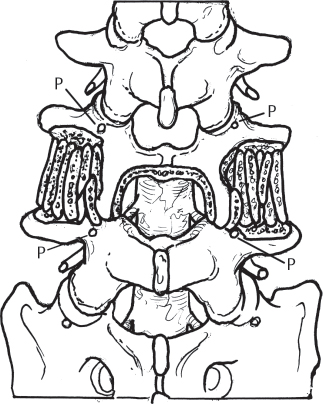
31 Lumbar degenerative spondylolisthesis is defined as the anterior subluxation of one vertebra relative to the adjacent inferior vertebra in the presence of an intact posterior neural arch. The subluxation results from degenerative changes involving the intervertebral disk and posterior facet joints. As the subluxation increases, secondary hypertrophy of the facet joints and ligamentum flavum contribute to spinal stenosis. The subluxation is usually limited to less than 30% by the intact neural arch and facet joints. Degenerative spondylolisthesis generally occurs in patients greater than 40 years of age. It is more common in females (female-to-male ratio 4:1), blacks (black-to-white ratio 3:1), and diabetic patients. Ninety percent of cases of degenerative spondylolisthesis occur at the L4–L5 level; 10% of cases occur at L3–L4 or L5–S1. Degenerative spondylolisthesis is frequently associated with sacralization of the L5 vertebra. Degenerative spondylolisthesis represents a heterogenous process with no universally accepted classification. A variety of factors, including disk space height, segmental motion on flexion-extension radiographs, segmental kyphosis at the level of slip, and the presence/absence of stabilizing osteophytes, have been used to stratify patients into broad treatment groups based on varying definitions of spinal instability. Presenting symptoms include neurogenic claudication, low back pain, and radicular pain. Neurogenic claudication presents as buttock and thigh pain or cramping pain associated with prolonged standing or walking. Relief of symptoms of neurogenic claudication is achieved by sitting or spinal flexion. Patients may also report numbness, heaviness, or weakness involving the lower extremities. Essential components of the physical examination of the patient with suspected lumbar degenerative spondylolisthesis include inspection, palpation, assessment of lumbar range of motion, and a complete neurologic examination, including lower-extremity sensation, motor strength, and reflexes. Physical examination should rule out nonspinal disorders (degenerative hip arthritis, peripheral vascular disease) that may mimic degenerative spondylolisthesis. Hip joint arthrosis may cause buttock and thigh pain that can erroneously be attributed to spinal stenosis. Assessment of hip joint range of motion and the presence of pain at the extremes of motion, especially internal rotation, can determine whether the hip joints are a source of pain and whether hip joint radiographs are indicated. If both hip arthritis and degenerative spondylolisthesis are present, injection of the hip joints under fluoroscopic guidance can aid in sorting out which problem is more symptomatic. Peripheral vascular disease can also cause symptoms of claudication. Assessment of lower-extremity peripheral pulses is an important part of the initial examination of adult patients with spinal disorders. Vascular claudication is associated with increased muscular exertion in the lower extremities independent of trunk position. Symptoms due to vascular claudication typically occur in the distal calf and foot and are not associated with back pain. Generally, these symptoms are exacerbated by walking and are relieved by stopping and standing and not specifically by sitting down or flexing the lumbar spine, as is the case with neurogenic claudication. Initial imaging studies should include standing anteroposterior (AP) and lateral lumbar radiographs, as well as lateral flexion-extension radiographs. Lumbar magnetic resonance imaging (MRI) is the preferred imaging study for evaluation of the spinal canal for neural compression. In patients who are unable to tolerate MRI (e.g., because of a pacemaker or claustrophobia), a computed tomographic (CT) myelogram is obtained. Parameters to assess on plain radiograph include the degree of subluxation, abnormal mobility at the olisthetic level, segmental kyphosis, and disk space height. In patients who have not undergone prior lumbar spine surgery, degenerative spondylolisthesis presents with a subluxation less than 50% (grade 1 or 2 slippage). Degenerative spondylolisthesis typically results in central spinal stenosis at the level of the subluxation as well as subarticular (zone 1) stenosis with compromise of the traversing nerve root. The exiting nerve root is generally spared from compression unless there is severe loss of disk space height. For example, L4–L5 degenerative spondylolisthesis results in central and subarticular spinal stenosis with compromise of the L5 nerve root (traversing nerve root of the L4–L5 motion segment). The L4 nerve root (exiting nerve root of the L4–L5 motion segment) is generally spared from compression unless severe loss of disk space height results in foraminal narrowing. Nonsurgical treatment options include nonsteroidal anti-inflammatory drugs (NSAIDs), physical therapy, orthoses, and injections. Physical therapy should include aerobic conditioning and exercises that emphasize lumbar flexion. Epidural corticosteroid injections are most likely to be effective for patients with significant lower-extremity symptoms rather than for patients whose predominant symptoms are in the low back. Surgical treatment is considered for patients who fail to improve with nonsurgical management or who present with progressive neurologic deficit, persistent or recurrent leg or back pain, neurogenic claudication, and significant reduction in quality of life. Imaging studies should be consistent with the diagnosis of degenerative spondylolisthesis with spinal stenosis, and the patient should be a medically appropriate candidate for spinal surgery. Surgical treatment options that are commonly considered for degenerative spondylolisthesis include (1) decompression; (2) decompression and posterior spinal fusion without spinal instrumentation; (3) decompression and posterior spinal fusion combined with posterior spinal instrumentation; and (4) decompression, posterior spinal fusion, and posterior spinal instrumentation combined with interbody fusion (anterior or posterior). Decompression for spinal stenosis associated with L4–L5 degenerative spondylolisthesis typically includes removal of the inferior half of the lamina of L4 and the superior half of the lamina of L5 to decompress central spinal stenosis (Fig. 31.1). Subsequently, the L5 nerve roots are decompressed by removing the medial half of the L4–L5 facet joint and accompanying ligamentum flavum. The decompression of the L5 nerve root is continued until mobility of the L5 nerve root is restored and a probe can be passed easily through the neural foramen. The L4 nerve root and neural foramen should also be checked for potential compression. Posterolateral fusion is the type of fusion most commonly performed for degenerative spondylolisthesis. After decompression is completed, the transverse processes of L4 and L5 are exposed and soft tissue is removed from their surfaces as well as from the intertransverse membrane. Decortication of the transverse processes is performed with a curette or burr to expose cancellous bone. Bone graft is applied to the intertransverse region to complete the fusion procedure (Fig. 31.1). Iliac crest autograft is the traditional gold standard for bone graft material. Some surgeons use only local bone obtained during decompression and increase the graft volume through addition of a bone graft extender (e.g., demineralized bone matrix). Recently, recombinant human bone morphogenetic protein-2 (rhBMP-2) has been utilized in an off-label fashion (per the United States Food and Drug Administration) as the sole graft material in the intertransverse region with similar outcomes compared with iliac autograft. If posterior instrumentation is used, a facet fusion may also be performed. However, if no instrumentation is used, facet disruption may increase the risk of postoperative instability. Fig. 31.1 Posterolateral L4–L5 fusion and central canal decompression. P, pedicle.
Lumbar Degenerative Spondylolisthesis
![]() Classification
Classification
![]() Workup
Workup
History
Physical Examination
Spinal Imaging
![]() Treatment
Treatment
Nonsurgical
Surgical
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







