CHAPTER 6 Miscellaneous Problems: Synovitis, Degenerative Joint Disease, and Tumors
GENERAL CONSIDERATIONS
Synovitis
The role of arthroscopic synovectomy in treating synovial diseases was apparent to the earliest arthroscopists. In almost all pathology of the hip, synovitis is present. Our group has had several undiagnosed cases of hip pain with effusions that were shown to be seronegative rheumatoid arthritis with synovial biopsy. In 1988, Ide and colleagues1 performed arthroscopic synovectomy for RA on six hips in three patients using mechanical shavers through a two-portal technique, with good results. With the advent of laser and radiofrequency (RF) ablation, there are now three modalities used to débride the synovium. It remains difficult to reach 100% of the joint but with newer, more effective medical management, debulking of the diseased synovium seems to be adequate.
CPPD has not been reported as frequently in the hip as it has in the ligamentum flavum and in the knee, associated with RA.2,3 Our group has performed synovectomy on two patients for CPPD associated with femoroacetabular impingement. Clearly, it is an entity that should be considered in the differential diagnosis of patients with refractory synovitis.
There are no reports in the arthroscopic literature on the treatment of hyperlipoproteinemia, hemachromatosis, or any of the metabolic arthropathies. Our group has performed partial synovectomy in a few patients thought to have fatty deposition and in one patient with hemachromatosis associated with arthritis. It is presented here only to make the arthroscopic surgeon aware that metabolic arthropathies exist.4 Metabolic arthropathy appears as white or yellowish plaques on the articular cartilage associated with a mild synovitic reaction. The plaque cannot be removed without destroying the articular cartilage and therefore should be treated with synovectomy only.
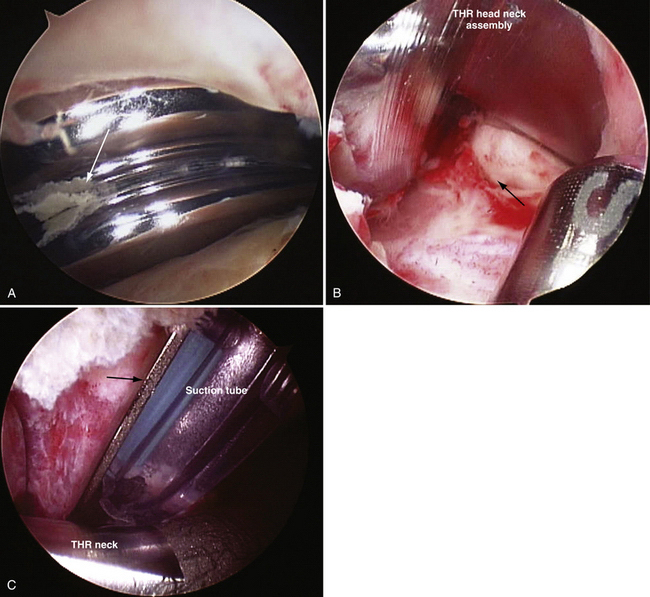
Arthroscopic débridement and lavage has become the treatment of choice for septic arthritis in children, adolescents, and adults. This modality has been associated with minimal morbidity and an excellent cure rate.5–8 McCarthy and associates9 have reported on successful treatment of septic total hips in two patients using arthroscopic débridement, lavage, and intravenous antibiotics Our group has successfully treated four patients with late hematogenous infections of their total hips arthroscopically. No recurrence has been noted, with the longest follow-up being 20 years, when one patient died from natural causes at the age of 93 years (Fig. 6-1).
Degenerative Joint Disease
The arthroscopic treatment of degenerative joint disease (DJD) of the hip remains controversial and most challenging and difficult. Even the most experienced hip arthroscopists avoid the procedure in DJD because there are few benchmarks to predict a successful outcome. Prior to 2001, DJD was treated with arthroscopic débridement, labrectomy, synovectomy, and abrasion chondroplasty. In 28 of 290 patients who had partial labrectomies in the presence of DJD, only 21% had a good result compared with a 71% good result rate in those without DJD.10 Subsequently, with the recognition of femoroacetabular impingement (FAI) and the added correction of the abnormal morphology, the modified Harris hip score improved significantly from 72 to 92 with an average 4-year follow-up.11–13
A residual head-neck deformity from femoral neck fractures has been a cause of FAI and DJD. Reshaping of the deformity has been done using an open surgical dislocation by Eijer and coworkers.14 Our group has treated the DJD and deformity with an arthroscopic head-neck osteoplasty and débridement, synovectomy, and abrasion chondroplasty with microfracture in three patients.
Tumors
Essentially all tumors that are amenable to arthroscopic treatment are benign. Pigmented villonodular synovitis (PVNS) and synovial chondromatosis may be considered synovial diseases instead of tumors, and are both difficult to eradicate unless a complete synovectomy can be performed. Frequent recurrences are seen, from inadequate removal of the tumors or inadequate synovectomy.15–17 Capsulotomy is recommended to expose all areas and recesses of the central and peripheral compartments to remove the loose and attached bodies and ablate the synovium, particularly where the lesions are forming.
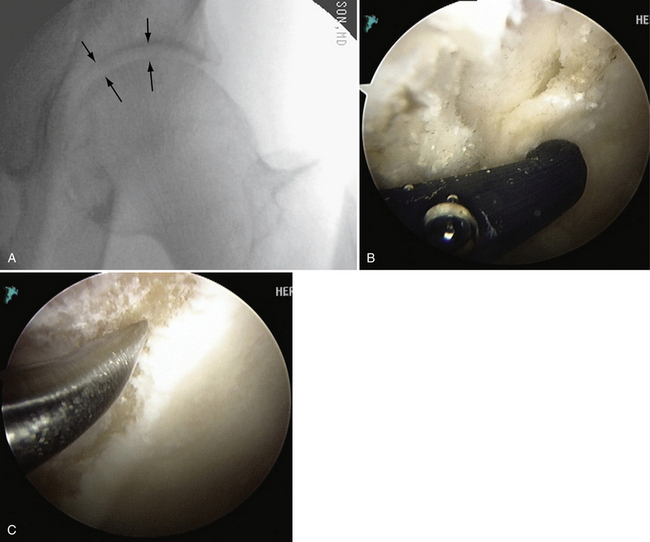
Arthroscopic removal of osteoid osteoma of the hip has been described by Glick and colleagues18 in two cases in the central compartment. Our group has since removed an old, yet active osteoid osteoma from the head-neck junction associated with a cam impingement requiring excision, synovectomy, and head neck osteoplasty (Fig. 6-2).
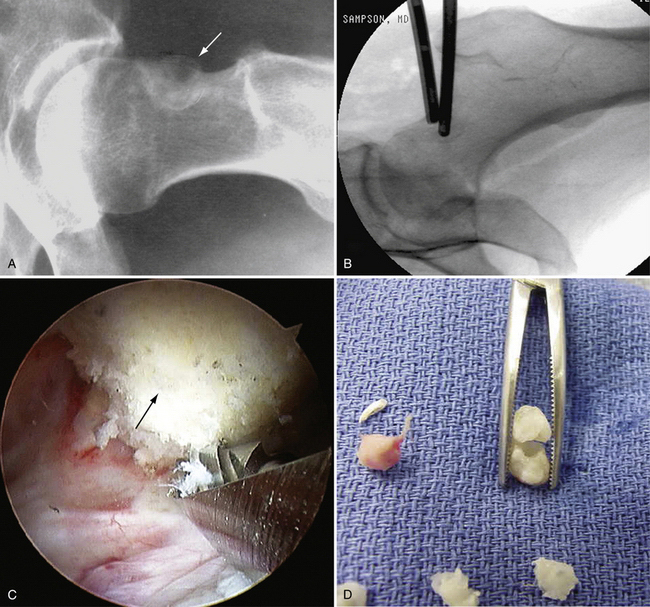
FIGURE 6-2 A, Radiograph of a 43-year-old woman with a 10-year history of a painful osteoid osteoma (arrow). B, Localization with fluoroscopy at surgery. C, The mass effect of the osteoid osteoma seen at arthroscopy (arrow). D, Removed osteoid osteoma, along with multiple loose bodies.
Heterotopic bone should be considered a pseudotumor of the hip and is most often a complication of trauma or hip surgery. There are no reports of its treatment using arthroscopic techniques; however, our group favors arthroscopic excision and follow surgery with a single dose of 700 rad of radiation or a strong dose of nonsteroidal anti-inflammatory drugs (NSAIDs) for 3 to 6 weeks. The recurrence rate is lower with the subsequent radiation.
ANATOMY AND PHYSICAL EXAMINATION
Degenerative joint disease presents with or without a limp, and difficulty walking, sitting, and putting on shoes and socks because of restricted range of motion. With the loss of articular cartilage, a straight leg raise with the knee extended may cause pain in the groin because of the compressive forces of the opposing chondromalacic surfaces of the head and acetabulum. There may be popping and catching with rotation. Loss of internal rotation is almost always present. The Trendelenburg sign and test may be negative in milder cases. Our group has found that if there is at least 50% range of rotational movement when tested passively compared with the normal contralateral side, and if more than 50% of articular cartilage thickness on the anteroposterior (AP) x-ray is present, results show a more than 80% chance of significant improvement that continues for more than 2 years (Fig. 6-3).
Tumors present with pain and, in many cases, popping and catching. There may be a limp if there is an effusion. Range of motion may be restricted if catching or locking is present. Most patients may present with entirely normal movement. Osteoid osteomas usually cause night pain that is relieved by aspirin or other NSAIDs.18,19
PREOPERATIVE IMAGING AND PLANNING
The findings of synovitis on x-ray may be normal in the early stages may include subtle erosions and cyst formation. On MRI, the findings in RA may include subchondral erosions and hypertrophic synovium.20
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree