CHAPTER 1 Clinical Examination and Imaging of the Hip
HISTORY AND PHYSICAL EXAMINATION
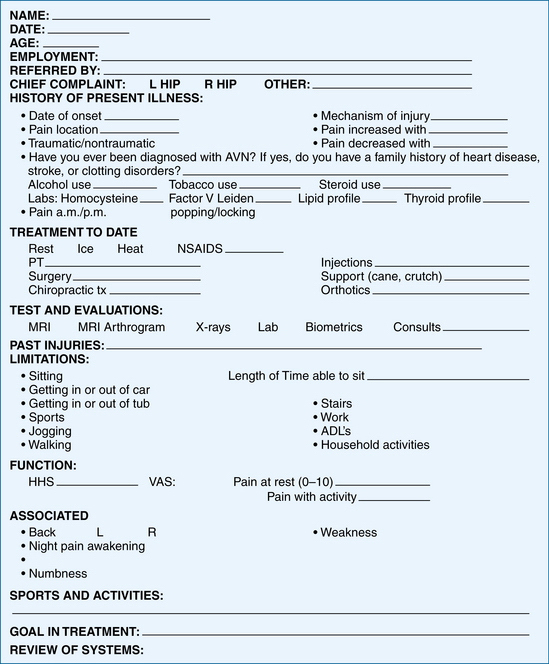
History
The location of the presenting pain and presence or absence of popping will aid in the determination of intra-articular versus extra-articular causes. Participation in sports and other activities are documented, which can help determine the type of injury. Rotation sports, such as golf, tennis, ballet, and martial arts, have been commonly associated with injuries to the intra-articular structures. Finally, treatment goals and expectations are reviewed with the patient. Treatment may vary, based on the patient’s expectations and postoperative goals. See Figure 1-1 for an illustration of a form for a complete review of the history.
A modified Harris hip or Merle d’Aubigné (MDA) score is a general guide to establish the gross levels of function. The modified Harris hip score (HHS) is the most documented and standardized functional score to date, which is a quantitative score based on pain and function. However, the high-performing athletic population may be best evaluated by the athletic hip score.1 Other hip scores have been outlined with quantifications for more specific patient populations, such as the nonarthritic hip score (NAHS), hip disability and osteoarthritis outcome score (HOOS), musculoskeletal function assessment (MFA), short form 36 (SF-36), and the Western Ontario and McMaster University (WOMAC) osteoarthritis index.2 Currently, the MAHORN (Multicenter Arthroscopy of the Hip Outcomes Research Network) Group is in the final stages of testing the hip outcomes score (HOS), which will provide an internationally accepted score and be useful for the athletic population.3
Physical Examination
The hip assumes an essential role in most activities. The hip is not only responsible for distributing weight between the appendicular and axial skeleton, but is also the joint from which motion is initiated and executed. It is known that the forces through the hip joint can reach three to five times the body’s weight during running and jumping.4 Hip pain often stems from some type of sports-related injury.1 Of athletic injuries in children, 10% to 24% are hip-related, whereas 5% to 6% of adult sports injuries originate in the hip and pelvis.5 Athletes participating in rugby and martial arts have also been reported to have an increased incidence of degenerative hip disease.6 Currently, 60% of intra-articular disorders are initially misdiagnosed.7 An organized physical examination will help in the diagnosis of hip problems.
A consistent hip examination is performed quickly and efficiently to screen the hip, back, and abdominal, neurovascular, and neurologic systems and to find the comorbidities that coexist with complex hip pathology. Each examination or physical evaluation has a specific method of being performed, although interobserver consistency and practice is one of the most important aspects of the evaluation.8
The technique of physical examination is dependent on the examiner’s experience and efficiency. The most efficient order of examination begins with standing tests followed by seated, supine, and lateral tests, ending with prone tests.9,10 The physical examination will be fine-tuned and directed through the review of the history of present illness. As with other extremity examinations, access for exposure and patient comfort with loose-fitting clothes about the waist are helpful. An assistant to record the examination on a standardized written form aids in accurate documentation and thoroughness, especially when first starting a comprehensive hip evaluation.
