22 Meniscal Injuries/Repair: Arrow
The surgical effort to repair a meniscus rather than remove it recognizes the importance of this structure in knee stability, load transmission, joint lubrication, and articular cartilage nutrition. Loss of the meniscus leads to degenerative changes over time. Repair approaches include the inside-out, outside-in, and all-inside techniques. Special meniscal repair devices have been developed to facilitate the all-inside repair. One of the first of these was the meniscal Arrow (Linuatec, Largo, FL). This technique greatly simplifies the repair especially in the challenging posterior medial and posterior lateral areas. Several clinical studies report favorable results.1–4
Indications
- Longitudinal, peripheral meniscal tears with a good blood supply. Typically this is a tear either at the synovial meniscal junction or in the red/white region.
- Tear length: longer tears do not heal as well. Tears between 1.5 cm and 2 cm have better success.
- Tears in the posterior medial or posterior lateral corner where other techniques might injure neurovascular structures
- Patients who do not wish to have any secondary incisions associated with the conventional meniscal repair
Contraindications
- Good meniscal blood supply is crucial; therefore, avoid repairs in older patients and horizontal cleavage tears.
- Degenerative articular cartilage change
- Allergy to lactic acid
Physical Examination
- Joint line tenderness
- McMurray’s test (or other meniscal tests) positive
- Effusion
Diagnostic Tests
- Physical examination
- Knee radiographs
- Magnetic resonance imaging (MRI) (sometimes indicated)
Special Considerations
The outside-in, single vertical suture is the “gold standard” for meniscal repair. Other techniques may approach the good results of this technique. Most repairable meniscal tears are found associated with an anterior cruciate ligament (ACL) injury, and the surgeon performing an ACL reconstruction should also be prepared to repair the meniscus. Healing rates for “isolated” meniscal repairs in stable knees are ~80%, whereas in knees undergoing ACL reconstruction they are 90 to 95%. The Arrow is made of self-reinforced poly L-lactic acid (PLLA). It biodegrades over time (which may be several years), and an inflammation may be observed. A new contoured head provides a lower profile with less chance of articular cartilage damage.
Preoperative Planning and Timing of Surgery
- Early intervention has not been demonstrated to improve the results. With the ACL-injured knee, it is desirable to wait until the effusion is resolved and good motion is established. This is even more critical when a meniscus repair is performed because of the tendency for postoperative stiffness and swelling.
- The Arrow requires a familiarity with the instrumentation and an understanding of which curved cannula is best for which portion of the tear. Also, only the 10-mm Arrows should be used in the middle third of the meniscus and the 13-mm Arrow in the posterior horn.
Special Instruments
- Arrow insertion cannulas, trocar needle, and pushing obturator.
- The crossbow gun is another insertion alternative.
Anesthesia
Options are general anesthesia, regional anesthesia, or local anesthesia.
Patient and Equipment Positions
- Patient is supine with knee in leg holder
- Standard knee arthroscopy setup
- Standard anterolateral, anteromedial, or central arthroscopy portals
- View through the ipsilateral (or central) portal; instrument through the contralateral portal
- To access the posterior medial meniscus, hold the knee slightly flexed with valgus stress. Access the posterior lateral meniscus by holding the knee in a figure-four position (~90 degrees) with varus stress.
- The Arrow cannula is required for device insertion.
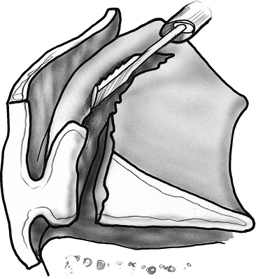
- Procedures to promote meniscal healing (vascular access channel punch, meniscal rasp, synovial abrasion) should be used (Fig. 22–1).
Surgical Procedure
- Establish standard viewing portals. View through the ipsilateral (or central) portal and instrument through the contralateral portal.
- Encourage a healing response by rasping (Fig. 22–1), creating vascular access channels, and synovial abrasion.
- Place the blunt obturator in the Arrow cannula and position it next to the torn meniscus (Fig. 22–2). Turn off the irrigation. Reduce the meniscus with the cannula and remove the obturator.
- Insert the most posterior Arrow first.
- Carefully maintain the cannula position adjacent to the meniscus. Insert the needle trocar through the cannula, then the meniscus (Fig. 22–3), and finally into the joint capsule to create a channel for the Arrow to follow.
- Select the correct-length Arrow (13 mm for posterior tears, 10 mm for middle third tears). Feed the Arrow into the insertion cannula, and then push it into the meniscus with the obturator (Fig. 22–4). Firmly press the obturator or tap it with a mallet until the “T” portion of the Arrow is below the surface of the meniscus (Fig. 22–5).
- Ensure that the “T” portion of the Arrow is horizontal with the tibial surface.
- Place Arrows about 5 to 10 mm apart on the superior surface of the meniscus until the repair is complete.
Dressings, Braces, Splints, and Casts
- A simple absorptive sterile dressing is applied to the skin.
- Compression with Ace bandage
- Progressive weight bearing with crutches as needed
Tips
- The Arrow is designed only for arthroscopic fixation of longitudinal vertical meniscal tears.
- Place the posterior Arrow first and then move forward.
- Be certain that the crossbar is horizontal to the tibial.
- Countersink the crossbar below the surface of the meniscus.
- Keep pressure on the cannula when loading the Arrow to avoid losing tear reduction.
- Turn off the water flow so there is no water flowing back out the cannula while trying to load the Arrow.
Pitfalls and Technique Errors
- This technique is quick and apparently easy. However, problems can occur!
- The PLLA Arrow takes 3 years or longer to degrade. There are reports of inflammatory problems in the knee with Arrow use.5
- The Arrow has been reported to migrate through the knee, become broken, and require later removal.6–8
- If the crossbar is inadvertently oriented vertically, damage to the articular surface can occur.
- Posterior knee pain is reported to occur with this repair technique.9
Postoperative Care and Rehabilitation
- For meniscal repairs performed in association with ACL reconstruction, the usual ACL reconstruction protocol should be followed.10
- Loaded knee flexion should not exceed 90 degrees for the first 8 weeks.
- Early motion is permitted as swelling decreases.
- Weight bearing as tolerated is permitted.
- When there is no effusion, full extension, and flexion to 135 degrees, straight-ahead jogging is permitted.
- Full pivoting sports may begin when there is no pain, swelling, or reduced motion despite running and agility training.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








