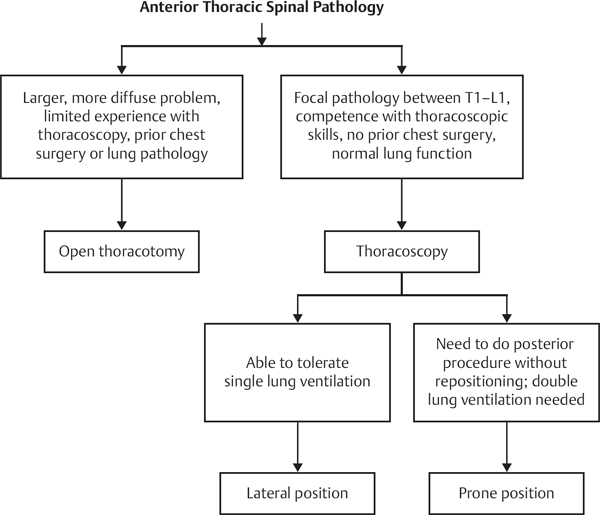
56 Modern minimally invasive surgery (MIS) techniques in the spine have focused primarily on the thoracolumbar spine. Current advances include the use of endoscopic visualization, fiberoptic lighting, and dilator-tubular retractor systems to facilitate direct visualization of the spine through small incisions (Fig. 56.1). The advantage of MIS is that the same surgery can be performed with less injury to the soft tissues, and therefore less pain and quicker recovery. Although much of the early MIS work has focused on the ability to decompress the neural structure, techniques for fusion and instrumentation of the spine are now being developed. A small number of clinical studies have compared MIS and open decompression techniques and found equivalent results. Direct clinical studies comparing these modern MIS approaches with traditional open techniques for cervical spine fusion have not yet been published, but proponents claim their clinical results are equal or superior to the more invasive open procedures. Although the anatomic constraints of the cervical spine are different from those of the thoracolumbar spine, an MIS approach in this region appears feasible. Fig. 56.1 A view of the lateral mass screws under direct visualization through a tubular posterior cervical minimally invasive surgery retractor. (From Endius Inc., Plainville, MA. Reprinted by permission.) The indications for a posterior cervical MIS approach should be essentially identical to those for open cervical surgery. Although posterior decompressive surgery is highly effective for many neurocompressive lesions, traditional approaches may be associated with significant neck discomfort due to the large amount of soft-tissue trauma associated with the surgical exposure. MIS approaches may decrease the amount of soft-tissue trauma associated with a surgical approach while allowing the goals of the surgery to be met. Similarly, posterior cervical MIS approaches with the insertion of lateral mass screws can be used to supplement an anterior cervical construct with a rigid posterior tension band or possibly to treat pseudarthroses following an anterior procedure (Fig. 56.2). Although no classification system for MIS approaches to the cervical spine has been described, one logical way to think of MIS in the cervical region is to divide the procedure into anterior and posterior approaches and to subdivide procedures into those requiring decompression alone or requiring fusion with or without instrumentation. Fig. 56.2 Insertion of posterior cervical lateral mass screws through a posterior cervical minimally invasive surgery tubular retractor developed by Endius. (From Endius Inc. Plainville, MA. Reprinted by permission.) The workup for a cervical MIS approach is no different from that required for a traditional cervical approach. Patients considered for decompressive surgery should have failed conservative treatment. High-quality imaging studies are mandatory to understand the nature of the pathologic condition. Certain anatomic considerations should be noted, such as bifid spinous processes, which might make it difficult to position the MIS tubes appropriately. The most frequent degenerative conditions treated involve radiculopathy. Although most of the current experience in MIS spinal surgery currently involves degenerative conditions, other conditions, such as cervical trauma or tumors, may be amenable to an MIS approach in the future. Preoperative planning is critical to the success of an MIS operation. The exact location of the pathology must be understood. The size and body habitus of the patient should be considered. All necessary equipment, including a C-arm fluoroscopy unit, should be available in the operating room. Experience in interpreting the fluoroscopic images is paramount to visualizing the true lateral positioning. Special caution should be exercised with a MIS approach because of the limited visualization of the surrounding anatomy. Revision surgery, in particular, may be more demanding as a result of dural adhesions and the risk of dural laceration. All known MIS techniques have significant learning curves; therefore, these highly technical procedures are best learned in a controlled environment. The surgeon should gain experience on simple pathology prior to attempting complex cases. The use of a traditional posterior cervical foraminotomy/discectomy for radiculopathy has been shown to have 95% excellent or good results. Posterior micro-endoscopic diskectomies have demonstrate similar medium-term outcomes to open procedures, with shorter hospital stays, less tissue destruction, less detachment of muscular insertions, and less postoperative pain. The theoretical benefits of a posterior arthrodesis and instrumentation also appear promising, although published series are not yet available to prove the efficacy of these procedures at the time of this writing. Theoretically, an MIS posterior cervical instrumentation strategy should prevent the large degree of muscle stripping and the potential denervation and atrophy inherent to a traditional approach. Complications inherent to the posterior approach include infections, bleeding, nerve root injuries, dural laceration, and retained pathology. If excess removal of the facet is performed, there is also the potential for spinal instability. MIS approaches are expected to have the same basic complications as open surgery, although, because of the technical nature of MIS operations and the steep learning curve involved, it is likely that the incidence of certain complications may be higher early in the learning curve of a surgeon’s MIS experience. Dreyer SJ, Boden SD. Nonoperative treatment of neck and arm pain. Spine 1998;23(24): 2746–2754 PubMed The authors discuss conservative management techniques for neck and back pain. Gala VC, O’Toole JE, Voyadzis JM, Fessler RG. Posterior minimally invasive approaches for the cervical spine. Orthop Clin North Am 2007;38(3):339–349, abstract v PubMed This review article details posterior minimally invasive cervical techniques. Complications and techniques for avoiding them are also discussed. Khoo LT, Beisse R, Potulski M. Thoracoscopic-assisted treatment of thoracic and lumbar fractures: a series of 371 consecutive cases. Neurosurgery 2002;51(5, Suppl):S104–S117 PubMed The authors review the outcomes of 371 cases of thoracoscopically assisted thoracolumbar fracture fixations. Kim DH, Jaikumar S, Kam AC. Minimally invasive spine instrumentation. Neurosurgery 2002; 51(5, Suppl):S15–S25 PubMed Overview of instrumentation and techniques for minimally invasive spinal procedures. Lee SH, Lee JH, Choi WC, Jung B, Mehta R. Anterior minimally invasive approaches for the cervical spine. Orthop Clin North Am 2007;38(3):327–337, abstract v PubMed A review article that details anterior minimally invasive cervical techniques. Complications and techniques for avoiding them are also discussed. Minamide A, Yoshida M, Yamada H, et al. Clinical outcomes of microendoscopic decompression surgery for cervical myelopathy. Eur Spine J 2010;19(3):487–493 PubMed The authors report on their experience performing microendoscopic decompression on 51 patients with cervical myelopathy. They reported the average Japanese Orthopaedic Association (JOA) score improved from 10.1 to 13.6 following surgery and that the average recovery rate was 52.5%. Complications included one dural tear, two C5 nerve root palsies, and one epidural hematoma requiring reoperation. Ramani PS, Singhania BK, Murthy G. Combined anterior and posterior decompression and short segment fixation for unstable burst fractures in the dorso lumbar region. Neurol India 2002;50(3):272–278 PubMed The authors discuss unstable burst fractures and techniques for fixation, including anterior-posterior and short-segment fixation techniques. Vaccaro AR. Combined anterior and posterior surgery for fractures of the thoracolumbar spine. Instr Course Lect 1999;48:443–449 PubMed This article discusses the techniques, instrumentation, and indication for doing combined anterior and posterior surgical procedures of the thoracolumbar spine. Winder MJ, Thomas KC. Minimally invasive versus open approach for cervical laminoforaminotomy. Can J Neurol Sci 2011;38(2):262–267 PubMed The authors retrospectively compared 65 patients who underwent open posterior cervical foraminotomies to 42 patients whose surgeries were performed using a tubular retractor system. There was no difference in operative time or complications. There was less blood loss, less postoperative narcotic use, and shorter length of stay among the patients for whom a tubular system was used.
Minimally Invasive Posterior Cervical Approaches
![]() Classifications
Classifications
![]() Workup
Workup
History
Spinal Imaging
![]() Treatment
Treatment
![]() Outcome
Outcome
![]() Complications
Complications
Suggested Reading
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






