against the skin.
Have an assistant hold the end of the wrap at 45 degrees to the foot, placing tension on the free end, while the surgeon’s thumb holds the wrap firmly against the skin.
 Do not overlap each turn more than half the width of the tourniquet. Wrap the tourniquet above the ankle, being careful not to leave any skin uncovered and not to allow the edges to roll on themselves.
Do not overlap each turn more than half the width of the tourniquet. Wrap the tourniquet above the ankle, being careful not to leave any skin uncovered and not to allow the edges to roll on themselves.
 When above the ankle, proceed proximally, no more than 8 to 10 cm proximal to the malleoli, staying distal to the muscle mass. Do not go more proximally because this would increase the discomfort caused by the tourniquet.
When above the ankle, proceed proximally, no more than 8 to 10 cm proximal to the malleoli, staying distal to the muscle mass. Do not go more proximally because this would increase the discomfort caused by the tourniquet.
 Complete the exsanguination with no more than three or four “cinches” around the ankle, followed by a tuck.
Complete the exsanguination with no more than three or four “cinches” around the ankle, followed by a tuck.
Anesthesia
Forefoot Block
Forefoot Block
 Palpate the dorsalis pedis artery as it reaches the first intermetatarsal space (Fig. 80-1A). The deep peroneal nerve to the first web space accompanies this artery.
Palpate the dorsalis pedis artery as it reaches the first intermetatarsal space (Fig. 80-1A). The deep peroneal nerve to the first web space accompanies this artery.
 Using a 25-gauge needle and, avoiding the artery, inject 2 to 3 mL of a mixture of short-acting and long-acting local anesthetic agents subcutaneously.
Using a 25-gauge needle and, avoiding the artery, inject 2 to 3 mL of a mixture of short-acting and long-acting local anesthetic agents subcutaneously.
 If a second or third hammer toe procedure is planned, direct the needle laterally just beneath the dorsal veins from the same entrance point and block the common digital branches of the superficial peroneal nerve to the second (and, if needed, the third) intermetatarsal space (Fig. 80-1B). Injection of another 2 to 3 mL should be enough.
If a second or third hammer toe procedure is planned, direct the needle laterally just beneath the dorsal veins from the same entrance point and block the common digital branches of the superficial peroneal nerve to the second (and, if needed, the third) intermetatarsal space (Fig. 80-1B). Injection of another 2 to 3 mL should be enough.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree