CHAPTER 10 Abductor Tears
Tendinopathy and tears of the gluteus medius and minimus tendons are a common cause of recalcitrant pain along the lateral side of the hip. Tears of the gluteus medius and minimus tendon were first described by Bunker and Kagan and colleagues in the late 1990s.1,2 Bunker and associates1 reported a 22% incidence of concomitant medius tears in 50 patients treated for femoral neck fractures. The tears were most commonly seen distally at the junction of the gluteus medius and minimus. Howell and coworkers3 reported that 22% of women and 16% of men who underwent total hip arthroplasty for osteoarthritis (N = 176) had abductor tears. The incidence was greater with increased age in both groups.
Abductor tears should certainly be suspected in patients with intractable GTPS in whom conservative management has failed. The pain can be variable, but is characteristically exacerbated by weight-bearing and resisted hip abduction. Bird and colleagues4 used MRI to evaluate the integrity of the gluteus medius in 24 women with recalcitrant GTPS. A tear of the medius tendon insertion was found in 46% of patients, and an additional 38% had gluteus medius tendonitis without an appreciable tear. Kagan and associates2 performed an open medius tendon repair in 7 patients with recalcitrant GTPS and magnetic resonance imaging (MRI) evidence of a tear. In all cases, the tear was located anteriorly in the lateral facet portion of the insertion. Repairs were performed using bone tunnels and anchors. At a median follow-up of 45 months, all patients were pain-free and all but one returned to previous levels of activity.
Although the causes of these tears are likely multifactorial, gluteus medius and minimus tears likely reflect a progressive degenerative process. A precipitating traumatic event is possible but uncommon. Most patients describe an insidious but often debilitating lateral-sided hip pain. The abductors have been likened to the rotator cuff of the hip, with the medius and minimus tendon analogous to the supraspinatus and subscapularis muscles. The medius tendon inserts on the lateral and posterosuperior facets, resulting in a moment arm similar in direction and force to the supraspinatus. The minimus inserts on the anterior facet and, depending on the position of the femur, can exert several different moments, including flexion, abduction, and internal and external rotation. Based on these observations, it follows that one of the primary functions of the minimus is to act as a head stabilizer. However, in many functional flexion angles, it provides a primary internal rotation force similar to that of the subscapularis.5 Similar to the rotator cuff, tears of the medius are significantly more common than those of the minimus. It has been estimated that almost 25% of middle-aged women and 10% of middle-aged men will develop a tear of the gluteus medius tendon.3,6 Tears are four times more common in women than in men.
Tear progression appears to occur by degeneration of the undersurface propagating posteriorly into a full-thickness tear.3,6 Most tears occur in the anterior portion of the tendon as it attaches into the lateral facet of the greater trochanter. These frequently start as partial-thickness undersurface tears that propagate into full-thickness lesions that can extend posteriorly.
Both open and arthroscopic techniques of repair can provide excellent symptomatic relief and restore abductor function. Arthroscopic techniques provide a less invasive alternative and can be readily performed. Regardless of the technique, however, determining the anatomic gluteus medius footprint is critical and can often be difficult. Unlike the supraspinatus tendon, no articular margin is present to be used as a reference landmark.6
ANATOMY
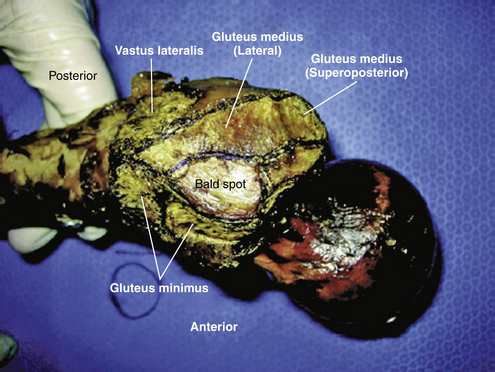
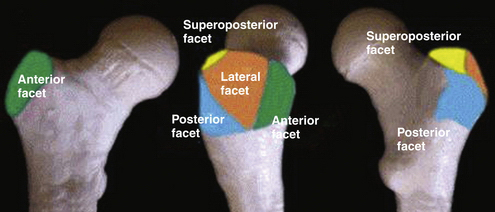
The gluteus medius tendon has two separate entheses on the greater trochanter. The posterior fibers attach to the posterosuperior facet (PSF), whereas the central and anterior fibers insert on the lateral facet (LF) of the trochanter. The facets are oriented at different planes relative to one another (Figs. 10-1 and 10-2).7 The tendinous portion inserting into the PSF is robust, with a circular insertion site of approximate radius of 8.5 mm. The surface area of this insertion is approximately 200 mm2. The lateral facet insertion is more rectangular in shape, with a surface area approximating 440 mm2.
The trochanteric insertion of the gluteus minimus is separated from the proximal portion of the LF footprint by the trochanteric bald spot. Near the midsubstance of the LF footprint, the bald spot ends and the long head of the minimus begins. At this location, the medius footprint abuts and covers a portion of the gluteus minimus.7 The trochanteric bald spot is circular in shape, with a radius of approximately 11 mm. Although it combines with the gluteus medius to comprise the entire lateral facet of the greater trochanter (see Fig. 10-1 and 2), it is critical not to overestimate the size of tendon detachment with an abductor tear by mistakenly incorporating the normal bald spot into the anatomic footprint of the medius tendon.6
The anatomically distinct insertions of the medius are thought to correlate with anatomically distinct portions that function in a phasic manner during the gait cycle. The posterior portion that inserts into the PSF is thought to stabilize the femoral head in the acetabulum during heel strike. The central portion, inserting into the PSF and LF junction, runs more vertically and is thought to be critical in initiating hip abduction. The anterior portion aids in abduction but also functions as an external rotator of the pelvis during swing-through on the contralateral limb.7
CLASSIFICATION
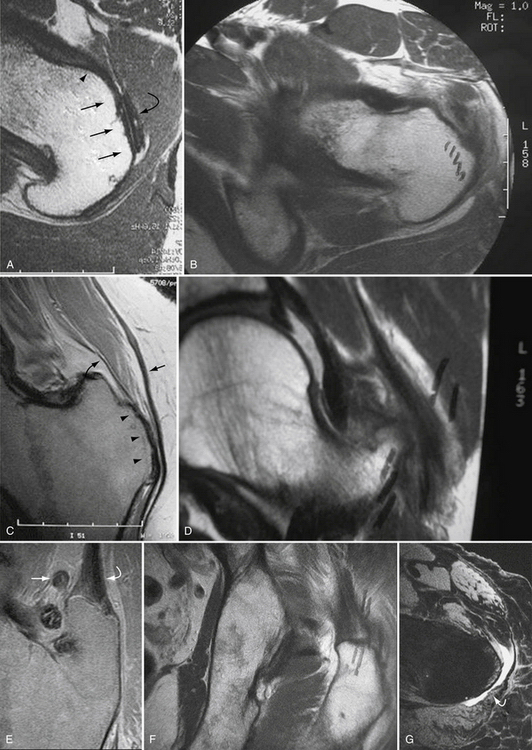
Dwek and associates8 and others9–14 have described a standardized MRI approach to abductor tear classification. They have divided the greater trochanter into four facets—posterosuperior, lateral, anterior, and posterior (Fig. 10-3; see Fig. 10-2). The minimus attaches to the anterior facet (see Fig. 10-3A and B). Figure 10-3A shows the normal attachment of the minimus and Figure 10-3B shows the corresponding image demonstrating a gluteus minimus tear. The medius inserts on the lateral and posterosuperior facets (see Figs. 10-3C-F). Figures 10-3C and E show the normal insertional anatomy of the medius on the LF and PSF whereas Figures 10-3D and F show corresponding images demonstrating medius tendon tears at the respective facets. The posterior facet is covered by the trochanteric bursa (see Fig. 10-3G).