Standing Examination
As the patient stands (Table 1-1), a general point of pain is noted with one finger, and can usually help direct the examination. The groin region directs a suspicion of intra-articular problem and lateral-based pain is primarily associated with intra- or extra-articular aspects. A characteristic sign of patients with intra-articular hip pain is the C sign.8 The patient will hold his or her hand in the shape of a C and place it above the greater trochanter, with the thumb positioned posterior to the trochanter and fingers extending into the groin. This finding can be misinterpreted as lateral soft tissue pathology, such as trochanteric bursitis or the iliotibial band; however, the patient is often describing deep interior hip pain.8 Posterior-superior pain requires a thorough evaluation in differentiating hip and back pain. The shoulder height and iliac crest heights are noted to evaluate leg length discrepancies (Fig. 1-2). Incremental wooden blocks placed under the short side heel help in orthotic considerations. General body habitus is assessed and issues of ligamentous laxity are determined by the middle finger test or hyperextension of the elbows or knees. Structural versus nonstructural scoliosis is differentiated by forward bending and the degree of lumbar flexion is recorded. Side-bending ROM is also useful.
TABLE 1-1 Standing Examination Assessment
| Examination | Assessment and Association |
|---|---|
| Abductor deficient gait | Abductor strength, proprioception mechanism |
| Antalgic | Trauma, fracture, synovial inflammation |
| Pelvic rotational wink | Intra-articular pathology, hip flexion contracture, increased femoral anteversion, anterior capsual laxity |
| Foot progression angle with excessive external rotation | Femoral retroversion, increased acetabular anteversion, torsional abnormalities, effusion, ligamentous injury |
| Foot progression angle with excessive internal rotation | Increased femoral anteversion or acetabular retroversion, torsional abnormalities |
| Short leg limp | Iliotibial band pathology, true-false leg length discrepancy |
| Single-leg stance phase test | Abductor strength, proprioception mechanism |
| Spinal alignment | Shoulder–iliac crest heights, lordosis, scoliosis, leg length |
| Laxity | Ligamentous laxity in other joints: thumb, elbows, shoulders, or knee |
See video for performing seated examination tests.
Gait abnormalities often help detect hip pathology.11,12 Joint stability, preservation of the labrum and articular cartilage, and proper functioning of the hip joint involve three biomechanical planes of the femur and acetabulum. These relationships are important for the transfer of dynamic and static load to the ligamentous and osseous structures.
Noting iliac crest rotation and terminal hip extension assesses pelvic rotation. On average, a normal gait requires 6 to 8 degrees of hip rotation and 7 degrees of pelvic rotation, for a total rotation of 15 degrees.12 The pelvic wink is demonstrated by an excessive rotation in the axial plane toward the affected hip, thus producing extension and rotation through the lumbar spine, to obtain terminal hip extension. This winking gait can be associated with intra-articular hip pathology, laxity, or hip flexion contractures, especially when combined with increased lumbar lordosis or a forward-stooping posture. Gait changes can affect spinal mechanics and function. Excessive femoral anteversion, or retroversion, can affect a wink on terminal hip extension because the patient will try to create greater anterior coverage with a rotated pelvis. Injury to the anterior capsule can also contribute to a winking gait.
During the stance phase, body weight must be supported by a single leg, with the gluteus maximus, medius, and minimus providing most of the force.12 Maximum ground reactive force occurs on heel strike at 30 degrees of hip flexion. A shortened stance phase can be indicative of neuromuscular abnormalities, trauma, or leg length discrepancies. The abductor deficient gait (Trendelenburg gait or abductor lurch) is an unbalanced stance phase attributed to abductor weakness or proprioception disruption. This pattern may present in two ways—with a shift of the pelvis away from the body (a dropping out of the hip on the affected side), or with a shift of the weight over the adducted leg (a shift of the upper body over the top of the affected hip). The antalgic gait is characterized by a shortened stance phase on the painful side, limiting the duration of weight-bearing (a self-protecting limp caused by pain). A short leg gait is noted by drop of the shoulder in the direction of the short leg.
In addition to body habitus and gait evaluation, the single-leg stance phase test (Trendelenburg test) is performed during the standing evaluation of the hip. The single-leg stance phase test is performed on both legs, with the nonaffected leg examined first, to establish a baseline (Fig. 1-3). During this test, the examiner stands behind the exposed patient (to the degree that the bony landmarks are easily observed). The patient stands with the feet shoulder width apart and then brings one leg forward by flexing the leg to 45 degrees at the hip and 45 degrees at the knee, thereby simulating the single-leg stance phase with the load on the examined hip. This position is held for 6 seconds. As the patient lifts and holds one foot off the ground, the contralateral hip abductor musculature and neural loop of proprioception are being tested. The pelvis will tilt toward or away from the unsupported side if the musculature is weak or if the neural loop of proprioception is disrupted. Normal dynamic midstance translocation is 2 cm during a normal gait pattern12; a shift in either direction of more than 2 cm constitutes a positive shift. This test is also performed in a dynamic fashion by some examiners.
Seated Examination
The seated hip examination (Table 1-2) consists of a thorough neurologic and vascular examination. The need to check the basics is obvious, even in apparently healthy individuals. The posterior tibial pulse is checked first, any swelling of the extremity is noted, and inspection of the skin is performed at this time. A straight leg raise test is then performed by passively extending the knee into full extension. The straight leg raise test is helpful for detecting radicular neurologic symptoms.
TABLE 1-2 Seated Examination Assessment
| Examination | Assessment and Association |
|---|---|
| Neurologic | Sensory nerves originating from the L2-S1 levels, deep tendon reflex of patella (L2-L4 spinal nerves and femoral nerve) and Achilles (L5-S1 sacral nerves) |
| Straight leg raise | Radicular neurologic symptoms |
| Vascular | Pulses of the dorsalis pedis and posterior tibial artery |
| Lymphatics | Skin inspection for swelling, scarring, or side to side asymmetry |
| Internal rotation | Normal between 20 and 35 degrees |
| External rotation | Normal between 30 and 45 degrees |
See video for performing seated examination tests.
The loss of internal rotation is one of the first signs of an intra-articular disorder; therefore, one of the most important assessments is internal and external rotation in the seated position. The seated position ensures that the ischium is square to the table, thus providing sufficient stability at 90 degrees of hip flexion and a reproducible platform for accurate rotational measurement. Passive internal and external rotation testing are performed gently and compared from side to side. Seated rotation range of motion is also compared and contrasted with the extended position of the hip (Fig. 1-4).
Musculotendinous, ligamentous, and osseous control of internal and external rotation are complex, so any differences in seated versus extended positions may raise the question of ligamentous versus osseous abnormality. Sufficient internal rotation is important for proper hip function—there should be at least 10 degrees of internal rotation at the midstance phase of normal gait,12 but less than 20 degrees is abnormal (see Table 1-3 for normal ROM). Pathology related to femoroacetabular impingement or to rotational constraint from increased or decreased femoral or acetabular anteversion can result in significant side-to-side differences. An increased internal rotation combined with a decreased external rotation may indicate excessive femoral anteversion and distinguished from hip capsular pathology by radiographic and biometric assessment.
Supine Examination
A battery of tests with the patient in the supine position (Table 1-4) helps distinguish internal from extra-articular sources of hip symptoms further. The supine examination begins with the assessment of leg lengths. Next, passive hip flexion range of motion is assessed (Table 1-3). Both knees are brought up to the chest and the degree of flexion is recorded (Fig. 1-5). It is important to note the pelvic position because the hip may stop early in flexion, with the end range of motion being predominantly pelvic rotation. From this position, the hip flexion contracture test (Thomas test) is performed by having the patient extend and relax one leg down toward the table (Fig. 1-6). Any lack of terminal extension, noted by the inability of the thigh to reach the table, demonstrates a hip flexion contracture. Both sides are examined for comparison. An important aspect of this test is to obtain the zero set point for the lumbar spine. Patients with hyperlaxity or connective tissue disorders could have a false-negative result. In these patients, the zero set point can be established with an abdominal contraction. The hip flexion contracture test could also be falsely negative if there is lumbar spine hyperlordosis.
TABLE 1-4 Summary of Supine Examinations and Assessment
| Examination | Assessment and Association |
|---|---|
| Range of motion | Flexion, abduction, adduction |
| FADDIR | Anterior femoroacetabular impingement, torn labrum |
| Hip flexion contracture test (Thomas test) | Hip flexor contracture (psoas), femoral neuropathy, intra-articular pathology, abdominal cause |
| FABER (Flexion, Abduction, External Rotation) | Distinguish between back and hip pathology, specifically sacroiliac joint pathology |
| Dynamic internal rotatory impingement test (similar to McCarthy test) | Anterior femoroacetabular impingement, torn labrum |
| Dynamic external rotatory impingement test (similar to McCarthy test) | Superior femoroacetabular impingement, torn labrum |
| Posterior rim impingement test | Posterior femoroacetabular impingement, torn labrum |
| Passive supine rotation test (log roll) | Trauma, effusion, synovitis |
| Heel strike | Trauma, femoral fracture |
| Straight leg raise against resistance (Stinchfield) | Intraarticular pathology along with psoas tendonitis or bursitis. Hip flexor strength |
| Palpation | |
See video for performing supine examination tests.
