Managing Difficult Cases and Patient Instructions
Kirk Eriksen
Learning Objectives
After studying this chapter, the reader should be able to better understand and manage the following cases in their practice:
Modify the Adjustment for patients with difficult Atlas transverse process contacts.
Manage patients with cervical herniated discs, torticollis, Atlantoaxial rotatory fixations, cervical laminectomies, Cervical spondylotic Myelopathy, and cervical fractures.
Provide information for managing patients with such congenital findings as Upper cervical articular asymmetry, basilar invagination, Platybasia, atlas occipitalization, Klippel Feil syndrome, anomalies that can cause instability, atlas posterior ponticle, and Arnold Chiari malformation.
Manage patients who are in wheelchairs, paraplegic, have anatomical leg length inequality, or are lower-extremity amputees and/or in leg casts.
Review both activities to avoid and to do during home care to help stabilize the spine and help Adjustments hold longer.
Cover the importance of patients getting a proper amount of exercise, rest, nutrition, and having a positive mental attitude.
It is my contention that being a doctor of chiropractic is one of the most noble and rewarding professions that one can pursue. The care that chiropractors provide can have a profound impact on their patients’ lives. Chiropractic is a service profession, and people with a wide variety of conditions and Health challenges will seek care. Because of the nature of upper cervical specific care, doctors using these methods may have a tendency to attract some patients who have to be managed in a unique fashion. Orthospinology care makes it easier for the doctor to modify the patient’s Adjustment and care because the quantitative analysis provides detailed information about the nature of the Subluxation.
The limited amount of force used with the orthogonally based upper cervical Adjustment may make this procedure a viable choice for certain patients with complicated conditions. Patients are adjusted in a somewhat neutral position. It is important that the doctor is prepared to help these challenging patients before their arrival in his/her practice. The doctor is also cautioned to use this information as an aid as opposed to an absolute guide to patient management. Doctors must use clinical judgment to decide the appropriateness of each individual patient’s care, as well as to determine the need for medical referral.
Difficult Contacts
Location of the Atlas Transverse Process
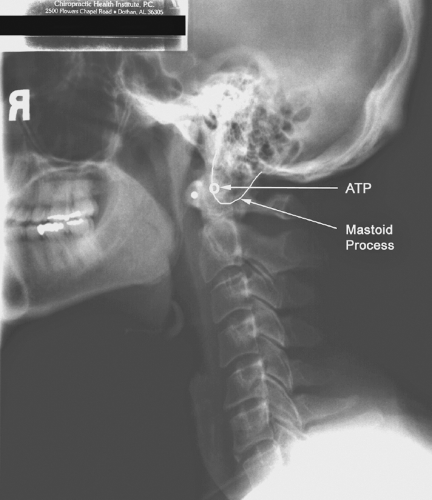
One of the most common challenges that an upper cervical chiropractor will face in practice is a patient who has a difficult atlas transverse process (ATP) contact. This usually results from congenital factors that can only be determined from careful X-ray analysis (see Chapter 4). The vast majority of patients will have an ATP contact point that is located within a region that is ¼ inch inferior and anterior to the inferior tip of the occipital Mastoid process (Fig. 14-4). It may be helpful to use the nasium film as an aid in finding the location of the ATP on the lateral view. Each ATP should first be outlined with an X-ray pencil on the nasium. The doctor should then observe the relationship between the ATP and the Atlas plane line as far as how much of the contact point lies above or below this reference line. This information
should be transposed to the lateral cervical film to determine if this same relationship exists between the ATP and the S-line. If two ATP contacts are observed on the lateral view, the nasium and Vertex X-rays should be used to determine which side has a superior or inferior and/or anterior or posterior positioned ATP.
should be transposed to the lateral cervical film to determine if this same relationship exists between the ATP and the S-line. If two ATP contacts are observed on the lateral view, the nasium and Vertex X-rays should be used to determine which side has a superior or inferior and/or anterior or posterior positioned ATP.
The first decision that the doctor must make before adjusting a patient is to determine if there is a reasonable chance to deliver a force to the upper cervical spine that will result in a successful biomechanical correction. It is better to leave a patient in a subluxated state, then to increase the misalignment. Difficult contacts can also result from congenital abnormalities, such as basilar invagination and Platybasia. These types of cases will be discussed later in this chapter; however, upper cervical Adjustments are considered contraindicated for many patients with these and other conditions. This is typically based on the severity of the condition and the degree of neurological involvement for each individual case.
In some rare cases, patients may have extremely large Mastoid processes that can cover all or most of the ATP as it is viewed in the sagittal dimension (Fig. 19-1). However, most patients who have at least part of the ATP accessible to contact can be adjusted by hand or with the use of an instrument. A difficult contact, as seen in Figure 19-1, can be adjusted manually if the atlas is subluxated anterior on the side of laterality. A posterior Listing would usually be too difficult to contact because of the Mastoid process. The doctor should slightly modify the Adjustment by removing almost the entire amount of elbow bend to reduce the depth with the hand Adjustment. This will help produce more control with the Adjustment and aid in a successful correction.
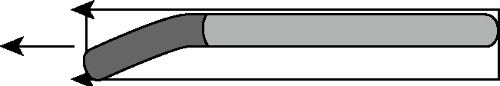 FIGURE 19-2 Bent stylus functions like a rigid body with vertex of force transmitted in a rectilinear direction. |
Using Various Handheld Instrument Styli with Difficult Contacts
The use of the Handheld instrument may be the most effective choice for most cases with a difficult contact. Various styli can be used with the instrument, depending on the Subluxation and type of contact that must be addressed. A Bent stylus may be used for patients who have a posterior Subluxation. This will enable the doctor to position the stylus over and around the Mastoid process so that a force can be introduced from a posterior to anterior direction into the ATP. Another benefit of the Handheld instrument is that the diameter for most of the styli tips is small in comparison with the pisiform of the doctor’s hand. The size of the stylus helps the doctor position the instrument so that appropriate contact is made, particularly with cases where the ATP is located high up in the Atlas fossa. Various styli are also available that come with beveled edges to aid with certain difficult ATP contacts.
A Bent stylus is also helpful if the Resultant angle is very steep (e.g., ≥30°). A large Resultant angle makes it difficult to make a solid contact because the skull gets in the way when the instrument has to be tilted to a large degree. Too much of the force may be directed across the neck as opposed to into the neck. The design of the Bent stylus helps remedy this situation. The stylus acts like a rigid body even though it is in a bent configuration (Fig. 19-2); thus, the vertex of force that is transmitted to the ATP travels in a rectilinear direction.
Cervical Herniated Disc
The cervical disc is different anatomically from the lumbar disc. The nucleus pulposus (NP) at birth constitutes no more than 25% of the cervical disc, as opposed to 50% of the lumbar disc. Aging causes the cervical nucleus pulposus to undergo fibrosis so that little nuclear material remains by the third decade of life.1 Clefts tend to develop in the cervical disc as people age, accompanying disc degeneration.2 This cleft development may help explain why adults can develop cervical
herniated nucleus pulposus (HNP) even if there is a relative paucity of water in the nucleus. In addition to the presence of discal clefts, tears may develop in the annulus that can contribute to the formation of a channel through which the nucleus pulposus migrates. If these channels extend to the periphery of the annulus fibrosus, the nucleus has a path through which it can herniate. This can then cause irritation and/or compression of the nerve root, depending on whether there is actual physical pressure present or whether there is merely chemical irritation.
herniated nucleus pulposus (HNP) even if there is a relative paucity of water in the nucleus. In addition to the presence of discal clefts, tears may develop in the annulus that can contribute to the formation of a channel through which the nucleus pulposus migrates. If these channels extend to the periphery of the annulus fibrosus, the nucleus has a path through which it can herniate. This can then cause irritation and/or compression of the nerve root, depending on whether there is actual physical pressure present or whether there is merely chemical irritation.
Cervical HNP has an incidence in the asymptomatic general population of ≤10%.3,4 This incidence is much less than that found in the lumbar spine (20%–36%),5,6,7 so it is somewhat rare for one to have an HNP in the cervical spine and not have symptoms. The symptomatic expression in one case study was ipsilateral popliteal pain caused by a cervical HNP.8 Patients knowingly or unknowingly have cervical HNPs and present to chiropractors for care. According to a 1996 survey,9 93% of all responding chiropractors reported that they would manipulate the spines of patients either known to have or suspected to have cervical HNP. Less than 2% of respondents never perform cervical Manipulation, and 67% would attempt to directly manipulate the involved segment in patients who have cervical HNP.9 A multitude of case studies10,11,12,13,14,15,16,17,18—and even a prospective clinical case series19—have been published showing the successful management of patients with cervical HNP by doctors of chiropractic. Case studies have also demonstrated the successful outcome of patients under chiropractic care for postsurgical neck syndrome.20,21 However, comanagement with a neurosurgeon or orthopedic surgeon may be necessary if the patient presents with serious neurological deficits and/or the patient fails to respond to chiropractic care in a reasonable amount of time.
