disadvantage of requiring longer acquisition times, and the long TE T2-weighted images are technically demanding in terms of imager performance.
Table 7.1 MR Screening Examination of the Knee at 1.5 T | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
special capabilities for depicting chondral and osteochondral lesions as shown in these images, but these have not been fully explored as yet.
for isotropic resolution in three-dimensional imaging. This is imposed by the short repetition time that must be used.
60% to 80% water. Collagen makes up 50% of the weight of cartilage and proteoglycans contribute 30% to 35%.52,66
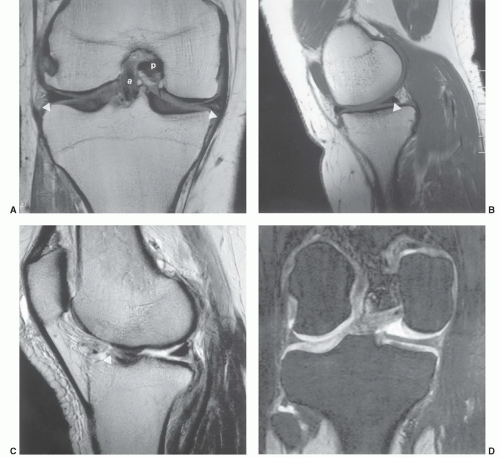
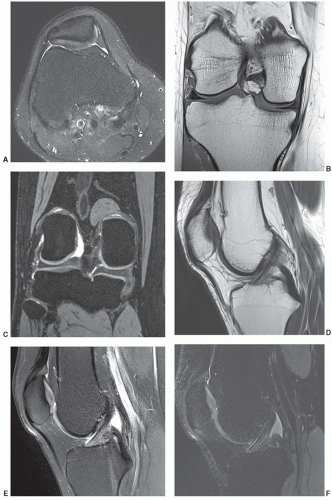
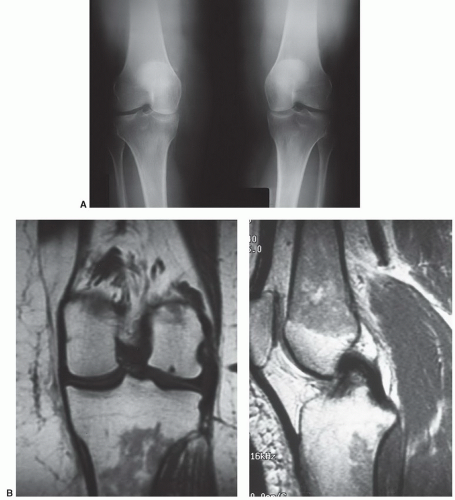
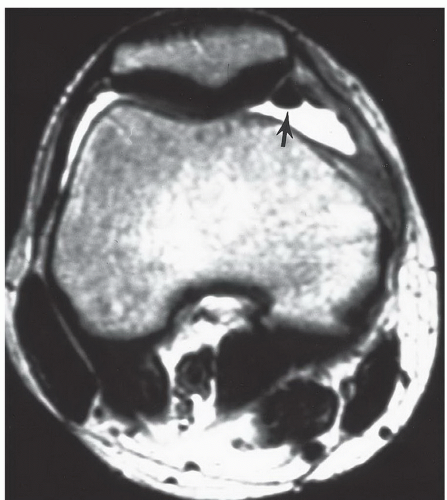
and tibial condyles (Fig. 7.20). The patella is divided into several Wiberg types. The medial and lateral facets are of equal size in type I. Type II, the most common configuration, has a smaller medial than lateral facet (Fig. 7.10). Type III has a very small medial facet that is convex and a large, concave lateral facet. Both facets are covered with hyaline cartilage and most easily seen on axial MR images (Fig. 7.10).64,70,71
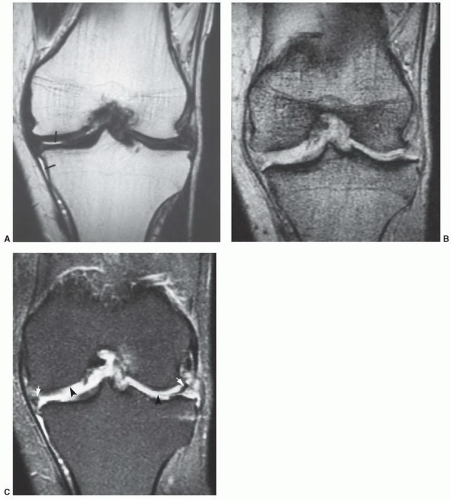
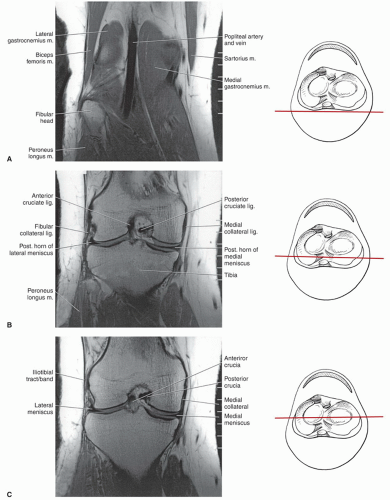
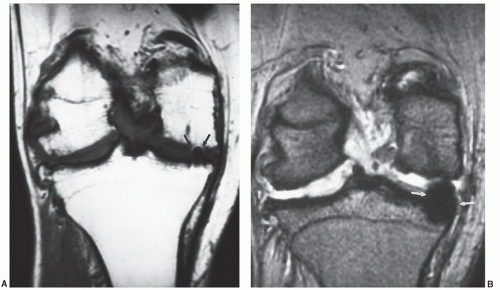
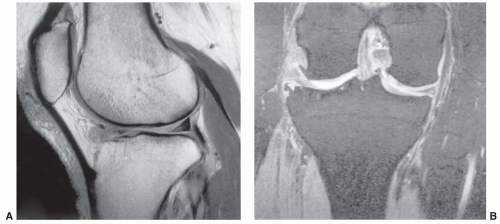
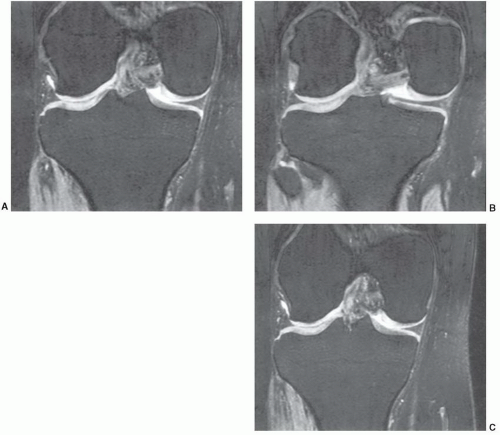 Figure 7.6 Three-dimensional gradient-echo images (A-C) of the knee from posterior to anterior demonstrating superior cartilage detail. |
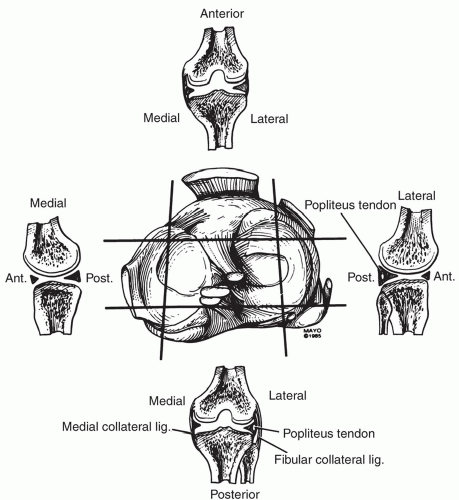
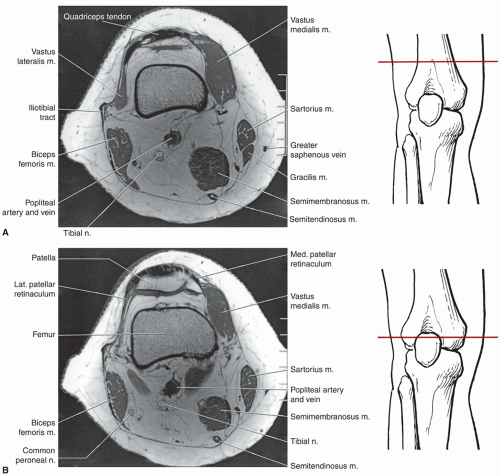
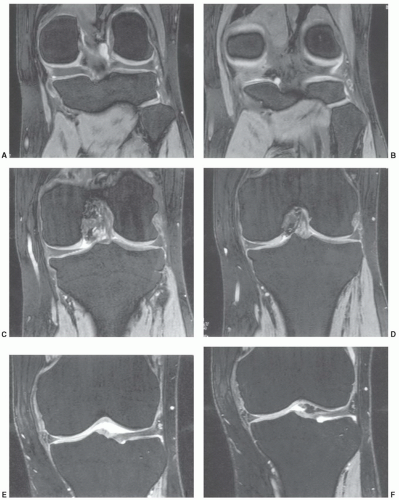
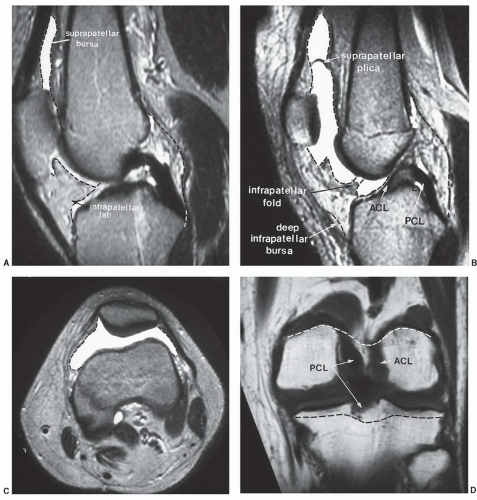
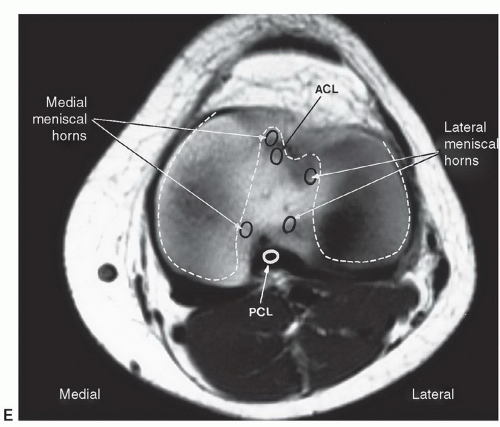
