Layer
Name
Structure
Purpose
Pathology
I
Osteochondral
Innominate
Joint congruity
Developmental
Dynamic
Acetabulum
Joint kinematics/biomechanics
Dysplasia
Cam/Rim impingement
Femur
Acetabular Profunda/protrusio
Trochanteric impingement
Sub-spine impingement
Femoral/acetabular version
Delamination
Femoral inclination
II
Inert
Capsule
Static stability
Capsular instability
Labrum
Labral tear
Ligamentous complex
Ligamentum teres tear
Ligamentum teres
Adhesive capsulitis
III
Contractile
Peri-articular
Musculature
Dynamic stability
Hemi-pelvic pubalgia
Lumbosacral
Musculature
Hip flexor strain
Pelvic Floor
Anterior enthesiopathy
Psoas impingement
Rectus femoris impingement
Medial enthesiopathy
Adductor tendinopathy
Rectus abdominus
Enthesiopathy
Posterior enthesiopathy
Hamstring strain
Lateral enthesiopathy
Peri-trochanteric disorders
Gluteus medius tear
IV
Neuromechanical
Neurovasculature of the pelvic girdle and hip
Biofeedback
Neural
Mechanical
Timing and sequencing of kinematic chain
Nerve entrapment
Scoliosis
Referred spinal
Ambulation/foot structure and mechanics
Mechanoreceptors
Perfusion
Pathology
Pelvic posture
Thoraco-lumbar and lower extremity mechanics
Neuromuscular dysfunction
Osteitis pubis
Regional pain syndromes
Sacroiliac dysfunction
Pubic symphysis dysfunction
Table 2
Differential diagnosis of hip pain
Traumatic injury | Fracture or stress fracture |
Hip dislocation | |
Soft tissue contusion or hematoma | |
Labral injury | Trauma |
Femoroacetabular impingement | |
Hip joint hypermobility | |
Dysplasia | |
Cartilage Injury | Lateral impaction |
Loose body | |
Condral shear | |
Osteoarthrosis | |
Osteonecrosis | |
Capsule pathology | Capsular laxity |
Adhesive capsulitis | |
Capsular inflammation/synovitis | |
Synovial proliferative disorders | Pigmented villonodular synovitis |
Synovial chondromatosis | |
Chondrocalcinosis | |
Inflammatory conditions | Rheumatoid arthritis |
Reiter syndrome | |
Psoriatic arthritis | |
Infection | Septic arthrosis |
Osteomyelitis | |
Tumor | Benign soft tissue neoplasm |
Benign osseous neoplasm | |
Malignant soft tissue neoplasm | |
Malignant osseous neoplasm | |
Metastatic disease | |
Metabolic disorders | Paget’s disease |
Primary hyperparathyroidism | |
Extra-articular musculoskeletal disorders | Coxa saltans |
Trochanteric bursitis | |
Athletic pubalgia | |
Abductor impingement | |
Psoas impingement | |
Ischial bursitis | |
Osteitis pubis | |
Tendonitis (flexors, abductors or adductors) | |
Sacroiliac pathology | |
Non-musculoskeletal disorders | Inguinal hernia |
Spine pathology (myelopathy, radiculopathy) Iliopsoas muscle abscess | |
Intra-abdominal pathology (endometriosis, ovarian cyst) | |
Peripheral vascular disease | |
Unknown etiology | Transient osteoporosis of the hip |
Bone marrow edema syndrome |
Layer 1: Osteochondral Layer
This deep layer of the hip comprises the osseous and chondral structures, which function to provide joint congruence and osteoarticular kinematics in the normal hip. The bony structures that encompass this layer include the pelvis, acetabulum, and femur. Structural pathologies exist within this layer and can be classified into three distinct groups: (1) static overload, (2) dynamic impingement, and (3) dynamic instability [1–8]. Numerous anatomic variations may result in static overload, including lateral or anterior acetabular undercoverage (acetabular dysplasia), acetabular protrusio, excessive femoral anteversion, relative femoral retroversion, excessive acetabular retroversion/excessive anteversion, and coxa vara/valga. These anatomic variants change the structural mechanics and may predispose the articular cartilage to eccentric loading, with subsequent abnormal or increased stress and asymmetric loads between the femoral head and acetabular socket in the axially loaded, standing position.
During terminal hip motion, hip pain may present due to abnormal stress and contact between the femoral head and acetabular rim. Structural variants within layer 1 that may contribute to such dynamic impingement include femoroacetabular impingement (FAI; cam-type, pincer-type, or combined), relative femoral retroversion, and coxa vara. When the required range of motion for competition in sports or for daily activities exceeds the limits of an individual’s physiologic motion imparted by the anatomic structures of the hip, a compensatory increase in motion may be provided through layer 1. Specifically, increased motion and consequential stresses through the pubic symphysis, sacroiliac (SI) joints, and lumbar spine may occur. Compensatory injuries in the form of lumbar spondylolysis, osteitis pubis, and SI joint strain have been well described in the setting of primary FAI. When functional range of motion requirements exceed the individual’s normal motion limits, forceful anterior contact occurring at the end range of internal rotation may also lead to dynamic instability in the form of subtle repetitive posterior hip subluxations as the femoral head levers out of the hip socket [1, 9]. An appropriately aligned anteroposterior (AP) pelvic radiograph in addition to a lateral view of the proximal femur (modified Dunn or frog-leg lateral) and/or a false profile view allows the treating physician to systematically assess the bony anatomy of the acetabulum and proximal femur. Various described radiographic indices such as Tönnis osteoarthritis grade, minimum joint space, lateral center-edge angle, anterior center-edge angle, Tönnis angle (acetabular inclination), alpha and beta angles, and presence/absence of crossover, posterior wall, and prominent ischial spine signs may better delineate the bony anatomy and thus facilitate a correct mechanical diagnosis [10–16].
Topographic Bony Anatomy
The evaluation of the osteochondral layer of the young adult with hip pain begins superficially with the bony landmarks about the hip. The principal bony landmarks that are identified include the pubic symphysis, anterior superior iliac spine (ASIS), iliac crest, posterior iliac spine, greater trochanter, and ischium (Fig. 1). These landmarks serve as reference points for the deeper soft-tissue structures during the physical examination. The greater trochanter and the ASIS also have been described as the two key landmarks for accurately establishing portals during hip arthroscopy should surgical treatment be warranted.
Fig. 1
Bony landmarks (marked with stars) which may be palpated during the examination of the hip to provide frame of reference include anterior superior iliac spine, pubic symphysis, iliac crest, posterior iliac spine, and ischial tuberosity (From Mathers LH, et al. Clinical Anatomy: Principles. St. Louis: Mosby; 1996. Copyright Elsevier)
Osteology of the Hip Joint
Both the proximal femur and pelvis are preformed in cartilage. Three of the eight acetabular ossification centers ultimately fuse to create the osseous acetabulum. The iliac, ischial, and pubic ossification centers form the triradiate cartilage. The iliac ossification center is the first to appear at approximately 9 weeks of intrauterine development, while the ischial and pubic centers appear at 16 and 20 months, respectively. At birth, the acetabulum remains a cartilaginous structure, and it is not until 8–9 years of life that the acetabulum transitions from a cartilaginous to full osseous structure. Fusion of the cartilage centers reaches completion around 16–18 years of life [17, 18].
The two ossification centers of the proximal femur (the femoral epiphysis and the trochanteric apophysis) are not present during prenatal life; however, they both become apparent during the first year of life. The femoral epiphysis ossification center is offset laterally within the femoral head. In early development, the AP diameter is greater than the transverse dimension. At the age of 3 years, the AP and transverse dimensions are equivalent. After 3 years of age, the femoral head becomes ovoid with the transverse diameter becoming larger than the AP diameter [19, 20].
The developmental osteology of the hip and acetabulum has been studied from early postnatal life and into adulthood, and these changes have implications on the degree of femoral head coverage by the acetabulum. Horii et al. [21] demonstrated the difference in the degree of femoral head coverage between children, adolescents, and adults, suggesting that global osseous acetabular coverage of the femoral head is greater in adults than in children and adolescents. However, when taking into account the acetabular labrum, the total femoral head coverage is greater in children than in adults [21].
An understanding of the normal anatomic positions of the acetabulum and femoral head is also important. The acetabular articular surface, or lunate fossa , is horseshoe-shaped, with the central-inferior portion devoid of articular cartilage. This bare area is the location of the acetabular attachment of the ligamentum teres, which is surrounded by a synovial fat pad, also known as the pulvinar. The horseshoe-shaped acetabulum is completed by the transverse acetabular ligament inferiorly, which is continuous with the labrum (Fig. 2) [17].
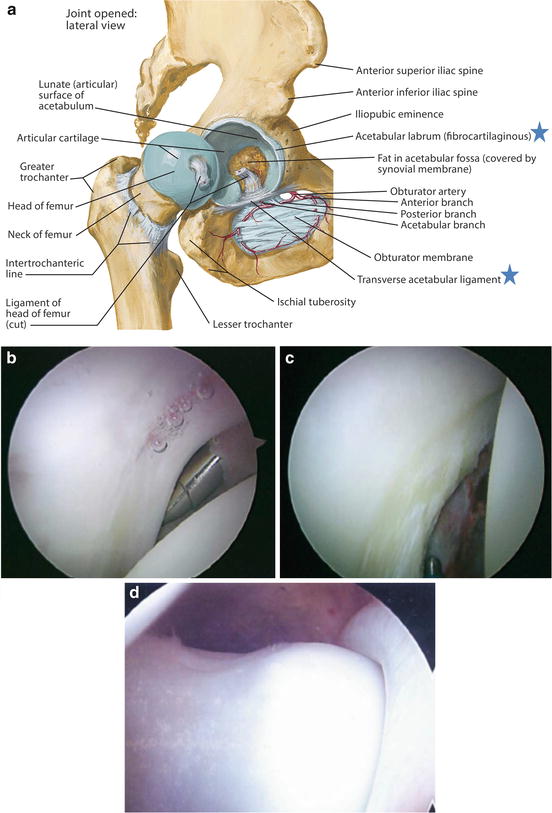
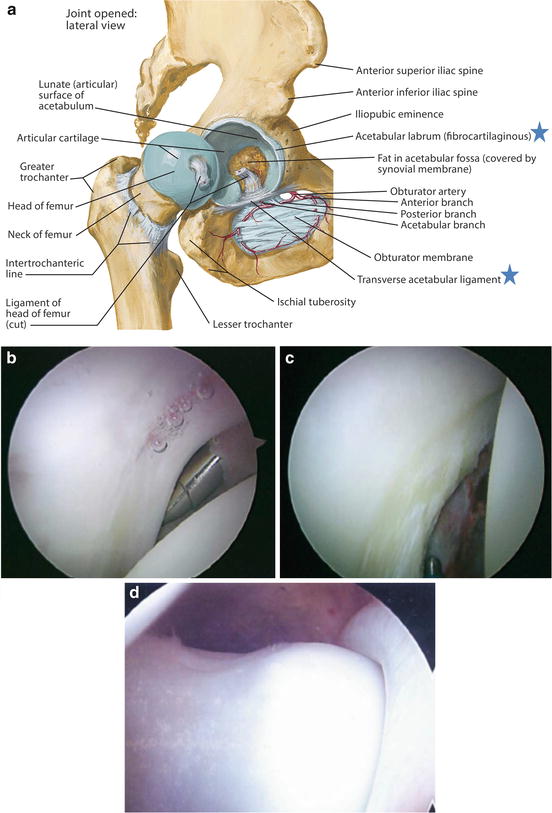
Fig. 2
(a) Illustration of the acetabulum and femoral head, with the hip dislocated to identify the acetabular labrum and transverse acetabular ligament (marked with stars). Netter illustration from www.netterimages.com. ©Elsevier Inc. All rights reserved. (b) Arthroscopic view of the anterior labrum from a posterolateral viewing portal. (c) Arthroscopic view of the posterior labrum from an anterolateral viewing portal. (d) Arthroscopic view of the “suction seal” effect of the labrum (b–d) (From Ranawat AS, Kelly BT. Anatomy of the hip: Open and arthroscopic structure and function. Oper Tech Orthop. 2005;15(3):160–174. Copyright Elsevier)
The proximal femoral anatomy can be quite variable; however the neck-shaft angle averages 125° with approximately 14° of femoral neck anteversion [22]. The femoral head articular cartilage is often described as covering the equivalent of two-thirds of a sphere. The cartilage is congruous except for a shallow depression in the inferomedial aspect of the head. This small area devoid of cartilage is known as the fovea capitis and anatomically serves as the femoral attachment of the ligamentum teres [17].
