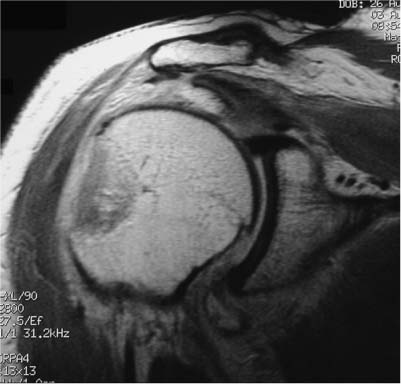
4 Isolated Tuberosity Fractures Greater tuberosity involvement has been reported in 15 to 40% of proximal humerus fractures. Isolated tuberosity fractures, however, have a significantly lower reported incidence.1–6 In a review of 930 operatively treated proximal humerus fractures at the AO Documentation Center (Davos Platz, Switzerland), fewer than 2% were isolated displaced tuberosity fractures.7 Several authors have suggested that isolated greater tuberosity fractures may be underreported due to misdiagnosis caused by commonly encountered subtle radiographic findings.1,8–12 The general consensus in the literature is that nondisplaced tuberosity fractures may be treated without operative intervention. However, treatment of displaced greater tuberosity fractures is a subject of controversy with regard to indications for operative management, surgical approach, and selection of optimal fixation to maintain an anatomic reduction. These injuries can be deceptively difficult to treat surgically as they frequently consist of suboptimal fragments for traditional internal fixation techniques and the muscle forces acting on the greater tuberosity may make obtaining and maintaining reduction more challenging than the preoperative images would suggest. Although acute anterior glenohumeral dislocations13,14 and concomitant rotator cuff tears15 are frequently associated with greater tuberosity fractures, in this chapter we will focus on the diagnosis and optimal treatment of isolated tuberosity fractures with an emphasis on the determination of surgical indications, operative techniques, and postoperative management. Isolated tuberosity fractures are most commonly caused by impaction or avulsion fractures. In the former, a direct blow from a fall or a hyperabduction injury results in impaction of the greater tuberosity against the acromion16 or superior aspect of the glenoid with the transmission of a concomitant shear force to the tuberosity. Avulsion injuries of the greater tuberosity have been described as a result of forceful contraction of the rotator cuff in patients with osteopenic bone. More frequently, fractures of the greater tuberosity resulting from a combination of impaction, avulsion, and shearing mechanisms have been reported in association with anterior glenohumeral dislocations as a component of the commonly encountered two-part fracture dislocation.8 McLaughlin6 described these patients as having sustained a “posterior mechanism anterior dislocation” and included greater tuberosity fractures, as well as large full thickness rotator cuff tears in association with this group of anterior dislocations. Greater tuberosity fractures have been reported to occur in up to 15 to 30% of anterior glenohumeral dislocations.13,14 The greater tuberosity is the insertion site of the supraspinatus, infraspinatus, and teres minor. The tendinous insertions of the articular capsule, rotator cuff muscles, the coracohumeral ligament, and glenohumeral ligament complex blend into a confluent sheet prior to insertion into the humeral tuberosities. The tendons of the supraspinatus and infraspinatus muscles join 15 mm proximal to their insertion and are not readily separable by blunt dissection. Similarly, the infraspinatus and teres minor fuse near their musculotendinous junctions. The supraspinatus and subscapularis tendons join as a sheath that surrounds the biceps tendon at the entrance of the bicipital groove.17,18 Displaced greater tuberosity fractures are pulled into a position of superior, posterior, and medial displacement by the posterior cuff muscles along the vector of their muscle forces (Fig. 4–1). Knowledge of the regional anatomy of the rotator cuff and rotator interval between the supraspinatus and subscapularis is critical for mobilizing displaced, retracted greater tuberosity fractures to obtain an anatomic reduction. The ramifications of displacement can more specifically be identified through a comprehensive knowledge of the relevant anatomical considerations. An anatomical study by Minagawa et al19 described the supraspinatus insertion to be primarily (~75%) on the anterior half of the greater tuberosity. A subsequent study by Dugas et al20 elegantly mapped the footprint (cuff insertion area) in 20 cadaveric specimens utilizing a 3-space digitizer. The mean medial-to-lateral insertion widths of the supraspinatus, infraspinatus, teres minor, and subscapularis tendons were 12.7, 13.4, 11.4, and 17.9 mm, respectively. The mean minimum medial-to-lateral insertion width of the entire rotator cuff insertion occurred at the midportion of the supraspinatus and was found to be 14.7 mm. The articular surface-to-tendon insertion distance was less than 1 mm along the anterior 2.1 cm of the supraspinatus/infraspinatus insertion. This distance progressively increased to an average distance of 13.9 mm at the inferior-most aspect of the teres minor insertion. The average anteroposterior distances of the supraspinatus, infraspinatus, teres minor, and subscapularis insertions were noted to be 1.63, 1.64, 2.07, and 2.43 cm, respectively.20 Another cadaveric study by Ruotolo et al21 examined 17 normal rotator cuffs and reported the supraspinatus tendon insertion was an average 1.7 mm from the articular margin. With regard to the osseous anatomy of the greater tuberosity, a three-dimensional analysis of the proximal humerus by Robertson et al22 reported the mean vertical distance from the superior aspect of the greater tuberosity to the superior aspect of the humeral head was 6 2 mm. Knowledge of the rotator cuff footprint dimensions and osseous anatomy is important for restoring the normal anatomical relationships when treating greater tuberosity fractures and may be of assistance when intraoperatively determining options for treatment of comminuted fracture patterns, fractures with concomitant rotator cuff tears, and fracture fragments with insufficient cortical density for stable fixation. Figure 4–1 (A) Plain film true anteroposterior (AP) radiograph demonstrating a large fragment with posteromedial displacement. (B) Plain film AP radiograph demonstrating superior displacement. (C) Plain film axillary radiograph demonstrating posterior displacement. (D) Plain film radiograph demonstrating an impacted greater tuberosity fracture. The primary blood supply to the proximal humerus is the anterior lateral branch of the anterior humeral circumflex artery.23,24 The anterior humeral circumflex artery is derived from the third division of the axillary artery approximately 1 cm distal to the inferior border of the pectoralis minor. It then travels laterally posterior to the coracobrachialis and approaches the surgical neck of the humerus at the lower border of the subscapularis. The anterolateral branch of the anterior humeral circumflex artery travels superiorly in the lateral aspect of the intertubercular groove to penetrate bone as it approaches the greater tuberosity and this branch then becomes the arcuate artery. Multiple extraosseous anastomoses exist between the anterior humeral circumflex artery, the posterior humeral circumflex artery, the thoracoacromial artery, suprascapular artery, subscapular artery, and profunda brachii artery.23 By selecting the most appropriate operative approach (see below), minimizing excessive dissection, and with a thorough knowledge of the regional vascular anatomy, the risks of nonunion, delayed union, and avascular necrosis may be minimized. The rationale for more aggressive operative intervention in the treatment of displaced tuberosity fractures is predicated on concern for malunion resulting in symptomatic subacromial impingement, functional loss from decreased shoulder abduction, and an alteration in rotator cuff function due to a shortening of the lever arms for forward elevation and external rotation.8,25–27 Hence, a rigorous approach to assessing the patient with an isolated tuberosity fracture is critical. After a thorough history and physical examination documenting the neurovascular status of the involved extremity, the initial plain radiographic evaluation consists of anteroposterior (AP), true AP, axillary, and scapular-Y or acromial outlet views. Plain radiographs may underestimate both the degree of displacement and extent of comminution. In addition, accurate assessment may be impaired by a small size fragment, comminution, or superimposition of the fragment on the humeral head.1,11,28 A study by Parsons et al1 was the first to examine the accuracy and reliability of image interpretation for known displacements of the greater tuberosity. In this cadaveric study, the authors reported that no one fluoroscopic view was significantly more accurate than any other and they noted a trend toward increased accuracy for imaging minimally displaced fragments (5 mm or less displacement) with the AP view in external rotation. Figure 4–2 Three-dimensional computed tomography reconstruction image of a greater tuberosity fracture with superior displacement. When a sufficient index of suspicion exists despite normal-appearing radiographs, consideration of further diagnostic imaging is appropriate. Computed tomography (CT) may be of assistance for its ability to accurately detail the osseous anatomy about the proximal humerus; however, its ability to adequately image the pertinent rotator cuff anatomy is limited (Fig. 4–2).28 As a result, magnetic resonance imaging (MRI) is more commonly employed and is a more practical modality (Fig. 4–3).9,26,29 Although rarely used to evaluate for a possible greater tuberosity fracture, ultrasound has been reported as a method to diagnose occult nondisplaced greater tuberosity fractures.30 Figure 4–3 Magnetic resonance image of an impacted nondisplaced greater tuberosity fracture. Classically, Neer31 defined one centimeter as a threshold for displacement requiring operative treatment of proximal humerus fractures. Subsequently, Young and Wallace32 reported good or acceptable results in 97% of cases with conservative treatment for minimally displaced greater tuberosity fractures. However, the authors of this study defined acceptable as abduction 60 degrees, a definition with which many contemporary orthopedic surgeons would not concur. In a case series of 79 pooled displaced and nondisplaced greater tuberosity fractures, Olivier et al33 reported unsatisfactory results in 31%. Extrapolation of the historical literature on conservative treatment of greater tuberosity fractures is difficult due to small sample sizes, pooling of displaced and nondisplaced fractures, and nonstandardized, nonvalidated outcome measures. As described above, several investigators have advocated operative intervention for the treatment of displaced greater tuberosity fractures as malunion often results in symptomatic subacromial impingement, functional loss from decreased shoulder abduction, an alteration in rotator cuff function due to a shortening of the lever arms for forward elevation and external rotation, and the potential for capsular contracture restricting internal rotation and horizontal adduction.8,25,26 As with any fracture or injury about the shoulder, tailoring operative indications to the patient’s functional status, activity level, history of shoulder pain and function, and concomitant injuries is imperative. Nevertheless, the recent literature regarding operative indications for greater tuberosity fractures endorses the consideration of operative management of fractures displaced more than 5 mm superiorly or more than 0.5 to 1 cm posteriorly based on the concerns mentioned above.11,26,34,35 Recent basic science studies have provided biomechanical data to further support these recommendations. A study by Bono et al26 employed a dynamic, cadaver-based biomechanical shoulder simulator to model greater tuberosity malunion and determine the change in deltoid force required for abduction with varying amounts of displacement. The authors demonstrated a statistically significant increase in abduction force for superior displacements of 0.5 cm (16%, p = 0.006) and 1 cm (27%, p = 0.0001). Combined together, posterior and superior displacements of 1 cm resulted in a 29% force increase (p = 0.001). Although there are limitations in any study employing a cadaveric biomechanical simulator, the biologic plausibility and statistical significance of the data reported support the clinical concerns of tuberosity displacement impeding normal glenohumeral kinematics through alteration of normal rotator cuff function. As described above, nonoperative management is typically selected for patients with less than 5 mm of superior displacement or 0.5 to 1 cm of posterior displacement. The approach is similar to that of any periarticular fracture with a balance struck between immobilization to allow fracture healing and motion to prevent contracture, muscular atrophy, and disability. Most greater tuberosity fractures associated with glenohumeral dislocation are minimally displaced or nondisplaced after reduction of the glenohumeral joint and may be treated nonoperatively. In a study of glenohumeral fracture-dislocations, McLaughlin6 reported that after closed reduction, the greater tuberosity was reduced in 24 of 34 cases (71%). As stated above, close follow-up is indicated for this patient population to prevent the treating physician from overlooking a concomitant acute, traumatic rotator cuff tear that would benefit from early operative intervention.36 Patients should be advised and reassured that glenohumeral dislocations associated with greater tuberosity fracture have been reported to have a low risk of recurrent dislocation.13,14 Duration of immobilization is surgeon- and patient-dependent; however, general recommendations in the literature include shoulder immobilization for 2 weeks after confirmed anatomic reduction of the glenohumeral joint followed by initiation of passive motion to limit capsular contracture and subacromial adhesions. After approximately 6 weeks, and with radiographic confirmation of no additional displacement, active range-of-motion exercises are initiated followed by rotator cuff and periscapular muscle strengthening exercises once full passive shoulder motion is achieved.8
Etiology and Mechanism of Injury
Anatomy
Patient Assessment
Treatment
Indications for Surgery
Nonsurgical Treatment
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree