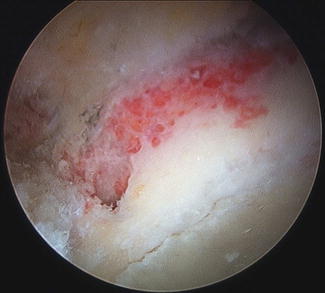
Fig. 1
The labral defect is identified and defined. A stump of native labrum is left to either side of the defect if possible to allow for anastomosis of the graft to the native labrum
Once the defect is defined, a motorized burr is utilized to prepare the acetabular rim. Recession for pincer lesion is performed as deemed necessary from the preoperative planning, and it is also common to decorticate the rim in the location of the defect to have a bleeding surface for the labral graft to adhere to during the healing process.
A distal anterolateral accessory (DALA) portal can be utilized for many parts of this procedure. It is useful for the anchor drilling sequence as it provides a more ideal trajectory to access the rim and also is useful for suture and graft management. It is created in line with the standard AL portal 3–4 cm distally and identified with a spinal needle. If the labrum is deficient in a more posterior position, it is useful to often establish a standard posterolateral portal which can be used to effectively deliver anchors to this location.
The defect is then measured prior to graft preparation or harvest. It is useful to mark a high-tensile suture at 5 mm increments with a surgical marking pen (Fig. 2). This marked suture is then introduced into the joint, and use two graspers to place it into the labral defect along the acetabular rim. The distance is then recorded and the graft is oversized by 5–7.5 mm to ensure the graft is of adequate length. Many labral defects will measure between 4 and 5 cm in length.
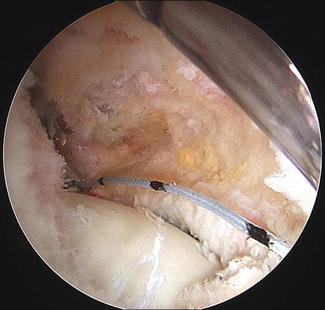
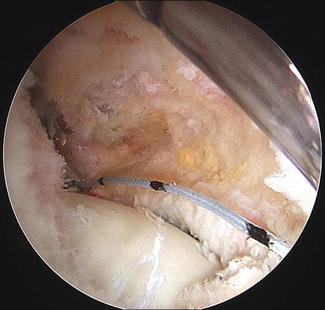
Fig. 2
The labral defect is measured with a high-tensile suture marked at 5 mm increments. Oversizing the graft by 5–7 mm is helpful in most cases
Once the defect size is known, the graft harvest is performed if using an autograft. If allograft is selected, a semitendinosus allograft (STA) or tibialis anterior tendon allograft (TAA) can be utilized depending on the size of the patient’s native labrum, and attempts are made to match this as close as possible with the graft selected. If autograft is preferred, an incision centered over the ipsilateral pes anserinus is made. The soft tissue above the sartorius fascia and bursal tissue are cleared, and the upper border of the gracilis tendon is identified. An L-shaped flap can be created to identify the tendons on the back side of the flap, or a split in the sartorius fascia can be made and the ST tendon identified. It is freed from its insertion of the tibia and the adhesions (usually at least two main connections to the gastrocnemius) are released. The tendon is then stripped with the use of a standard tendon-stripping instrument. On the back table, the muscle is stripped from the tendon.
The remainder of the procedure is identical for either allo- or autograft. On the back table, the most robust portion of the tendon is identified, and the graft is cut to the desired length as determined previously. In the case of a more robust native labrum, the tendon can be folded over and whipstitched to make a larger graft if desired. Often the native labrum is very close in size to the ST, and this doubling procedure is unnecessary.
Each end of the tendon is then whipstitched with a high-tensile suture. Leaving the stitches long will allow parachuting the graft into place, and by bringing the stitches out the posterior aspect of the graft a few millimeters shy of the absolute end, it facilitates anastomosis to the native labrum. A mattress type of suture is then placed in the center of the graft, so there are three total sutures at the end of the preparation. This graft is then placed on tension on the back table and protected while the pilot holes for knotless anchors are prepared.
While many anchor choices exist, this technique can be aided with PEEK knotless anchors. Once the graft is prepped, the first pilot hole is placed on the rim just behind the remaining native labrum at the superior aspect of the defect (Fig. 3). It is critically important to be able to visualize this hole later when shuttling the graft into place so a shaver or RF device can be used to clear soft tissue from the whole and define the pilot hole. This location can be accessed often from the DALA portal while looking from either the AL or MMA portal, the AL portal, or the PL portal if it is in a more posterior position. A second pilot hole is then drilled at the center of the labral defect, and a final hole is drilled just behind the anterior remnant. Often the majority of the time, all of these pilot holes can be drilled through the DALA portal with limited to no tension on the drill guide.