Deviations from the normal development and morphologic relationships of the bony acetabulum and proximal femur may result in a mechanical conflict within the hip joint. This conflict can span a continuum from hip joint “undercoverage” (dysplasia) to hip joint “overcoverage” (femoroacetabular impingement) [1, 4, 5]. The specific pathology that results in a femoral and acetabular mismatch can be further differentiated by its primary factor, either static or dynamic [1].
Static mechanical factors may result in abnormal stress within the hip joint and asymmetric load across the hip joint either in the standing or axially loaded position. Bony pathologies most often associated with static mechanical stress are lateral acetabular undercoverage, anterior acetabular undercoverage, and excessive femoral anteversion and femoral valgus. The mechanical stresses in the aforementioned conditions may lead to asymmetric loading and thus premature wear of the chondral surfaces of the acetabulum and femur [1, 23–25]. This primary bone and cartilage mechanical stress may lead to compensatory muscular injury/overload (abductors, iliopsoas, and adductors) as the periarticular musculature attempts to stabilize the mismatched anatomy of the hip joint and subsequently affect the superficial layer 3, which will be discussed later in this chapter.
In the setting of dynamic mechanical disorders, range of motion of the hip causes contact between the femoral head and acetabular rim. The bony abnormalities most often associated with dynamic mechanical overload are a cam-type or pincer-type (focal, global retroversion, profunda, protrusio) deformity, relative femoral retroversion, or coxa vara. The mechanical stresses of the above pathologic conditions primarily result in hip and groin pain. When the athletic demands on the hip are greater than the functional range of motion, compensatory stresses and subsequent pain may develop in the lumbar spine, pubic symphysis, sacroiliac joints, and posterior acetabulum [1]. This compensatory stress also places demands on the periarticular musculature, which may also lead to muscle injury of the adductor longus, proximal hamstrings, abductors, iliopsoas, and hip flexors (layer 3) [26].
Layer 2: Inert Layer
The resultant mechanical stresses of the previously described layer 1 may lead to reactive hip pain related to insufficient congruency or impingement between the femoral head and the acetabulum. Thus, the morphology of layer 1 has a direct effect on the inert layer, or layer 2, of the hip.
Layer 2 includes the acetabular labrum, joint capsule, ligamentous complex, and ligamentum teres. These structures are all contributors to the static stability of the hip joint. When abnormal mechanical stresses are applied to the hip joint secondary to underlying abnormalities within layer 1, the resultant pathology may present in layer 2. These pathologies include labral injury, ligamentum teres tears, capsular injury, and consequent instability or adhesive capsulitis. Magnetic imaging resonance (MRI), usually with an arthrogram, is the best imaging modality to help evaluate the chondral, labral, and capsular damage. With an understanding of the underlying structural mechanics of layer 1, in combination with knowledge of the activity-specific range of hip motion, one can predict the type of injury to layer 2 structures.
Capsular Structure and Function
The capsular complex is mainly composed of three discrete thickenings. The three discrete bands of capsule are the iliofemoral, ischiofemoral, and pubofemoral ligaments (Fig. 3). These three ligaments each originate from one of the three named bones of the pelvis. Their function is to effectively encapsulate the hip joint from acetabulum to the intertrochanteric ridge. From the acetabular origins, the capsule extends laterally to surround the femoral head and neck and fans out to insert broadly on the proximal femur. The femoral insertions extend anteriorly onto the intertrochanteric line, superiorly onto the base of the femoral neck, posteriorly superomedial onto the intertrochanteric crest, and inferiorly onto the femoral neck [17].
