Chapter 17 Amputations of the Hip and Pelvis
Disarticulation of the Hip
Anatomical Hip Disarticulation
 With the patient in the lateral decubitus position, make an anterior racquet-shaped incision (Fig. 17-1A), beginning the incision at the anterior superior iliac spine and curving it distally and medially almost parallel with the inguinal ligament to a point on the medial aspect of the thigh 5 cm distal to the origin of the adductor muscles. Isolate and ligate the femoral artery and vein, and divide the femoral nerve; continue the incision around the posterior aspect of the thigh about 5 cm distal to the ischial tuberosity and along the lateral aspect of the thigh about 8 cm distal to the base of the greater trochanter. From this point, curve the incision proximally to join the beginning of the incision just inferior to the anterior superior iliac spine.
With the patient in the lateral decubitus position, make an anterior racquet-shaped incision (Fig. 17-1A), beginning the incision at the anterior superior iliac spine and curving it distally and medially almost parallel with the inguinal ligament to a point on the medial aspect of the thigh 5 cm distal to the origin of the adductor muscles. Isolate and ligate the femoral artery and vein, and divide the femoral nerve; continue the incision around the posterior aspect of the thigh about 5 cm distal to the ischial tuberosity and along the lateral aspect of the thigh about 8 cm distal to the base of the greater trochanter. From this point, curve the incision proximally to join the beginning of the incision just inferior to the anterior superior iliac spine.
 Detach the sartorius muscle from the anterior superior iliac spine and the rectus femoris from the anterior inferior iliac spine, and reflect them both distally.
Detach the sartorius muscle from the anterior superior iliac spine and the rectus femoris from the anterior inferior iliac spine, and reflect them both distally.
 Divide the pectineus about 0.6 cm from the pubis.
Divide the pectineus about 0.6 cm from the pubis.
 Rotate the thigh externally to bring the lesser trochanter and the iliopsoas tendon into view; divide the latter at its insertion and reflect it proximally.
Rotate the thigh externally to bring the lesser trochanter and the iliopsoas tendon into view; divide the latter at its insertion and reflect it proximally.
 Detach the adductor and gracilis muscles from the pubis, and divide at its origin that part of the adductor magnus that arises from the ischium.
Detach the adductor and gracilis muscles from the pubis, and divide at its origin that part of the adductor magnus that arises from the ischium.
 Develop the muscle plane between the pectineus and obturator externus and short external rotators of the hip to expose the branches of the obturator artery. Clamp, ligate, and divide the branches at this point. Later in the operation the obturator externus muscle is divided at its insertion on the femur instead of at its origin on the pelvis because otherwise the obturator artery may be severed and might retract into the pelvis, leading to hemorrhage that could be difficult to control.
Develop the muscle plane between the pectineus and obturator externus and short external rotators of the hip to expose the branches of the obturator artery. Clamp, ligate, and divide the branches at this point. Later in the operation the obturator externus muscle is divided at its insertion on the femur instead of at its origin on the pelvis because otherwise the obturator artery may be severed and might retract into the pelvis, leading to hemorrhage that could be difficult to control.
 Rotate the thigh internally, and detach the gluteus medius and minimus muscles from their insertions on the greater trochanter and retract them proximally.
Rotate the thigh internally, and detach the gluteus medius and minimus muscles from their insertions on the greater trochanter and retract them proximally.
 Divide the fascia lata and the most distal fibers of the gluteus maximus muscle distal to the insertion of the tensor fasciae latae muscle in the line of the skin incision, and separate the tendon of the gluteus maximus from its insertion on the linea aspera. Reflect this muscle mass proximally.
Divide the fascia lata and the most distal fibers of the gluteus maximus muscle distal to the insertion of the tensor fasciae latae muscle in the line of the skin incision, and separate the tendon of the gluteus maximus from its insertion on the linea aspera. Reflect this muscle mass proximally.
 Identify, ligate, and divide the sciatic nerve.
Identify, ligate, and divide the sciatic nerve.
 Divide the short external rotators of the hip (i.e., the piriformis, gemelli, obturator internus, obturator externus, and quadratus femoris) at their insertions on the femur, and sever the hamstring muscles from the ischial tuberosity.
Divide the short external rotators of the hip (i.e., the piriformis, gemelli, obturator internus, obturator externus, and quadratus femoris) at their insertions on the femur, and sever the hamstring muscles from the ischial tuberosity.
 Incise the hip joint capsule and the ligamentum teres to complete the disarticulation (Fig. 17-1B).
Incise the hip joint capsule and the ligamentum teres to complete the disarticulation (Fig. 17-1B).
 Bring the gluteal flap anteriorly, and suture the distal part of the gluteal muscles to the origin of the pectineus and adductor muscles.
Bring the gluteal flap anteriorly, and suture the distal part of the gluteal muscles to the origin of the pectineus and adductor muscles.
 Place a drain in the inferior part of the incision, and approximate the skin edges with interrupted nonabsorbable sutures.
Place a drain in the inferior part of the incision, and approximate the skin edges with interrupted nonabsorbable sutures.
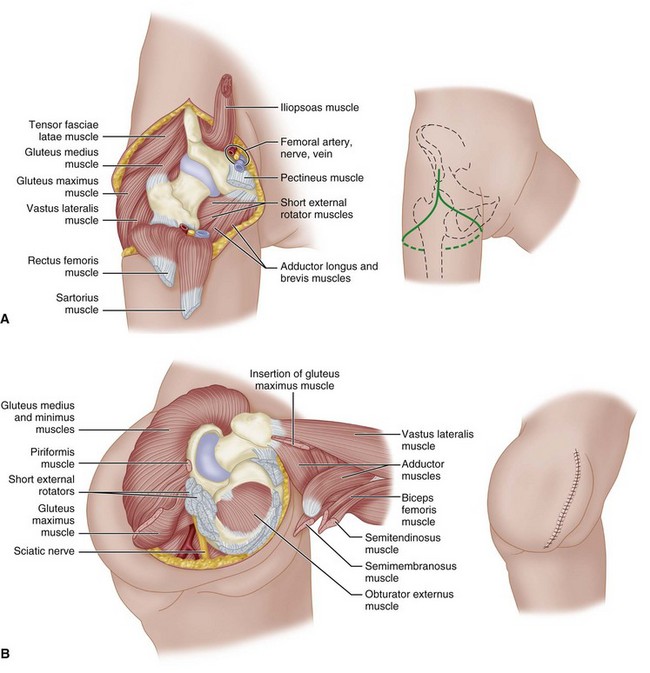
FIGURE 17-1 Boyd disarticulation of hip. A, Femoral vessels and nerve have been ligated, and sartorius, rectus femoris, pectineus, and iliopsoas muscles have been detached. Inset, Line of skin incision. B, Gluteal muscles have been separated from insertions, sciatic nerve and short external rotators have been divided, and hamstring muscles have been detached from ischial tuberosity. Inset, Final closure of stump. SEE TECHNIQUE 17-1.
(Redrawn from Boyd HB: Anatomic disarticulation of the hip, Surg Gynecol Obstet 84:346, 1947.)
Posterior Flap
 Begin the incision at the level of the inguinal ligament, carry it distally over the femoral artery for 10 cm, curve it along the medial aspect of the thigh, continue it laterally and proximally over the greater trochanter, and swing it anteriorly to the starting point. A posteromedial flap long enough to cover the end of the stump is formed.
Begin the incision at the level of the inguinal ligament, carry it distally over the femoral artery for 10 cm, curve it along the medial aspect of the thigh, continue it laterally and proximally over the greater trochanter, and swing it anteriorly to the starting point. A posteromedial flap long enough to cover the end of the stump is formed.
 Isolate, ligate, and divide the femoral vessels, and section the femoral nerve to fall well proximal to the inguinal ligament.
Isolate, ligate, and divide the femoral vessels, and section the femoral nerve to fall well proximal to the inguinal ligament.
 Abduct the thigh widely, and divide the adductor muscles at their pubic origins.
Abduct the thigh widely, and divide the adductor muscles at their pubic origins.
 Section the two branches of the obturator nerve so that they retract away from pressure areas.
Section the two branches of the obturator nerve so that they retract away from pressure areas.
 Free the origins of the sartorius and rectus femoris from the anterior superior and anterior inferior iliac spines. Moderately adduct and internally rotate the thigh, and divide the tensor fasciae latae at the level of the proximal end of the greater trochanter; at the same level, divide close to bone the muscles attached to the trochanter. Next, abduct the thigh markedly and divide the gluteus maximus at the distal end of the posterior skin flap.
Free the origins of the sartorius and rectus femoris from the anterior superior and anterior inferior iliac spines. Moderately adduct and internally rotate the thigh, and divide the tensor fasciae latae at the level of the proximal end of the greater trochanter; at the same level, divide close to bone the muscles attached to the trochanter. Next, abduct the thigh markedly and divide the gluteus maximus at the distal end of the posterior skin flap.
 Identify, ligate, and divide the sciatic nerve.
Identify, ligate, and divide the sciatic nerve.
 Divide the joint capsule, and complete the disarticulation.
Divide the joint capsule, and complete the disarticulation.
 Swing the long posteromedial flap containing the gluteus maximus anteriorly, and suture it to the anterior margins of the incision.
Swing the long posteromedial flap containing the gluteus maximus anteriorly, and suture it to the anterior margins of the incision.
Hemipelvectomy
The standard hemipelvectomy employs a posterior or gluteal flap and disarticulates the symphysis pubis and sacroiliac joint and the ipsilateral limb. An extended hemipelvectomy includes resection of adjacent musculoskeletal structures, such as the sacrum or parts of the lumbar spine. In a conservative hemipelvectomy, the bony section divides the ilium above the acetabulum, preserving the crest of the ilium. Internal hemipelvectomy is a limb-sparing resection, often achieving proximal and medial margins equal to the corresponding amputation. This procedure is discussed in Chapter 24.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