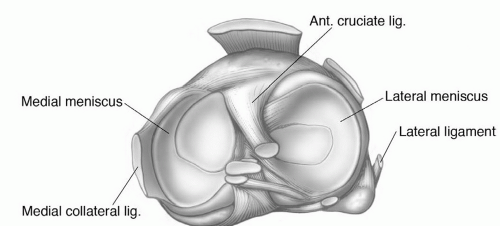
Along the medial, lateral, and posterior aspects of the capsule, the synovial membrane attaches to the femur at the edges of the articular surfaces posteriorly. Medially and laterally, it passes from the articular margins inferiorly to attach to the articular margins of the tibial condyles (Fig. 7.14D). The intrasynovial space that extends from the intracondylar fossa superiorly to the intracondylar area of the tibia inferiorly houses the cruciate ligaments. The cruciate ligaments are, therefore, covered superiorly, medially, laterally, and anteriorly by synovial membrane but not posteriorly (Fig. 7.14A, B, and E). Posterolaterally, the synovial membrane is separated from the fibrous capsule by the popliteus tendon. It is not unusual to identify a bursa along the popliteus tendon that communicates with the joint space posterolaterally. The other common bursae about the knee are listed in Table 7.2 (Fig. 7.15).19,65 There is also a lateral synovial extension that may be implicated in iliotibial band syndrome.73
Table 7.2 Bursae About the Knee | ||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||
the popliteal muscle and tendon.84 The coronary ligament, ligament of Winslow, and lateral collateral ligament are secondary restraints.65
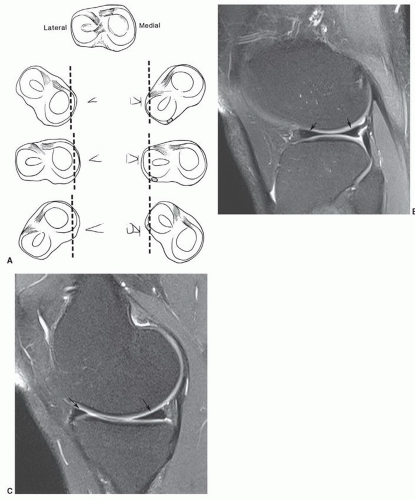
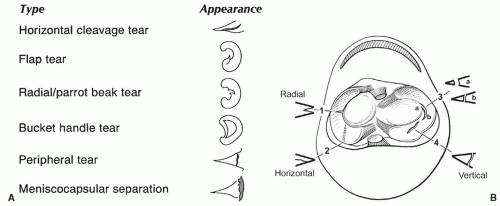
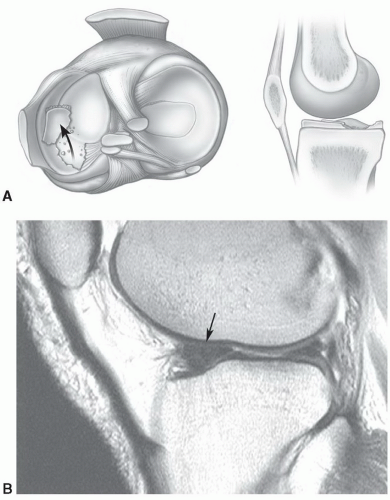
suggested that the orientation of the layers explains the origin of most meniscal tears as they appear to align with the axis of the collagen fibers.89 The fibrocartilaginous menisci have a differing shape, with the medial meniscus being larger and thicker in transverse diameter posteriorly than anteriorly (Figs. 7.11, 7.13, and 7.15A). The lateral meniscus is more C-shaped and uniform in width (Fig. 7.15A). Despite the difference in shape, the medial meniscus covers less articular surface (50%) compared with 70% coverage by the lateral meniscus.89 There are several ligamentous attachments that may cause confusion on MR images. For example, the posterior horn of the lateral meniscus is closely applied to the PCL and may give off a band of fibers, termed the meniscofemoral ligament, that follows the PCL to its attachment on the femur. Between the anterior horns of the medial and lateral meniscus there is a transverse band of fibers termed the transverse ligament of the knee. This can easily be confused with an anterior meniscal tear, especially on the medial side (Fig. 7.16).64,65 Another variant, the meniscomeniscal ligament, may also be confused with meniscal pathology. The medial meniscomeniscal ligament extends from the anterior horn of the medial meniscus to the posterior horn of the lateral meniscus. The lateral meniscomeniscal ligament extends from the anterolateral to posteromedial meniscus.90 The central attachments of both menisci are defined as the anterior and posterior root ligaments.89
posterior suprapatellar fat pad anterior to the femur (Fig. 7.16).91,92 Hoffa fat pad is bordered by the inferior pole of the patella superiorly, the patellar tendon anteriorly, the joint capsule posteriorly, and the deep infrapatellar bursa inferiorly.91 The transverse ligament can be seen in the posterior aspect of Hoffa fat pad (Fig. 7.17).91,92
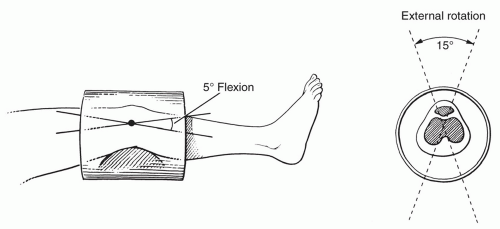
does not create as much motion artifact as when the patient is supine.2
Shellock et al.100 reported an increase in hematopoietic marrow in 43% of marathon runners, compared with only 15% of patients with knee disorders and 3% of normal healthy patients. This marrow conversion pattern may be due to “sports anemia,” which has been attributed to numerous problems such as hemolysis, hematuria, increased plasma volume, and gastrointestinal blood loss.100
Table 7.3 Knee Flexors and Extensors | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
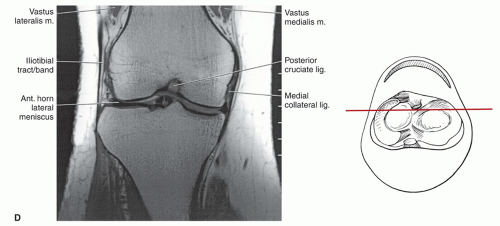
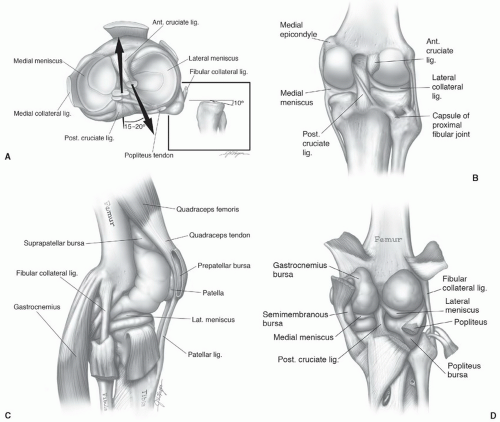 Figure 7.15 Axial (A), coronal (B), sagittal (C), and posterior (D) illustrations of the ligaments, menisci, and bursae of the knee. |
Table 7.4 Common Variants and Artifacts in MR Imaging of the Knee | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
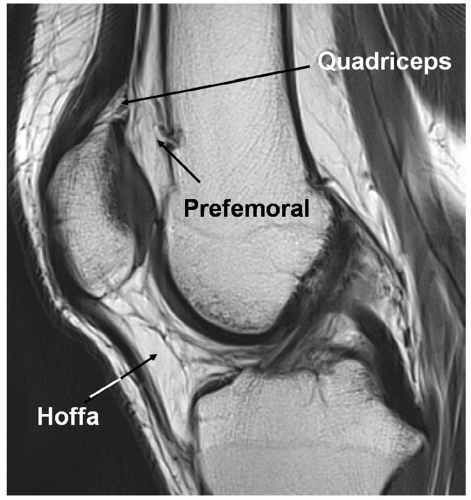 Figure 7.16 Fat pads of the anterior knee. Saggital T1-weighted 3.0-T MR image demonstrating the three anterior fat pads of the knee. |
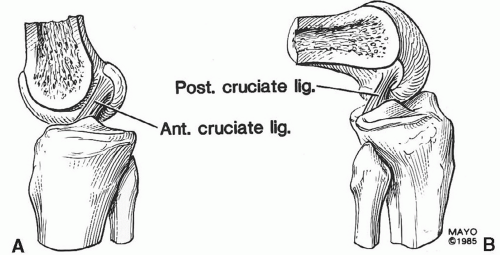 Figure 7.18 Sagittal illustrations of the knee and cruciate ligaments in the extended (A) and flexed (B) positions. |
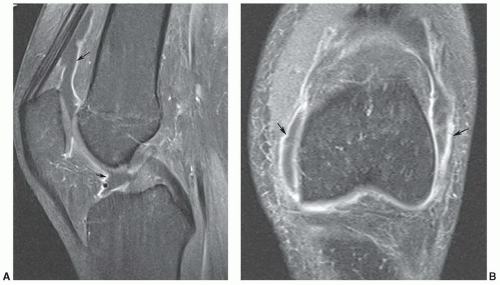
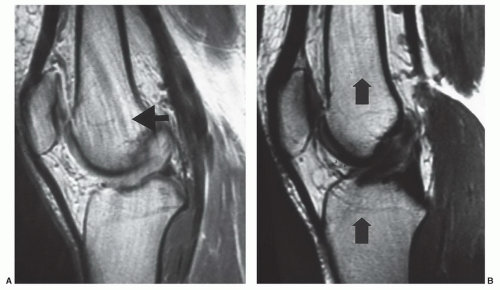
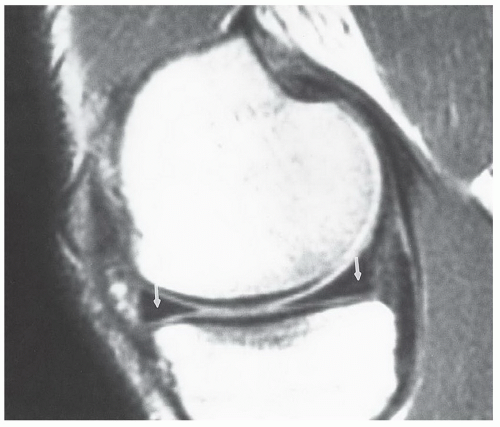
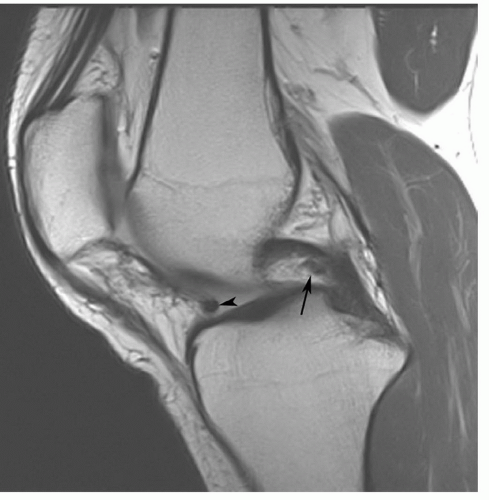
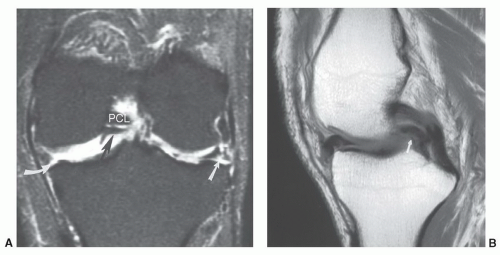
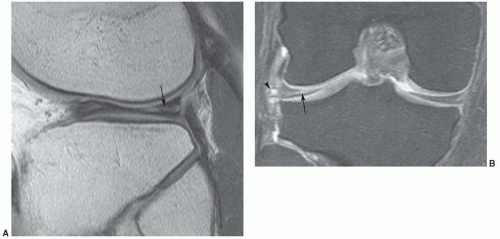
completely identified. Normal variations in the posterior ligaments can be confused with partial tears in the PCL, a meniscal tear, or osteochondral fragment.110,111,112 Themeniscal femoral ligament extends from near the posterior capsular attachment of the lateral meniscus to the medial femoral condyle and may have two branches. The most common segment is the ligament of Wrisberg that is seen just posterior to the PCL (Fig. 7.28). This is evident in 23% to 32.5% of sagittal MR images and should not be confused with a partial tear.93,96,103,104,112 The anterior bundle of this ligament or the ligament of Humphrey is seen in 34% of patients (Fig. 7.29).96,103 This lies just anterior to the PCL.
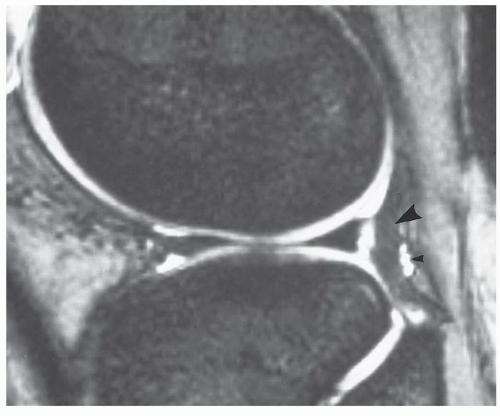
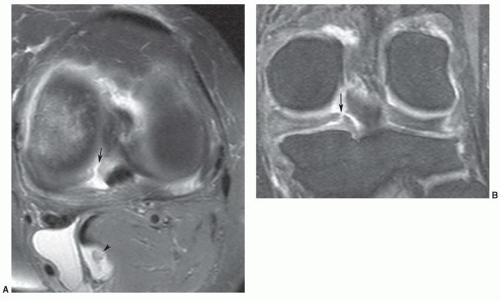
 Figure 7.23 Sagittal gradient-echo image of the posterior medial meniscus demonstrating increased signal intensity at the meniscosynovial junction (arrow), which can be confused with a tear. |
patients with trauma or suspected internal derangement of the knee.3,21,81,89,114,115,116,117,118
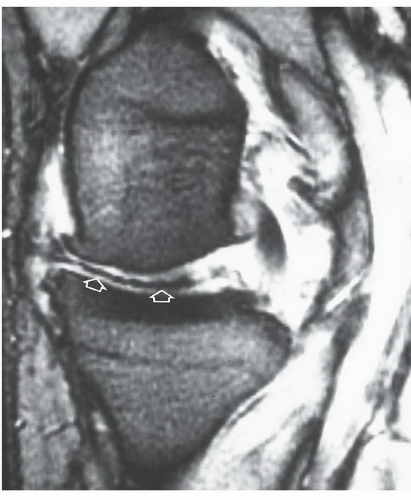 Figure 7.27 Oblique radial gradient-echo image showing an irregular low-intensity structure (open arrows) extending into the joint from the meniscal margin due to vacuum phenomenon. |
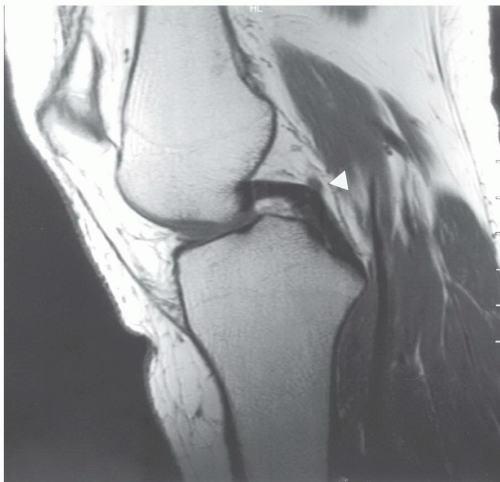 Figure 7.28 Sagittal proton density-weighted image demonstrating a normal posterior cruciate ligament. The ligament of Wrisberg (arrowhead) should not be confused with a posterior cruciate defect. |
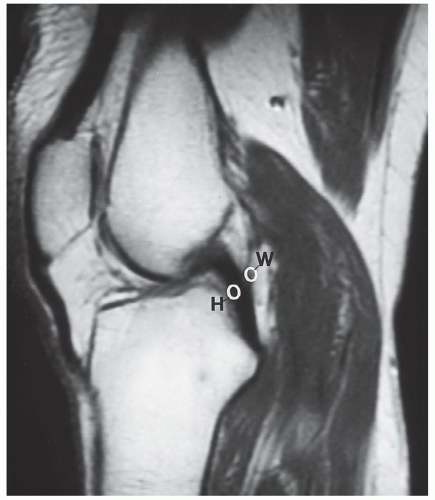 Figure 7.30 Sagittal proton density-weighted MR image demonstrating the usual locations of the meniscofemoral ligaments of Humphrey (H) and Wrisberg (W). |
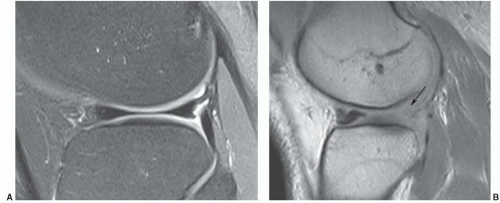
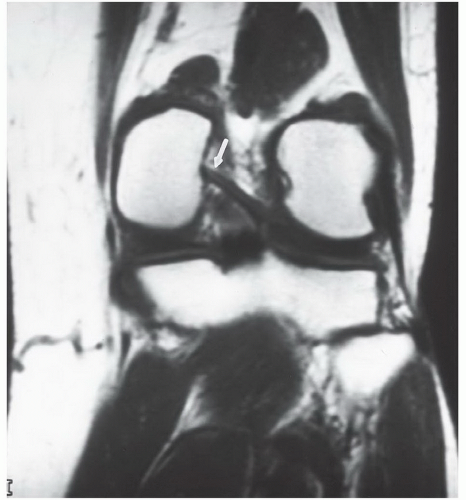 Figure 7.31 Coronal T1-weighted image demonstrating a type I meniscofemoral ligament inserting on the medial femoral condyle (arrow). |
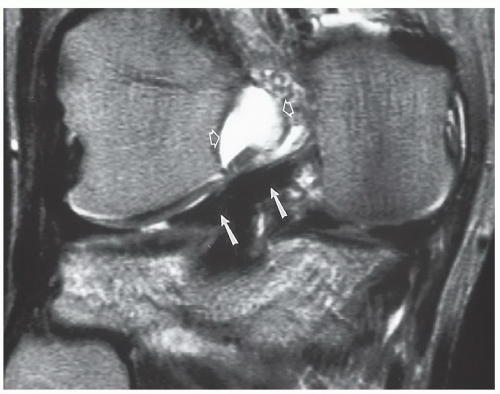 Figure 7.32 Coronal T2-weighted image demonstrating a type II meniscofemoral ligament (arrows) that is less vertically oriented than the type I in Fig. 7.31. There is high signal intensity in the notch (open arrows) due to an ACL tear. |
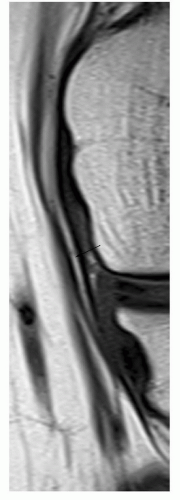 Figure 7.33 Focused coronal T1-weighted image of the medial collateral ligament demonstrating a linear fat plane (arrow) between the deep and superficial segments. |
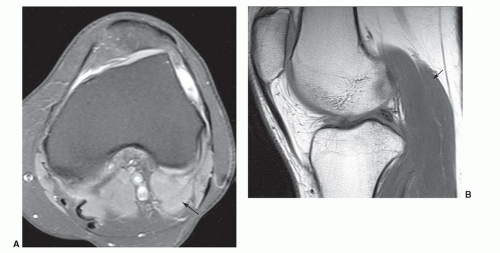 Figure 7.35 Accessory gastrocnemius. Axial fat-suppressed proton density (A) and sagittal T1-weighted (B) images demonstrating an accessory lateral head of the gastrocnemius (arrow). |
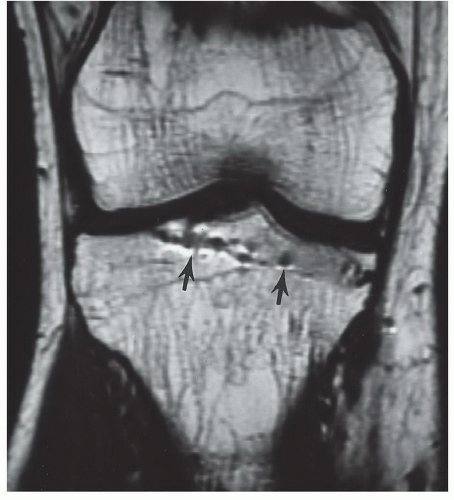 Figure 7.38 Coronal T1-weighted image, demonstrating artifacts from a previous screw tract (arrows) created by residual microscopic metal fragments. |
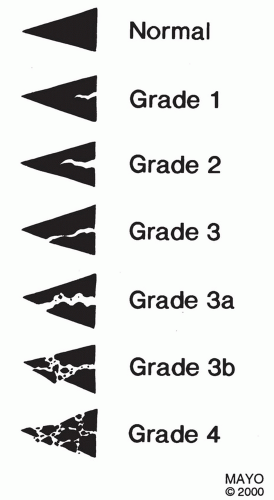
posterior to the anterior.61 Chronic repetitive trauma is common both in athletes and nonathletes with aging.75,125 Chrondrocyte necrosis and increase in mucoid ground substance can lead to meniscal tears.126
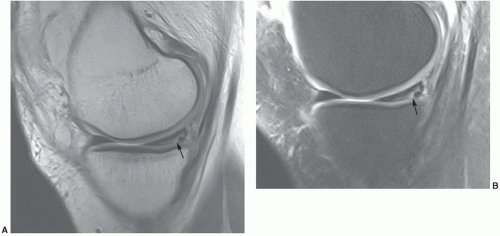
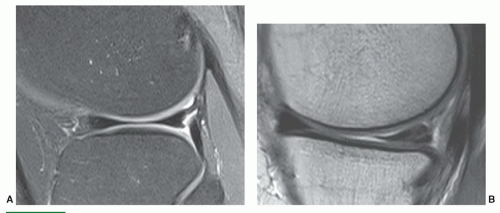
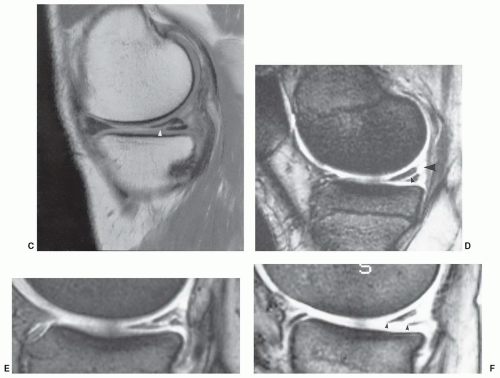
on the second echo of spin-echo sequences. Today, turbo or FSE proton density sequences are commonly used with or without fat suppression.89,129,130 The increased signal intensity seen on proton density MR images is felt to be related to hydrogen protons attached to macromolecules in the region of the tear.89 There is still some controversy regarding the accuracy of conventional spin-echo and FSE proton density sequences. Rubin et al.41 found similar sensitivities and specificities with both conventional and FSE techniques. If using FSE techniques, Rosas and De Smet89 recommend lower echo train lengths (<4) and larger bandwidths (>30 mHz) to reduce blurring. We currently obtain FSE proton density sagittal images with and without fat suppression. False negatives can be reduced using fat-suppression techniques (Fig. 7.42).129,130 Statistics for fat-suppressed proton density FSE sequences result in 92% to 95% sensitivity, 92% to 93% specificity, and 92% to 93% accuracy.130
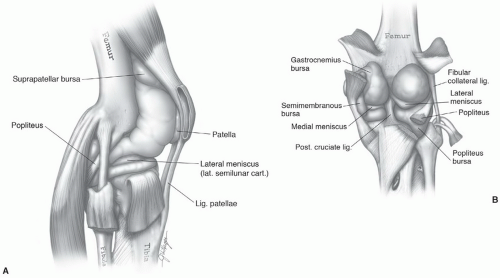 Figure 7.40 Lateral (A) and posterior (B) illustrations of the knee demonstrating the joint space and associated ligament and meniscal anatomy. |
significant signal-intensity changes that communicate with the articular surface.
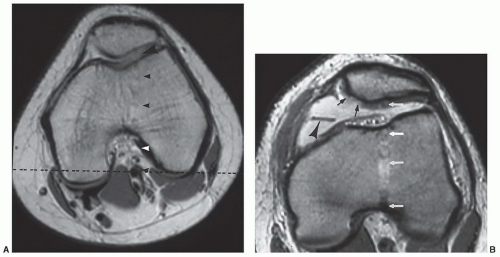
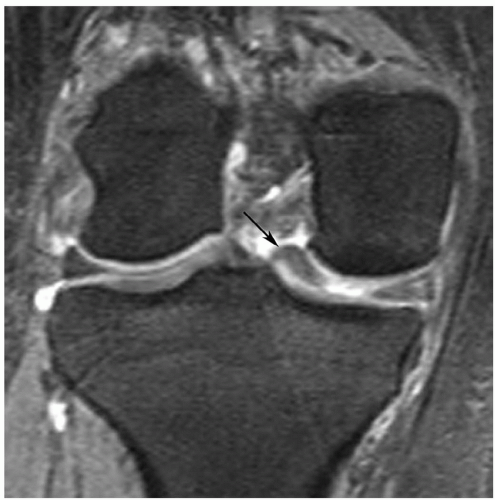
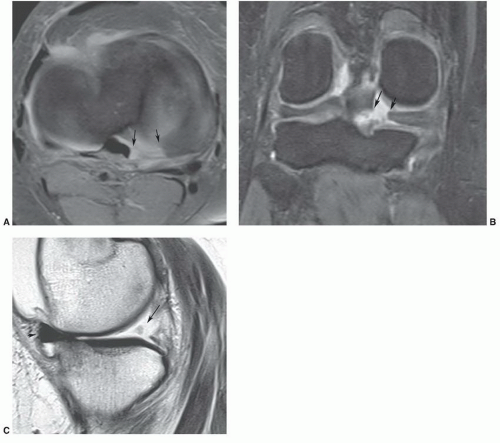
flipped-fragment sign (Fig. 7.51) is seen with 44% of medial and 29% of lateral meniscal bucket-handle tears (Table 7.5).54 Another sign is a fragment in the intercondylar notch, which is not the same as the double-PCL sign.89 Defining a fragment in the notch may be difficult, especially when they are small and the configuration of the meniscus is not significantly truncated (Fig. 7.48; Table 7.5). Larger fragments are identified with 66% of medial and 43% of lateral meniscal tears.54 Detection may be improved by using coronal STIR images. Magee and Hinson48 reported detection of 93% of fragments using STIR sequences. Defining the fragments is important, as they need to be removed arthroscopically.48 The final sign is the absent “bow-tie sign,” which is seen as absence of the normal meniscal configuration on sagittal images through the meniscus (Fig. 7.52).89
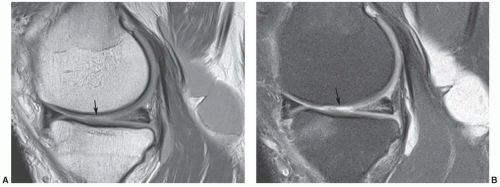 Figure 7.46 1.5-T proton density (A) and proton density with fat suppression (B) images of a complex medial meniscal tear with associated cartilage loss (arrow) and a large popliteal cyst. |
to find an associated meniscal cyst. The etiology of meniscal cysts is felt to be related to extension of joint fluid through the tear.89 Horizontal meniscal tears are more common in elderly patients with degenerative disease.89,147
Table 7.5 Bucket Handle Tears: MRI Features | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
chondrocyte nutrition. Stress to the articular cartilage is also reduced. The meniscus also restricts anterior displacement of the tibia on the femur, reducing stressonthe ACL.64,160,161
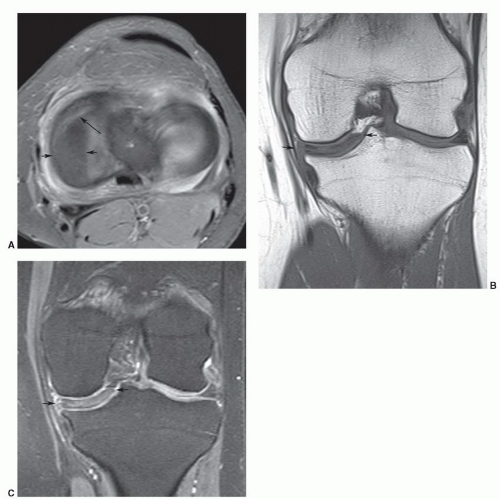
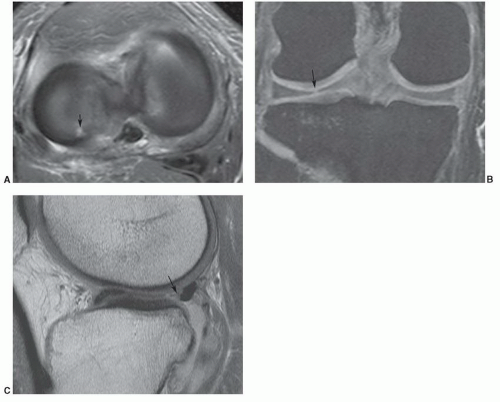
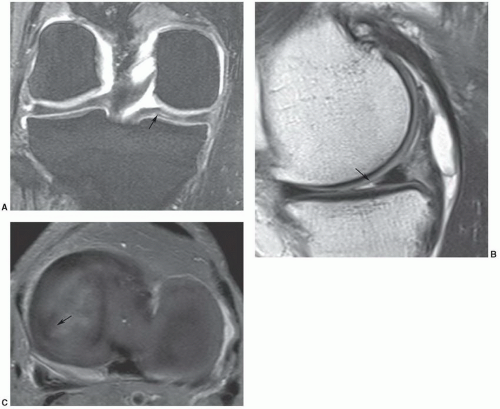 Figure 7.53 Parrot-beak tear. Coronal DESS (A), sagittal proton density (B), and axial fat-suppressed proton density (C) images demonstrate a radial tear extending peripherally (arrow). |
sequences are more useful in this setting as fluid signal intensity extending to the articular surface are more specific. Specificities have been reported as high as 90%.165 More recent studies suggest that the specificity ranges from 73% to 88% using the earlier criteria.89,162
arthrograms least accurate (58%) for evaluating menisci after surgical procedures.163 The use of arthrography remains somewhat controversial.89 In a recent study, De Smet et al.168 found that similar to the nonoperative knee, any signal intensity contacting the meniscal surface on two or more contiguous sections is most likely a new tear. This group reserves MR arthrography for patients with greater than 25% of the meniscus removed.168 We have not used MR arthrography except in selected cases or when specifically requested by the orthopedic surgeons. In our experience, MRI equivocal cases are most often reexamined arthroscopically.
Table 7.6 MRI of Meniscal Tears | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||