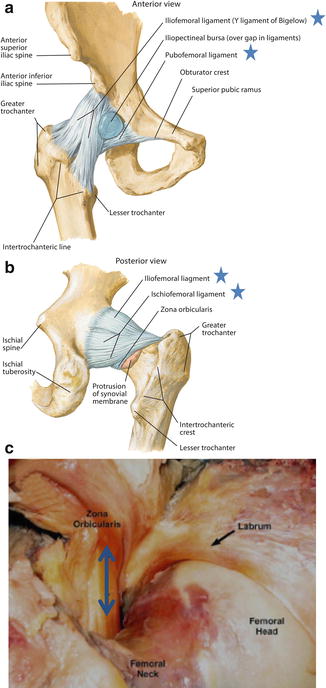
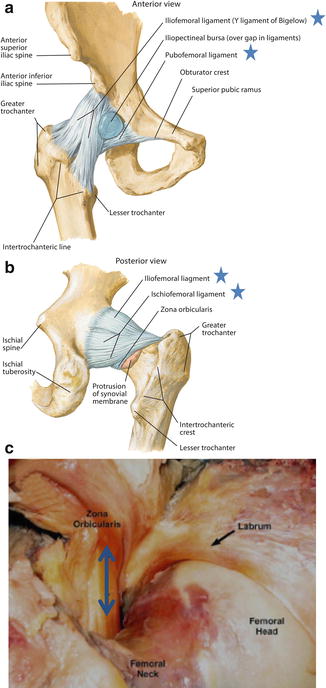
Fig. 3
Illustration of the (a) anterior capsular complex and (b) posterior capsular complex; iliofemoral ligament, ischiofemoral ligament, and pubofemoral ligament are marked with stars. Zona orbicularis present on the posterior view and denoted with red underline. Netter illustrations from www.netterimages.com. ©Elsevier Inc. All rights reserved. (c) Gross dissection of the capsular structures denoting the inner surface of the capsule and the undersurface of the zone orbicularis (marked with blue arrow) (From Bedi et al. Capsular management during hip arthroscopy: From femoroacetabular impingement to instability. Arthroscopy. 2011;27(12):1720–1731. Copyright Elsevier)
The iliofemoral ligament (Y-ligament of Bigelow) has two arms, comprises the anterior portion of the capsule and derives its name from its appearance as an inverted “Y.” From one common origin between the anterior-inferior iliac spine and the acetabular rim, it splits into a superior arm and an inferior arm as it crosses the joint [17, 27]. The superior arm travels horizontally and inserts proximally along the intertrochanteric line anterior to the hip joint. The inferior arm takes a vertical course and inserts caudally along the intertrochanteric line [28]. The iliofemoral ligament is the strongest and thickest of the three ligaments. Functionally, it provides restraint to anterior hip subluxation or dislocation, especially when the hip is in positions of extension and external rotation [17, 27]. In its contracted position, the iliofemoral ligament causes the hip to move into a flexed and internally rotated posture. Given its functionality, preservation or repair of the iliofemoral ligament at the conclusion of hip preservation surgery is preferred and may be especially relevant in patients with hyperlaxity, anterior instability, and/or acetabular undercoverage.
The ischiofemoral ligament comprises the majority of the posterior portion of the hip capsule. Generally, the ligament takes its origin from the ischial rim of the acetabulum and inserts around the posterior aspect of the femoral neck [27]. The ischiofemoral ligament also divides into two arms, with the more superior arm blending with the zona orbicularis fibers and the inferior arm inserting more posteriorly on the intertrochanteric crest [28]. In action, the main function of the ischiofemoral ligament is to resist internal rotation and adduction of the hip. In comparison to the iliofemoral ligament, the ischiofemoral ligament has less than half its ultimate load to failure [27–29].
The pubofemoral ligament takes its origin at the pubic portion of the acetabular rim and the obturator crest of the pubic bone before fanning out distally like in a sling-like shape to attach onto the femoral neck. Fibers of the pubofemoral ligament blend with the more medial arm of the iliofemoral ligament. As the ligament courses caudally, it inserts posteriorly on the femoral neck below the ischiofemoral ligament. In action, the pubofemoral ligament works in conjunction with the medial and lateral arms of the iliofemoral ligament, to control external rotation of the joint [17, 28].
In contrast to the longitudinally oriented fibers of the three constituents of the outer capsule (iliofemoral, ischiofemoral, and pubofemoral ligaments), the inner capsular fibers of the zona orbicularis run in a horizontal fashion as they circle the femoral neck (Fig. 3). This leash of capsule fibers acts like a locking ring around the femoral neck preventing femoral head distraction [30]. In a cadaveric study, Ito et al. [30] demonstrated that the zona orbicularis serves as the main hip stabilizer against distractive forces.
In addition to providing stability to the hip joint, the capsule provides protection to the articular cartilage and serves as the location for the blood supply to the acetabulum and femoral head. Four main blood vessels supply the hip capsule : the superior gluteal artery, the inferior gluteal artery, the medial femoral circumflex artery, and the lateral femoral circumflex artery (Fig. 4). The posterior hip capsule receives its major blood supply from the superior and inferior gluteal arteries as they descend from the pelvis. The anterior capsule is vascularized from the medial and lateral circumflex arteries as they ascend through the hip capsule [31]. In most cases, the medial femoral circumflex artery travels on to be the primary blood supply to the femoral head; however, a cadaveric study by Kalhor et al. [31] demonstrated the inferior gluteal artery to be the dominant blood supply to the femoral head in a minority of cases. In the majority of cases, the main blood supply to the femoral head originates distally at the capsular insertion, and thus overzealous dissection of the capsule either for exposure or instrumentation during hip procedures may lead to iatrogenic devascularization of the femoral head. Therefore, in cases where the capsule must be opened, either via capsulotomy or capsulectomy, the T-capsular split should be made between the medial and lateral synovial folds, which corresponds to the intermuscular plane between the iliocapsularis and gluteus minimus [17, 31].
Fig. 4
(a) Illustration of the major blood vessels to the hip (From Mathers LH, et al. Clinical Anatomy: Principles. St. Louis: Mosby; 1996. Copyright Elsevier). (b) Detailed illustration of the terminal branches of the medial femoral circumflex artery (MFCA). (1) Femoral head, (2) gluteus medius, (3) deep branch of the MFCA, (4) the terminal subsynovial branches of the MFCA, (5) insertion of gluteus medius, (6) piriformis insertion, (7) nutrient vessels to lesser trochanter, (8) the trochanteric branch of MFCA, (9) the branch of the first perforating artery, and (10) the greater trochanteric branches (From Gautier et al. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg [Br]. 2000;82-B:679–683. Reproduced with permission and copyright © of the British Editorial Society of Bone and Joint Surgery)
Labral Structure and Function
The labrum is a horseshoe-shaped fibrocartilaginous tissue that attaches to the bony rim of the acetabulum and effectively deepens the acetabular socket. The labrum is triangular in cross section with the apex forming the free edge closest to the joint center. The labrum terminates inferiorly at the anterior and posterior edges of the acetabular fossa. At the terminal edges, the labrum becomes contiguous with the transverse acetabular ligament (Fig. 2) [17]. The base of the triangular labrum (edge furthest from the joint center) attaches to the acetabular articular cartilage through a transition zone of calcified cartilage with a distinct tidemark [32]. The average labral thickness is reported to be 5.3 ± 2.6 mm [33]. However, labral thickness varies by location; the largest diameter is located at the posterosuperior aspect and the smallest diameter is in the anteroinferior aspect of the acetabular rim. The labrum is a neurovascular structure that receives its vascular supply from the exterior capsular attachments, which penetrate the labral tissue at its base. This vascular configuration leaves the central most region of the labrum with rather poor vascular perfusion and thus limited healing potential. Conversely, in similar fashion to the knee meniscus, the peripheral capsulolabral junction has the highest healing potential [34]. The labrum also contains free nerve endings that carry both proprioceptive and nociceptive fibers. This likely substantiates clinical results that suggest athletes with torn labral tissue have decreased proprioception and pain [35].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