TABLE 1-3 Normal Internal and External Rotation Range of Motion
| Range of Motion Assessment | Normal (degrees) | Abnormal (degrees) |
|---|---|---|
| Seated internal rotation | 20-35 | <20 |
| Seated external rotation | 30-45 | <30 |
| Extended internal rotation | 20-35 | <20 |
| Extended external rotation | 30-45 | <30 |
| Supine hip flexion | 100-110 | <100 |
| Adduction | 20-30 | <20 |
| Abduction | 45 | <45 |
The FABER test, conventionally known as the Patrick test, is helpful in determining hip versus lumbar complaints (Fig. 1-7). Re-creation of hip pain can be associated with musculotendinous or osseous posterior lateral acetabular incongruence or ligamentous injury. In cases of a coup-contrecoup injury, in which the mechanism of injury is initiated posteriorly, pain will be secondarily referred to anteriorly.
For the DIRI test, the patient is in the supine position and instructed to hold the nonaffected leg in flexion beyond 90 degrees, thus establishing a zero pelvic set point and eliminating lumbar lordosis. The examined hip is then brought into 90 degrees of flexion or beyond and is passively taken through a wide arc of adduction and internal rotation (Fig. 1-8). A positive result is noted with re-creation of the complaint pain. DIRI can also be performed in the operating room for direct visualization of femoral neck and acetabular congruence (video).

FIGURE 1-8 Dynamic internal rotatory impingement (DIRI) test. A, DIRI begins with the hip at 90 degrees flexion or beyond. B, It is then passively taken through a wide arc of adduction and internal rotation (arrows) while decreasing flexion to about 80 degrees.
For the DEXRIT test, the patient is in the supine position and instructed to hold the nonaffected leg in flexion beyond 90 degrees, thus eliminating lumbar lordosis. The hip is then brought into 90 degrees flexion or beyond and dynamically taken through a wide arc of abduction and external rotation (Fig. 1-9). A positive result is noted with re-creation of pain. DEXRIT can be performed intraoperatively for direct visualization of femoral neck and acetabular congruence (video).
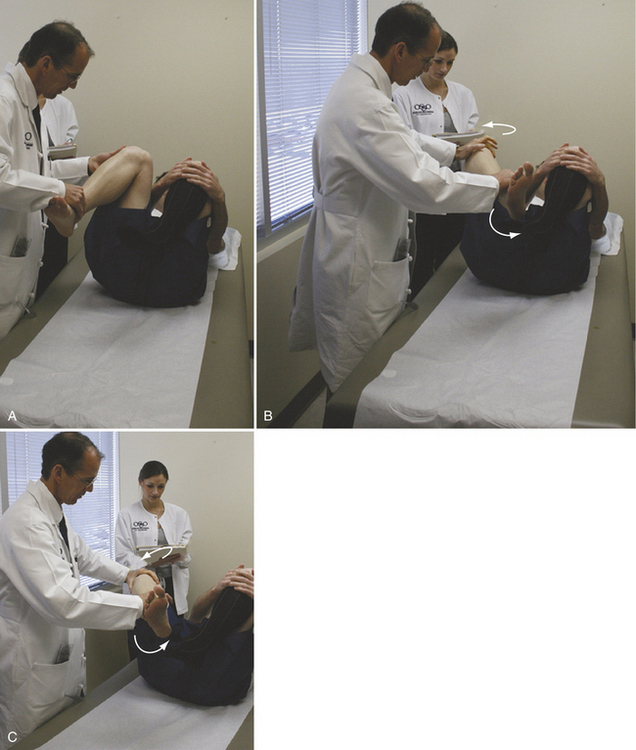
FIGURE 1-9 The dynamic external rotatory impingement test (DEXRIT). A, DEXRIT begins with the hip at 90 degrees flexion or beyond. B, C, It is then dynamically taken through a wide arc of abduction and external rotation (arrows).
Passive abduction and adduction range of motion are assessed in the supine position (see Table 1-3). Palpation of the abdomen is performed and any tenderness is documented (Fig. 1-10). Abdominal tenderness is differentiated from fascial hernia and/or adductor tendinitis. Resisted torso flexion with palpation of the abdomen will differentiate the fascial hernia from other complaints. Palpation of the adductor tubercle with active testing will detect adductor tendonitis. Common physical examination findings associated with athletic pubalgia include inguinal canal tenderness, pubic crest-tubercle tenderness, adductor origin tenderness, pain with resisted sit-ups or hip flexion, and a tender, dilated superficial ring.
Other useful tests may include Tinel’s test of the femoral nerve. This test is found to be positive with hip flexion contractures of more than 25 degrees as a result of the proximity of the psoas tendon and femoral nerve. A heel strike is performed by striking the heel abruptly. A positive response is indicative of trauma or a stress fracture (Fig. 1-11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree