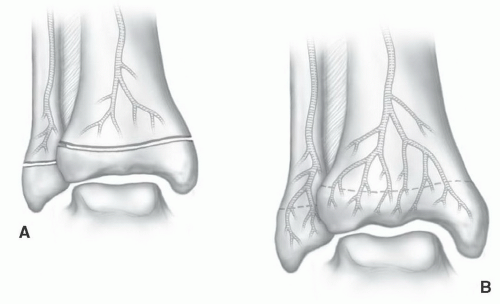
Osteomyelitis presents a diagnostic and therapeutic challenge regardless of the age group. Early diagnosis and management are essential to avoid irreversible bone, joint, and soft tissue damage. Hematogenous osteomyelitis, which occurs more commonly in children than adults, may be acute, subacute, or chronic, and most commonly involves the long bones of the lower extremities. In infants (<2 years) and adults, the epiphysis is not protected; vascular channels cross the growth plate allowing infection to involve both the metaphysis and epiphysis with a high incidence of joint space involvement.
10,15 In patients aged from 1 to 2 years up to 16 years, the growth plate prevents spread of infection to the epiphysis and joint space involvement is less common unless the metaphysis is intracapsular (
Fig. 13.1).
12Infections typically involve the metaphyseal portion of long bones or areas near the physis in flat bones, such as the ilium. Radiologic changes are nonspecific in the early stages of infection. Localized swelling and distortion of the tissue planes may be the only findings.
6,7 This may be followed with osteopenia in the area of marrow involvement or subtle lytic areas in the cortex. More defined bone destruction is usually not appreciated until 35% to 40% of the involved bone is destroyed, and thus is generally not evident for 10 to 14 days.
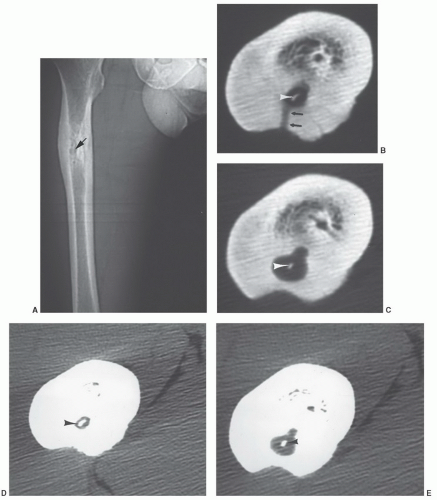
10,12 Periosteal elevation may also be evident. The degree of involvement is often underestimated on routine radiographs. In this situation, computed tomography (CT) may be useful to more clearly define the extent of involvement. CT (
Fig. 13.3) has been especially useful in determining the extent of disease prior to planning operative therapy and for detection of sequestra, cloaca (
Table 13.1), and soft tissue changes.
6,7,8,11,34,51Radioisotope studies provide a sensitive tool for early detection of osteomyelitis. Technetium-99m, indium-111 labeled leukocytes, and technetium white cells or antigranulocyte antibodies provide sensitive and fairly specific methods for diagnosis of infection.
2,6,7,13,27,38,52 However, the anatomic extent may be inaccurate, especially in the articular regions, and differentiation of soft tissue from bone involvement is not always possible.
7 Also, in complex clinical settings such as previous surgery or instrumentation, neurotrophic changes or other conditions that create bone remodeling radionuclide imaging is less specific.
16,53 This will be discussed in detail later in this chapter.
Acute Osteomyelitis
MRI is particularly suited to evaluate osteomyelitis due to superior soft tissue contrast and multiple image plane capabilities. Anatomic detail is superior to that provided by isotope studies. Subtle bone and soft tissue changes are more easily appreciated than on radiographs or CT examinations.
3,4,51,52,53,54,55 In recent years, new pulse sequences, including diffusion-weighted imaging and the use of intravenous contrast have improved the utility of MRI for evaluating infection.
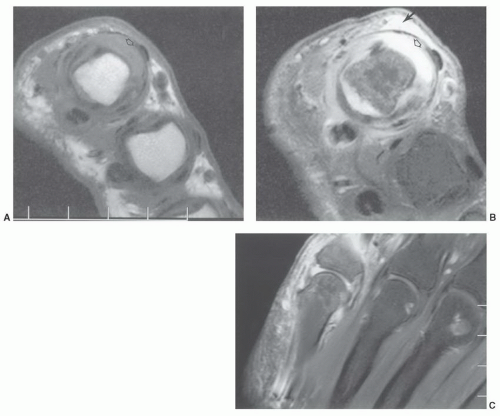
53,55As with other musculoskeletal pathology examination of patients with suspected infection requires at least T1-weighted and T2-weighted or STIR sequences, conventional spin-echo (SE) or fast spin-echo (FSE) sequences can be used.
7,8,54 These sequences are needed to provide the necessary contrast between normal and abnormal tissues. T1-weighted sequences (SE or FSE) can be performed quickly and provide high spatial resolution.
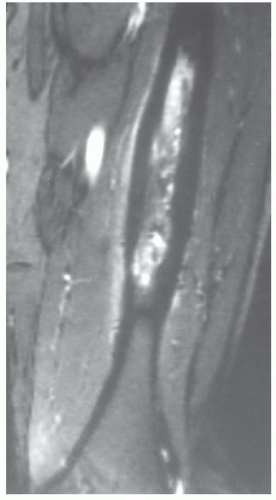
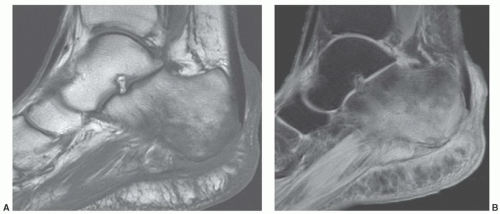
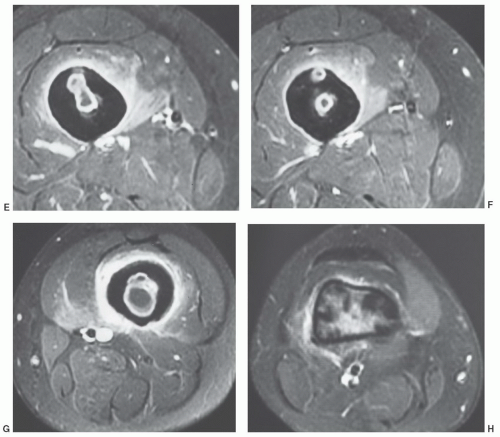
4,5,8,34 Infection is demonstrated as an area of decreased signal intensity compared to the high signal intensity of normal marrow fat (
Fig. 13.4). Changes in cortical bone, periosteum, and muscle are less obvious on T1-weighted sequences (
Fig. 13.4A). T2-weighted (SE or FSE) or STIR sequences demonstrate infection as areas of high signal intensity. We use fat suppression with FSE T-2 weighted sequences. Fat signal is reduced so areas of marrow inflammation are increased in signal intensity compared to normal marrow (
Fig. 13.4B). In certain situations, more than two sequences may be required to improve tissue characterization. Short TI inversion recovery (STIR) sequences (
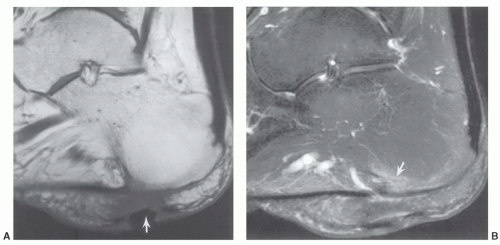
Fig. 13.5) may provide valuable information about fat, water (cellular elements), or subtle inflammatory changes in bone marrow and soft tissues.
4,7,8,34 We routinely add gadolinium-enhanced fat-suppressed T1-weighted images in patients with suspected osteomyelitis (0.1 mmol/kg b.w. intravenously) (
Fig. 13.6).
The anatomic extent of osteomyelitis can be clearly demonstrated by MRI.
4,7,8,31 The extent of disease, including detection of skip areas, is easily established using multiple image planes. This information is particularly valuable when planning surgical debridement.
There have also been several studies comparing isotope studies, CT, and MRI for detection of early osteomyelitis.
56,57,58 Chandnani et al.
56 compared CT and MRI.MRIdemonstrateda94%sensitivity compared to 66%
for CT. Both techniques were equally specific for excluding osteomyelitis. Gallium-67 and indium-111 labeled white blood cells are more specific for infection than technetium scans.
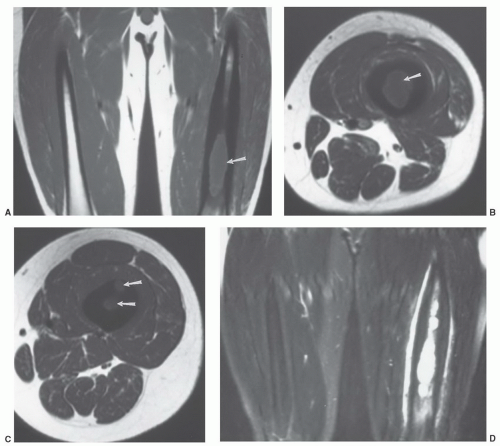
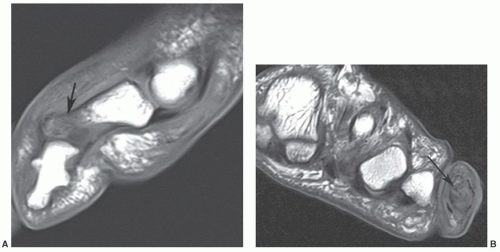
28,56 Beltran et al.
57 compared technetium-99m methylene diphosphonate (MDP), gallium-67, and MRI for evaluating musculoskeletal infection. All techniques were equally effective in detecting osseous infection. However, MRI was more sensitive (100% compared to 69% for isotope scans) in identifying abscesses and distinguishing abscesses fromcellulitis (
Fig. 13.7).
57 Contrast enhancement and diffusion-weighted imaging add to the ease of detection of abscesses.
4,31,55,59The specificity of MRI for diagnosis of osteomyelitis needs to be more clearly defined. Increased signal intensity in marrow, cortical bone, periosteum, and soft tissue is noted on T2-weighted, STIR, and gradient-echo (T2*) sequences (
Figs. 13.4,
13.5,
13.6,
13.7).
4,6,8,16,53Morrison et al.
53 evaluated fat-suppressed gadolinium-enhanced imaging in 51 patients with suspected osteomyelitis. These studies were compared with conventional T1- and T2-weighted MR images and technetium-99m MDP bone scintigrams. Focal enhancement with gadolinium was considered indicative of osteomyelitis (
Fig. 13.6). In 73% of patients, the diagnosis was complicated by postoperative change, chronic osteomyelitis, or neurotrophic arthropathy. Despite this, enhanced fat-suppressed T1-weighted MR images demonstrated a sensitivity of 88% and specificity of 93% compared to a sensitivity of 79% and specificity 53% for non-gadolinium MR images (
Fig. 13.8). Bone scans were 61% sensitive and 33% specific.
53 Most
agree that sensitivity for detection of infection is improved by contrast-enhanced imaging. However, findings are not specific in differentiating infection from inflammation or neoplasms.
47 Lack of bone enhancement effectively excludes infection.
47,53,59More recently, Johnson et al.,
60 studied the utility of signal abnormality on T1-weighted images for confirming osteomyelitis. Nineteen of twenty cases demonstrated confluent decreased marrow signal intensity (
Fig. 13.9) for a 95% sensitivity and 91% specificity. More subtle changes on T1-weighted sequences were less specific.
Chronic Osteomyelitis
With acute infections, the clinical features combined with MR features are used to make the diagnosis. Biopsy may be necessary to confirm the organism. With subacute, chronic, or long-standing infections, image features may be more difficult to interpret. MR features combined with radionuclide scans or PET imaging may be required to define active infection. Chronic infection may be related to inadequate treatment, specific organisms, and other clinical features such as immunodeficiency.
1,21,22,27,32,39,46,61,62,63This section will consider low-grade and subtle infections such as tuberculosis, atypical mycobacterial infections, fungal infections, and specific conditions such as chronic relapsing multifocal osteomyelitis (CRMO) and Synovitis, Acme, Pustulosis, Hyperostosis, Osteitis (SAPHO) (
Table 13.1).
7,27,61,64,65,66,67,68Diagnosis of chronic osteomyelitis is often delayed significantly due to nonspecific symptoms and radiographic features.
25,27,38,61,64,65,66,67,68
Mycobacterium Tuberculosis
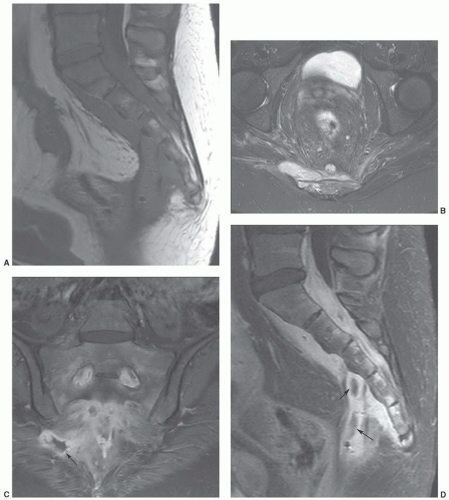
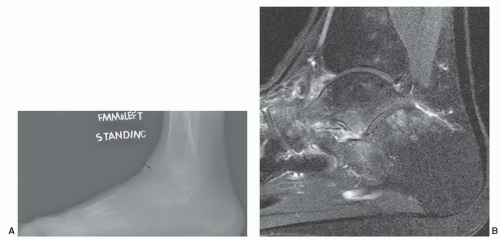
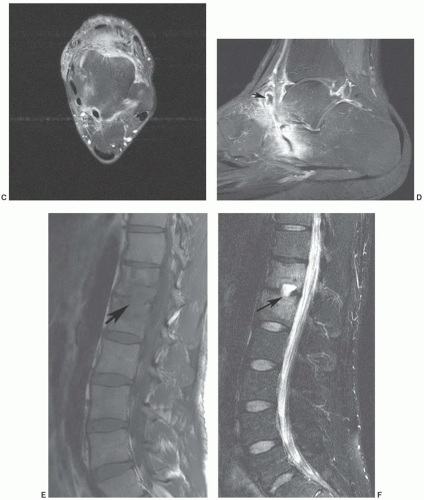
Tuberculosis continues to be a significant health problem in all countries, especially developing countries.
69,70 Musculoskeletal involvement occurs in 1% to 3% of patients.
70 Spinal involvement (accounts for 50%) of musculoskeletal involvement and tuberculous arthritis (accounts for 60%) respectively remain the most common sites of involvement (
Fig. 13.10).
64,70 Extraspinal osteomyelitis accounts for 19% of musculoskeletal tuberculosis. Pulmonary tuberculosis is evident in about 50% of patients with musculoskeletal involvement.
70 Tuberculous osteomyelitis involves the metaphysis or epiphysis similar to pyogenic osteomyelitis. Periosteal reaction, bone sclerosis, and sequestra are less common than pyogenic infection.
61,70 Changes may
resemble a benign bone tumor or, if more aggressive, round cell lesions such as Ewing sarcoma, lymphoma, or leukemia.
7,31 CT, radionuclide scans, and MRI frequently add little to the specificity of the pathology.
61,69 Therefore, biopsy and culture are required.
In children, multiple lytic lesions may mimic fungal infection, pyogenic osteomyelitis, or neoplasms. The latter include eosinophilic granuloma, neuroblastoma, or lymphoma.
38Sharma
61 described MR features of tuberculous osteomyelitis. Two types of lesions were described. Lesions might have predominantly low or intermediate signal intensity on T2-weighted sequences and low signal intensity on T1-weighted sequences. Features are related to central
caseating necrosis in tubercular granulomas. The second image feature described was low intensity with marginally higher intensity peripherally on T1-weighted images. Surrounding edema was common in this setting. Extraosseous soft tissue edema and abscess formulation were evident in about 80% of cases.
61
Atypical Mycobacterial Osteomyelitis