CHAPTER 3 Labral Pathology
Our understanding of labral pathology as a cause of hip pain is evolving. The exact prevalence of acetabular labral tears in the general population is unknown. Injuries to the acetabular labrum are the most consistent pathologic findings identified at the time of hip arthroscopy. In the review of their last 300 cases by Kelly and colleagues,1 labral tears were present in 90%. Labral tears are most frequently anterior and often are associated with sudden twisting or pivoting motions.
ANATOMY AND PATHOANATOMY
The hip labrum is a fibrocartilaginous structure that surrounds the rim of the acetabulum in an almost circumferential manner. It is contiguous with the transverse acetabular ligament across the acetabular notch. The labrum is widest in the anterior half, thickest in the superior half, and merges with the articular hyaline cartilage of the acetabulum through a transition zone of 1 to 2 mm.2 The labrum is firmly attached to the rim of the acetabulum. Its junction with the osseous margin is irregular, and there may be extension of bone into the substance of the labrum. A group of three or four vessels is located in the substance of the labrum on the capsular side of this bony extension from the acetabulum and penetrates into the peripheral third of the labrum. The labrum is separated from the hip capsule by a narrow synovium-lined recess.3 Extrapolating from our understanding of the healing capacity of the meniscus, repair strategies should be considered for tears involving only the peripheral labrum.
Function
We are only beginning to understand the function of the labrum. The bony congruity of the hip joint allows for primary stability. The labrum functions as a secondary stabilizer by extending the acetabular congruity and helping maintain the negative intra-articular pressure within the joint. This has been confirmed through a poroelastic finite model that showed the labrum helps provide structural resistance to lateral motion of the femoral head within the acetabulum.4 Furthermore, it has been demonstrated that the labrum decreases the contact pressures within the hip, probably as a result of its effect on maintaining the articular fluid in contact with the weight-bearing cartilage.5
Causes of Labral Tearing
There are many theories on the mechanism of labral tearing, suggesting that the cause is multifactorial. Kelly and associates1 have identified at least five causes of labral tears: (1) trauma, (2) femoroacetabular impingement (FAI), (3) capsular laxity and hip hypermobility, (4) dysplasia, and (5) degeneration.
Injury to the labrum could occur with traction, which would cause a tear resulting from excessive or repetitive external rotation of the femoral head on the anterior labrum.6 Compression forces may also tear the labrum through excessive and repetitive flexion and/or internal rotation of the hip. This process could be accelerated with FAI (see Chapter 4). Atraumatic instability has also been attributed to a deficient labrum associated with redundant capsular or ligamentous tissue that allows for more strain, and may transiently cause an incongruent joint. Deformities of the femoral head or acetabulum (e.g., slipped capital femoral epiphysis lesions, Legg-Calvé-Perthes disease, developmental dysplasia of the hip) have been discussed as a cause of labral tearing from incongruities between the femur and acetabulum.7
In the setting of a normal labrum, supraphysiologic loads would be required to produce a labral tear. Conversely, in the setting of an abnormal labrum, tearing could occur at physiologic loads. Sports that require repeated hip rotation, such as football, golf, gymnastics, soccer, ballet, and baseball, are susceptible to overuse injuries to the labrum and capsuloligamentous complex.8
Regardless of the mechanism, most labral tears encountered at the time of arthroscopy occur in the anterior quadrant. In a series by Fitzgerald,9 45 of 49 labral injuries were documented in the anterior marginal attachment of the acetabulum. These findings were supported by another study, which reported that 96% of labral tears encountered in a series of 436 consecutive hip arthroscopies occur in the anterior quadrant.10
The data from cadavers show that labral lesions are extremely common, present in 93% of specimens. Because the labrum is thought to be a stabilizing structure in the hip, labral lesions might contribute to the development of osteoarthritis in numerous ways. Injury or degeneration of the labrum may result in instability of the femoral head in the acetabulum, resulting in cartilage damage adjacent to the damaged labrum. This instability also might be more widespread, resulting in cartilage damage in the weight-bearing region of the acetabulum.6 Finally, the lack of a seal may affect cartilage density as a result of fluid loss from the central articular compartment.4
HISTORY AND PHYSICAL EXAMINATION
The clinical presentation of patients with a tear of the labrum is variable and, as a result, the diagnosis is often missed initially. Burnett and coworkers11 have reported on a series of 66 patients in whom the diagnosis of a labral tear had been made by arthroscopy. In this series, the mean time from onset of symptoms to diagnosis was 21 months. An average of 3.3 health care providers had seen each patient prior to their being diagnosed. Groin pain was the most common complaint (92%), with the onset of symptoms most often insidious. The most common examination finding was a positive impingement sign, which occurred in 95% of patients in this series.
Most patients who present with labral injury report activity-related groin pain in the affected hip. A few patients also report gluteal or trochanteric pain, secondary to aberrant gait mechanics. In some patients, the gluteal pain may be a sign of posterior labral injury. Although most patients do not specifically report loss of hip range of motion (ROM), this finding is almost universally seen. Hips with structural abnormalities, such as acetabular retroversion, coxa profunda, or pistol grip deformities, may have decreased ROM from anatomic limitations, but may also be limited by pain. Patients with pathologic hip conditions also commonly develop late capsulitis, synovitis, and/or trochanteric bursitis. Differential diagnosis of the classic mechanical symptoms (painful catching or clicking) of labral tears includes a snapping iliotibial tendon or hypermobile psoas tendon.1 Many other conditions can produce symptoms around the hip. The differential diagnosis should include an array of disorders such as sacroiliitis, degenerative disk disease, abductor muscle problems, osteonecrosis, psoas tendinitis, pubic rami fractures, and stress fractures of the proximal femur. More chronic problems are usually associated with trochanteric bursitis.12
In addition to functionally limiting symptoms, reproducible physical findings, and mechanical symptoms, restricted ROM from pain or a perceived mechanical block is a further indication of an intra-articular cause. Findings on physical examination can include a positive McCarthy sign—with both hips fully flexed, the patient’s pain is reproduced by extending the affected leg, first in external rotation and then in internal rotation. Also common is inguinal pain with flexion, adduction, and internal rotation of the hip, as well as anterior inguinal pain with ipsilateral resisted straight leg raising.13 The pain, which may be of sudden onset or associated with a traumatic event such as a fall or twisting injury, is generally exacerbated with activity and does not respond to conservative treatment including ice, rest, nonsteroidal anti-inflammatory drugs (NSAIDs), and physical therapy. Conservative treatment may be successful for muscle strains but not for acetabular labral tears.
The impingement test was first described for patients with femoroacetabular impingement, but is equally useful for labral injuries. With the hip at 90 degrees of flexion, maximum internal rotation and adduction is performed. Contact between the anterosuperior acetabular rim and femoral neck elicits pain (Fig. 3-1). The hip can also be tested at varying degrees of flexion. Posterior labral tears can be tested with the leg externally rotated and in hyperextension.
DIAGNOSTIC IMAGING
Multiple studies have demonstrated the superior accuracy of magnetic resonance arthrography (MRA) over standard magnetic resonance imaging (MRI) for diagnosing labral tears. Intra-articular gadolinium has been shown to improve the sensitivity of diagnosing labral pathology from 25% to 92% using a small field of view.14 Therefore, when clinical suspicion of a hip labral tear exists, MRA using a small field of view is the study of choice.
An intra-articular bupivacaine injection may be useful in situations in which the diagnosis of labral pathology is equivocal or if a tear has been diagnosed by MRA,15 but it is uncertain whether symptoms are related to this finding. Similar to its use in diagnosing external impingement of the shoulder, if patients experience relief from their symptoms following the injection, the diagnosis of pain secondary to hip intra-articular pathology is more certain. However, intra-articular pathology could still be present without pain relief from an injection.16
CLASSIFICATION
A outcome correlated classification system of labral injuries and chondral damage has been created by McCarthy and colleagues17 Stage 0, as compared with a normal acetabular labrum, is a contusion of the labrum with adjacent synovitis. Stage 1 is a discrete labral free margin tear with intact articular cartilage of the acetabulum and femoral head. Stage 2 is a labral tear with focal articular damage to the subjacent femoral head but with intact acetabular articular cartilage. Stage 3 is a labral tear with an adjacent focal acetabular articular cartilage lesion, with or without femoral head articular cartilage chondromalacia. Stage 4 constitutes an extensive acetabular labral tear with associated diffuse arthritic articular cartilage changes in the joint (Fig. 3-2). The labral injury involved the anterior half of the joint 95% of the time. All patients who had combined anterior and lateral labral injuries had associated degenerative arthritis in the joint.
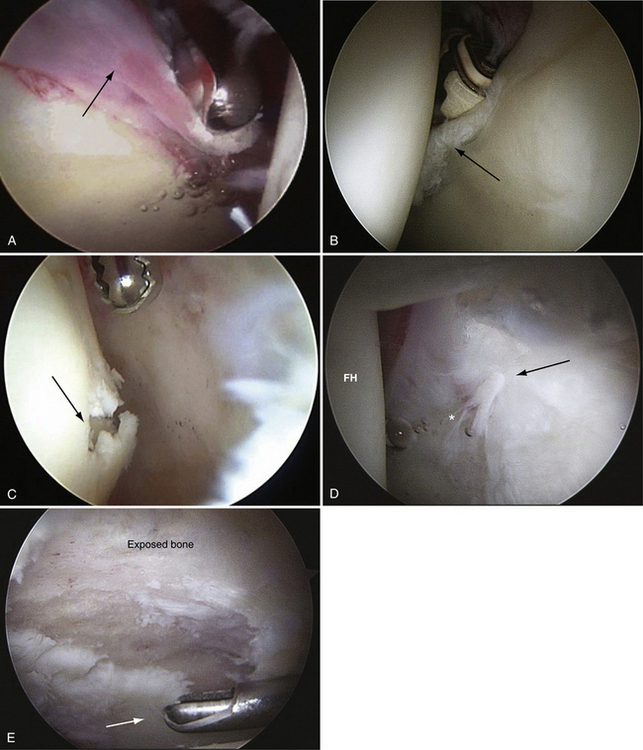
FIGURE 3-2 Classification of labral tears. A, Stage 0—labral contusion (arrow) with synovitis. B, Stage 1—labral tear (arrow) with intact articular cartilage of the acetabulum and femoral head. C, Stage 2—labral tear with focal articular damage (arrow) to the subjacent femoral head but with intact acetabular cartilage. D, Stage 3—labral tear (arrow) with an adjacent focal acetabular cartilage lesion, with or without femoral head (FH) articular cartilage damage. E, Stage 4—extensive acetabular labral tear, with associated diffuse arthritic articular cartilage changes in the joint. The arrow delineates transition to normal cartilage.