Medical studies have indicated that most patients with cervical HNPs and radiculopathy can be treated conservatively with good results.22,23 Surgery is indicated only when appropriate conservative treatment for a reasonable time has failed.23 High patient satisfaction with nonoperative care has also been demonstrated.22 It should be noted that various medical authors have reported an apparent association between cervical Manipulation and the cause of cervical HNP or the aggravation of a pre-existing condition.24,25,26,27,28,29,30,31 However, many of these cases have resulted from Manipulation performed by nonchiropractors. Specific Adjustments performed by doctors of chiropractic have not been demonstrated to be a significant risk of complications related to cervical HNPs. Indeed, chiropractic is a profession and not a modality (i.e., Manipulation, Adjustment), and nonqualified personnel should not provide this care.
Orthogonally based upper cervical care has been shown to be an effective method of spinal care in the management of patients with cervical HNPs.15,32,33 One case study presented the chiropractic management of a patient suffering from multiple symptoms, including a C6-C7 HNP.15 This 34-year-old man suffered from severe neck, lower-back, and radicular pain of 1 year duration, and he had previously received care from multiple medical specialists with little or no results. A needle electromyogram examination confirmed the presence of a C6-C7 radiculopathy with radiculopathic changes from C4-C7. The patient was managed with Grostic procedure hand Adjustments, and after 1 week, he was significantly better. After 1 month, a series of re-examinations revealed a dramatic improvement in all subjective and objective findings. This care involved minimal force, and the Adjustment was conducted in the neutral side posture position without placing the cervical spine in a rotated or stressed position. It is proposed that this type of care may be safer than standard cervical Manipulation, although more studies are necessary to determine the effectiveness of each method.
 FIGURE 19-3 Patient suffering with spasmodic torticollis (cervical Dystonia). (From Eriksen K. Upper Cervical Subluxation Complex. Baltimore: Lippincott Williams & Wilkins, 2004:366.) |
Torticollis
The term torticollis comes from the Latin torti, meaning twisted, and collis, meaning neck (Fig. 19-3). It is thought to be caused by unilateral spasm of the sternocleidomastoid (SCM) muscle, which typically causes ipsilateral head tilt with contralateral head rotation. Torticollis can be congenital or acquired, although the etiology of the former cause in many cases is unclear and is likely attributed to birth trauma that damages the SCM muscle. Medically defined Atlantoaxial rotatory subluxations (AARSs) have been associated as a possible cause of torticollis,34,35,36,37,38,39,40,41,42,43
although Hicazi et al.44 have come up with conflicting data. Dystonia is a neurologic movement disorder characterized by sustained muscle contractions, usually producing twisting and repetitive movements or abnormal postures or positions. Dystonic movements are directional, forcing the involved body part or region into an abnormal position, which is typically sustained. Dystonia may affect muscles throughout the body (generalized) or in certain parts of the body (segmental), or may be confined to particular muscles or muscle groups (focal). This disorder may affect any part of the body, including the arms and legs, eyelids, face, neck, and vocal cords. Spasmodic torticollis is considered to be one form of Dystonia.
although Hicazi et al.44 have come up with conflicting data. Dystonia is a neurologic movement disorder characterized by sustained muscle contractions, usually producing twisting and repetitive movements or abnormal postures or positions. Dystonic movements are directional, forcing the involved body part or region into an abnormal position, which is typically sustained. Dystonia may affect muscles throughout the body (generalized) or in certain parts of the body (segmental), or may be confined to particular muscles or muscle groups (focal). This disorder may affect any part of the body, including the arms and legs, eyelids, face, neck, and vocal cords. Spasmodic torticollis is considered to be one form of Dystonia.
Atlantoaxial Rotatory Fixations
Some patients with neglected cases of torticollis can develop Atlantoaxial rotatory fixations (AARFs), which is a condition that involves a fixed rotation of C1 on C2. AARFs can also be caused by trauma (primarily rotational) and even upper respiratory infections that cause a local soft tissue response, which can result in ligament laxity and nonphysiologic motion.45,46 Corner47 first described this type of condition in 1907, when he reviewed 20 cases, although several reports have since been published.46,48,49,50,51,52,53,54,55,56 In 1977, Fielding and Hawkins48 provided a more precise description of the pathologic anatomy of AARFs, including a classification system. Type I involves no atlas anterior displacement, and the axis odontoid acts as a pivot. Type II has an anterior atlas displacement of 3 to 5 mm, and one articular process acts as a pivot. Type III has an anterior displacement that exceeds 5 mm, and type IV involves an atlas posterior displacement.
The diagnosis of AARF is usually delayed because of difficulty in taking appropriate radiographs caused by the patient’s postural distortion. Radiographic assessment (preferably cineradiography) should reveal that the posterior arches of atlas and axis move as one unit when the cervical spine is rotated.48,57 An asymmetry of the atlantodental interval of more than 4 mm is also one of the diagnostic signs for AARF.52 However, this condition can occur with or without anterior displacement of the atlas on the axis. Unlike torticollis, AARF patients usually have no muscle spasm on the side opposite the head tilt. There is usually an inability to passively or actively move the head beyond vertical. AARFs can also be considered to be severe, long-standing AARSs that typically cause torticollis. Subach et al.58 discuss one way of assessing the AARSs is to palpate the C2 spinous process to determine which way it moves with head rotation. Normal axis spinous process movement is contralateral deviation after about 20° of head rotation. They have typically observed ipsilateral spinous process deviation with AARSs. This observation is similar to what has been noted clinically in upper cervical practice (see Chapter 16). These medical authors view this as a compensatory mechanism of the body trying to restore the midline axis.
AARFs are most common in children probably because of various factors that may predispose them to this condition or upper cervical Subluxations in general. First, children’s ligaments and joint capsules possess sufficient elasticity to allow Hypermobility without disruption.53,59 Second, their atlantoaxial facet joints are shallower and more horizontally oriented than those of adults. The articular cartilage of these Articulations gives the opposing surfaces a nearly convex appearance and allows greater freedom of motion. Also, the uncinate processes of the pediatric spine are poorly developed and may allow excessive lateral flexion and rotation. Finally, the disproportion between the size of the child’s head and the Hypermobility of the cervical spine with minimally developed posterior cervical musculature may predispose the upper cervical spine to excessive forces, nonphysiologic motion, and AARFs.60 The head of a child reaches almost 90% of adult size by age 2.40 Meniscus-like synovial folds have been found in the occipitoatlantal and atlantoaxial facet joints of children’s spines but not in those of adults, and this is thought to be a contributory mechanism in the development of AARFs.53
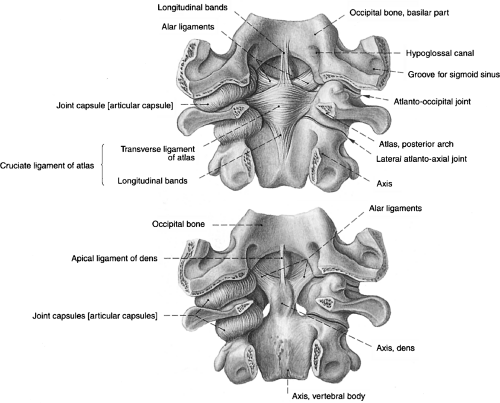
The atlantoaxial Articulation accounts for about 45% to 50% of cervical rotation. The alar ligaments arise from the tip of the dens and extend obliquely upward and laterally, inserting into the medial sides of the occipital condyles and atlas (Fig. 19-4). The alar ligaments limit or check rotation and lateral flexion of the occipitoatlantal and atlantoaxial joints and are therefore referred to as check ligaments. The left alar ligament controls right axial rotation and vice versa. Rotational stability of the atlantoaxial Articulation is also provided by the joint capsules of the lateral facet joints. Rotational movement of the atlas on the axis is a complex coupling movement, which involves a screwlike action in which the atlas drops vertically about 2 to 3 mm. Coupled with rotation is a slight amount of lateral flexion to the same side.61
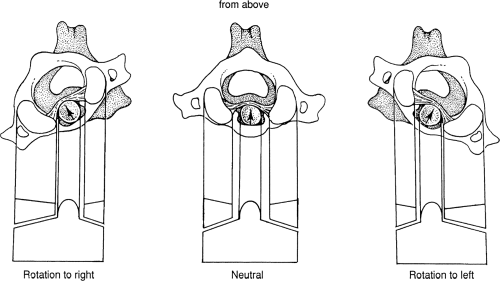
Severe atlantoaxial Subluxations will project on an anterior to posterior (AP) radiograph in a unique manner. Disregarding Atlas laterality, when the atlas rotates or is severely misaligned to the right and anterior, this can also be described as left and posterior because the axis of rotation is usually around the axis dens. In this case, there will be an apparent increase in the distance between the left lateral mass and the dens (atlantodental interval) as seen on an AP film. The oblique lateral mass appears to be narrow as it is viewed on end. The right lateral mass appears to be wider because it is viewed broadside with an apparent narrowing of the distance between the atlas and the odontoid. The opposite is true for rotation to the other side (Fig. 19-5).
Chiropractic Management of Torticollis and Atlantoaxial Rotatory Fixations
The severe misalignment component of the AARF is usually a Subluxation (from a medical definition) but can be a dislocation in extreme cases. This malposition causes adaptive changes in the subaxial vertebrae, which can lead to increased biomechanical stresses and subsequent early degenerative changes.46 Medical treatment consists of traction, medication, and surgery in many cases. The risks involved with medication and surgical intervention are well understood; however, cervical traction poses a potential serious risk as well.51 Moderate to severe cases of AARF should be comanaged with an orthopedic surgeon or neurosurgeon. Indeed, the chiropractor should use great care, with precision and gentleness, if the patient’s case is stable enough to undergo a trial of low-force upper cervical care. Knutson62,63 has presented two cases that have responded successfully to a course of Grostic upper cervical care. Kukurin64 reported the successful management of a patient with cervical Dystonia resulting from primarily two chiropractic procedures—applied biostructural therapy and atlas coccygeal technique. These same techniques have also been shown to be helpful in managing a patient with Cervical stenosis.65
A case study in the medical literature has shown an association between AARS and primary Dystonia.66 Patients with torticollis or various forms of Dystonia will occasionally present to a chiropractor’s office, but the management of such patients may prove precarious if the doctor is not prepared. Chapter 3 described the modified radiographic protocol that is necessary to obtain acceptable X-rays for patients with torticollis-like distortion (Fig. 3-9). Most patients with torticollis or other types of Dystonia can be placed on the adjusting table in the standard procedure as long as the doctor takes his/her time and is delicate in handling the patient. However, because of extreme postural distortion and/or severe pain, it may not be possible to place a patient in the standard side-posture position. In these cases, the chiropractor may decide to provide various forms of physical therapy to temporarily improve the patient’s muscle tension and/or pain. In extreme cases, the patient can be referred to a medical physician for pain medication that may help the chiropractor to perform an accurate Adjustment.
Another option involves using a modified Adjustment performed while the patient is in a seated position. In 1995, Dr. Cecil Laney presented a method for adjusting the atlas that was recommended only in rare situations in which a doctor was not able to receive or provide a standard upper cervical Adjustment.67 The procedure begins with placing the neck in slight extension while laterally flexing the neck to the left (for a right Atlas laterality Listing). The tip of the right middle finger is placed as high under the right ear lobe as possible. Mild to moderate pressure is applied straight in and held. Next, the neck is moved from left lateral flexion to right lateral flexion with a speed of about 1 second, while at the same time moving the finger straight down about ¼ to 3/8 inch.
Laney presented five sets of post-nasium film taken on himself (taken at different times) at the Upper Cervical Spine Conference, which revealed a near complete reduction of the upper cervical misalignments using this procedure. Dr. Kevin James has presented a case report of two patients with severe torticollis.68 James used the fingertip-modified Adjustment because both patients were unable to be positioned properly on the adjusting table. Post–X-rays revealed a satisfactory correction that enabled the patient to be placed in the side-posture position and then receive a standard Orthospinology Adjustment. James reported that both patients responded to care and recovered rather quickly from their torticollis state.
Cervical Laminectomies
A Cervical laminectomy is just what the name implies—the removal of the lamina(e) of the cervical vertebra(e). This surgical procedure is usually done to relieve pressure on the spinal cord or the nerves emerging from it, or to allow access to the spinal cord to complete another operative procedure. Laminectomies of the spine usually involve two or three spinal segments. However, I have taken care of a handful of patients with complete laminectomies from C1 to C7 and even part of the occiput in a couple of cases. I happen to practice in the same city where a controversial neurosurgical technique was partially developed to treat patients with severe Fibromyalgia and chronic fatigue syndrome (CFS). A family practitioner from Dothan, Alabama, obtained relief from CFS-like symptoms after receiving complete cervical laminectomies from a neurosurgeon from the University of Alabama at Birmingham. The Wall Street Journal carried the story about these two doctors Working in collaboration.69
The theory was that many patients suffering from chronic pain syndromes were actually dealing with Cervical stenosis and/or Arnold-Chiari malformations. This results in compression or irritation of the spinal cord and/or brainstem. From the mid-1990s until 1999, about 300 patients from Dothan were referred to the neurosurgeon, with at least 90 receiving the controversial surgery. The surgical procedure cost about $30,000 and is obviously quite invasive. It appears that some patients received significant relief, although others were made worse (including partial paralysis), and many did not achieve significant change in their original symptoms. However, most all of the patients obtained a
disability after having the back part of the vertebrae in their cervical spine removed.
disability after having the back part of the vertebrae in their cervical spine removed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree