38 Introduction to Physical Medicine, Physical Therapy, and Rehabilitation
Modern rehabilitation is interdisciplinary using a patient-centered approach.
The main focus in the assessment and treatment of patients is on function.
Exercise is consistently effective in the treatment of various rheumatic diseases.
Physical modalities may be used as an adjunct to active therapies.
Rehabilitation is a specialized medical field that combines medical therapy and nonpharmacologic interventions with the goals of maximizing function and independence and ameliorating symptoms. The rehabilitation community has embraced the International Classification of Functioning, Disability, and Health (ICF)1 as a framework for developing interventions to address the consequences of disease, communicating about strategies that enable individuals to engage fully in society, and formulating research in rehabilitation medicine.2–7
Rehabilitation interventions are multimodal and diverse and are designed to help individuals with arthritis live with their disease.8–15 Exercise is the most studied and best proven intervention.15–17 Physical modalities such as ultrasound and heat are adjuncts to exercise and show modest benefits with respect to pain relief, extensibility of tissue, and relaxation.8–10,13–15 Orthotics, ambulatory devices, splints, and adaptive devices enable patients to navigate barriers that persist despite other interventions.18–20
Brief History of Rehabilitation in Arthritis
Early arthritis rehabilitation focused on bed rest, splinting, and gentle range-of-motion exercises. Physicians and rehabilitation specialists believed that physical activity and strenuous exercise would produce pain, increase joint swelling and temperature, and accelerate joint damage. In the 1940s, with the introduction of steroids, highly efficient and potent anti-inflammatory drugs, the rehabilitation focus shifted toward splinting and mobilizing patients with assistive devices to promote function. Surgical approaches such as joint replacements were used in the 1960s and 1970s to “stop” the progression of disease. At this time, rehabilitation interventions focused on postoperative protocols to enable patients to regain function and maximize independence. Through the 1970s and 1980s, with the proliferation of disease-remitting agents such as myochrysine, methotrexate, and sulfasalazine, rehabilitation regimens began to incorporate dynamic exercises and functional activities earlier in the disease process. Rehabilitation researchers also began to evaluate the impact of isometric and low-intensity isotonic exercise on immune response and function. Early data from these trials suggested positive effects on disease activity and strength.21,22 As more medications entered the market and the prevalence of disease-modifying antirheumatic drugs (DMARDs) in clinical practice expanded, rehabilitation research focused on evaluation of the effects of various intensities, frequencies, and modes of strengthening exercises on patient outcomes. From the mid-1990s onward, studies of aerobic exercise illuminated the benefits of aerobic conditioning for cardiovascular function without deleterious effects on joints and soft tissue.23–25 In the 21st century, with the development of advanced radiologic techniques and the advent of biologic therapies, researchers are investigating the impact of weight-bearing activities on joint integrity in people with arthritis26 and are embracing a public health perspective through promotion of community physical activity programs designed to improve quality of life and function.27,28
Goals of Rehabilitation, Rehabilitation Team Members, and Models of Team Care
Rehabilitation interventions address all aspects of the patient’s condition with the aim of maximizing function and independence. As such, interventions range from prescription of adaptive devices, such as splints, orthotics, and ambulatory devices, to use of physical modalities, such as ultrasound, heat, and cold, to instruction in exercise and self-management strategies (relaxation, proper rest). Rehabilitation specialists are educated to assess environmental factors so they can best address barriers and facilitators impacting their patients.29
The initial phase of the rehabilitation process involves a comprehensive assessment of all dimensions of the patient’s life and condition. Given the fluctuating course of many arthritides, a coordinated effort by a variety of skilled multiprofessional rehabilitation specialists is required. The structure, function, and resources of the medical system in which the patient resides influence the composition of the team.30,31 Physiatrists, or rehabilitation medicine physicians, are educated in medicine and rehabilitation to treat patients and refer to, and/or supervise, other skilled rehabilitation professionals.29 These physicians typically are responsible for the care of arthritis patients. However, in some circumstances, the rheumatologist may be the only physician involved in the patient’s care. Other rehabilitation professionals involved in the care of these patients are primary care physicians, nurse practitioners, nurses, physical therapists, occupational therapists, social workers, nutritionists, psychologists, podiatrists, and vocational rehabilitators, who work with the patient’s family.
Comparative studies of team care delivery versus individual practitioner models indicate that coordinated team efforts yield better outcomes.32–34 In all cases, the patient is the focal point of the team. Traditional models of team care are categorized as interdisciplinary, multidisciplinary, or transdisciplinary. In the interdisciplinary model, each professional conducts an independent patient evaluation and shares this information during team meetings to facilitate the development of integrated team goals. Negotiation and collaboration are prevalent principles. Multidisciplinary team care does not foster intercommunication between professionals in a coordinated manner.35 Rather, each professional conducts an examination and develops his/her goals for care in concert with the patient, and separately documents findings. The transdisciplinary model allows for the transference of professional roles. This model crosses professional boundaries (e.g., a physical therapist can do some functions of a nurse).36–38 Any of these models of care may occur in an inpatient or outpatient setting.
Although team care has been widely used in Europe, this is not the case in North America, in part because of budgetary constraints and shortages of health care professionals, especially in rural areas.39 Consequently, innovative care models such as the clinical nurse-specialist model,36,38 the primary therapist model,37 and telemedicine have emerged.
International Classification of Functioning, Disability, and Health: A Framework for Rehabilitation Management
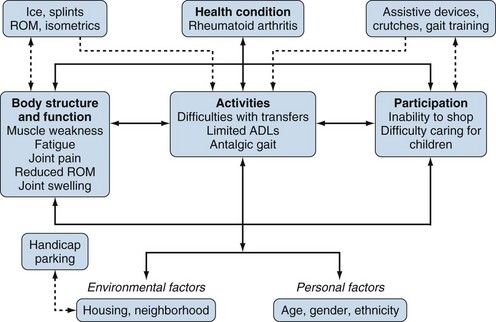
The International Classification of Functioning, Disability, and Health (ICF) of the World Health Organization provides a framework for the development and implementation of rehabilitation interventions.1 The ICF systematically organizes various aspects of an individual’s health condition. The term functioning is used to describe body functions, activities, and participation; the term disability refers to impairments, activity limitations, and participation restrictions. The ICF also considers environmental and personal factors that interact with body functions, body structures, activities, and participation.1 This framework integrates aspects of the biopsychosocial medical model with an ecological perspective. The equal emphasis on ecological factors, such as personal and environmental contextual factors, helps rehabilitation specialists identify and address elements that may facilitate or present barriers to obtaining independence. The ICF definitions serve as a common language for providers to communicate about patients’ health conditions, interventions, and performance of activities and participation in society1–8 (Figure 38-1). Researchers use the ICF to solidify and examine core constructs relevant to clinical studies of arthritis rehabilitation.3,6,7 These core sets have been compared with well-validated clinical outcome measures and help to identify the most salient outcome measures for use in rehabilitation clinical trials.3,39
Assessment Tools and the REHABILITATION Cycle
• Technical measures: electrophysiologic, biomechanical, and computerized devices
• Clinical tests: ligament laxity tests, range-of-motion and strength testing
• Performance measures: gait velocity, mobility tests
• Patient-centered measures: patient and proxy self-reports on health status, quality of life, and health preferences
Because the primary goal in rehabilitation is to restore function and enable a return to normal life, the emphasis of a rehabilitation examination is on assessment of functioning and societal participation.35
Body structures and function elements such as joint motion may be assessed subjectively through simple observation, goniometry, or high-speed cinematography. Goniometry is most commonly used in the clinical setting because it is inexpensive, is easy to perform, and is psychometrically sound. Muscle strength is frequently assessed using manual muscle testing procedures, although its reliability and validity varies by joint location and by disease. Quantitative methods of maximal isometric strength measurement with hand-held dynamometers are reliable in patients with inflammatory arthritis35,40,41 and in those with degenerative lumbar spinal stenosis.42 Hand-grip strength can be measured reliably with a hydraulic hand dynamometer.43
Gait velocity, calculated as the time needed to walk a specific distance, is commonly measured to assess walking mobility44 and serves as a test of lower extremity function. The “Timed Up and Go” test45 is a basic mobility test that measures the time it takes a patient to rise from an arm chair (seat height of 46 cm and arm height of 65 cm), walk 3 meters, and return to and sit down in the chair. This performance measure has been tested in a variety of patients and has been used to establish normative values for different age groups.
Patient self-report measures developed and tested over the past two to three decades are widely implemented in the core-set measures for various rheumatic conditions. In inflammatory arthritis, the Health Assessment Questionnaire (HAQ) assesses dimensions of health, including disability, pain, medication effects, and costs of care.46 A modified version of the HAQ, known as the MHAQ, uses fewer items and maintains good psychometric properties, although differences in scores for disability are evident between the HAQ and the MHAQ.47 A disease-specific version of the HAQ is available for persons with rheumatoid arthritis (RA-HAQ). The Katz Index of activities of daily living and the MacMaster Toronto Arthritis Preference Disability Questionnaire (MACTAR) also measure general activities of daily living. The MACTAR is unique in that it allows patients to choose which activities are important to them.35
A range of patient-oriented, disease-specific measures of function and symptoms may be used to assess pain, psychological status, well-being, fatigue, sleep, and quality of life.12 Thus it may be difficult for clinicians and researchers to select the most appropriate measure for their purpose. To address this problem, one can refer to the ICF framework of functioning, which provides a clear picture of which health domains are addressed by each of the measures. Linking rules have been established to relate technical and clinical measures, health status measures, and interventions to the ICF.4
What Do Current Guidelines for Rehabilitation Management of Select Arthritides Suggest?
Clinical guidelines for arthritis management consistently promote the use of exercise, physical activity, and physical therapy.48–59 Recommendations are based on substantial evidence from randomized controlled trials of exercise in arthritis60–65 indicating moderate effect sizes for the benefits of exercise for pain relief, function, and muscle strength. However, specific exercise prescriptions are not provided. Lack of details regarding exercise prescription originates from inconsistency in information regarding the intensity, frequency, mode, and duration of exercise in early clinical trials of exercise.65 More recent studies adhere to standardized reporting criteria such as the GRADE (Grading of Recommendations Assessment, Development, and Evaluation) framework,66 thus providing detailed information about exercise interventions to enable better synthesis of data. Information regarding accepted clinical rehabilitation is provided in the section addressing specific diagnoses and interventions.
Nonpharmacologic Interventions to Manage Arthritis
Nonpharmacologic interventions used to manage arthritis symptoms include rest (total body or local), massage and trigger point techniques, exercise, assistive devices, orthotics and splints, counseling, education and self-management, manual therapy/mobilization, gait training and instruction in ambulatory devices, mobility devices, ergonomic modifications, and vocational rehabilitation. Table 38-167–76 provides a description of each of these interventions and their role in the management of arthritis. Among these, exercise, patient education programs, and self-management interventions are the best studied and the most effective. Across diseases, exercise interventions, whether dynamic or static, yield moderate improvements (effect sizes of 4 to 6) in strength, pain, and function, and produce small to moderate improvements in mood, quality of sleep, sleep patterns, and psychological well-being.16,17,63–65,77–81 Exercise also reduces inflammation.82–84
Table 38-1 Definitions, Descriptions, and Purposes of Common Rehabilitation: Interventions to Manage Symptoms of Arthritis
| Intervention | Description |
|---|---|
| Energy conservation/total body rest | Important with inflammatory rheumatic diseases to have intermittent rests during the day (half hour) and 8-10 hours of rest per night87 |
| Local rest/resting splints | Resting splints (worn at night or during periods of total body rest to prevent joint movement) provide local rest to joints and maintain joint alignment. In RA and other systemic inflammatory disorders, resting wrist splints are well tolerated and effective.14 |
| Manual therapy/joint mobilization/manipulation | Performed as low- or high-velocity, small- or large-amplitude passive movement techniques. Flexibility and strengthening exercises follow manual therapy/mobilization to gain full benefit. Evidence is strongest in treating hip and low back disorders, but effects are small.67 |
| Trigger point therapy | Used for muscle pain. Consists of ischemic compression of trigger points, followed by isotonic contractions or muscle tissue stretching. Additional techniques include myofascial release, trigger point injections, trigger point dry needling, and intramuscular manual therapy. A local twitch response, provocation of referred pain, and subsequent relaxation of the taut band indicate successful application.35 |
| Massage | Increases local blood and lymph flow, facilitates muscle relaxation, and reduces muscle stiffness, pain, and spasm. Techniques include gliding, kneading, deep friction, and percussion. Gliding and kneading reduce muscle tension, improve circulation, and decrease edema. Friction breaks up adhesions. Lymph drainage increases lymph flow and decreases edema.68 Massage is contraindicated over malignant tumors, open wounds, thrombophlebitis, and infected tissues. Lymph drainage should be avoided in patients with congestive heart failure.35,69 |
| Exercise | |
| Range-of-motion (ROM) and flexibility exercises | Maintain joint movement and function and may be performed passively (by therapist) or may require active patient participation. In active-assisted exercises, the patient exerts some force with joint movement but is assisted by the therapist. Active ROM exercises require the patient to exert muscle effort to achieve the desired ROM.35,87 Flexibility or stretching exercises enhance extensibility of muscle tissue. Stretching is best performed using gentle, smooth movement, and then holding the stretch for 2-15 seconds. |
| Isometric (static) exercise | Muscle contraction performed without a change in joint range or muscle length. These exercises produce less strain on joints than is produced by dynamic exercise.87 |
| Isotonic/dynamic/isokinetic exercise | Isotonic exercises require changes in muscle fiber length by elongating (eccentric) or shortening (concentric). These exercises involve movement through a fixed ROM at a fixed rate (velocity) against variable resistance. A machine provides resistance and rate of movement that matches exactly the force generated by the patient at any point in the range. This equipment can calculate the torque developed during the exercise activity.35,82 Note: AVOID in the presence of inflammation, popliteal cysts, and joint derangement.87 |
| Aerobic conditioning or endurance exercise | Provides cardiovascular pulmonary benefits, improves muscle strength, and reduces inflammation and weight. Modest effect sizes for these outcomes are achieved when exercises are performed at moderate levels of intensity for extended periods. Modes of aerobic exercise include walking, running, hiking, cycling, swimming, and stair climbing.23–2579 |
| Aquatic exercise, spa therapy, balneotherapy | Based on physical properties of water (i.e., buoyancy, molecule adhesion, temperature), provide physiologic benefits such as muscle relaxation and ease of movement. Exercises performed in water allow buoyancy to support body weight and unload joints. Water adhesion properties may provide resistance when exercising. Diuresis and hemodilution are physiologic effects experienced with aquatic exercise. The recommended water temperature is 33° C–34° C (92° F–94° F). A systematic review of randomized controlled trials investigating balneotherapy has reported positive findings. However, the evidence was insufficient to allow formal conclusions about the efficacy of balneotherapy for patients with arthritis.10 |
| Physical Modalities | |
| Superficial heat/cold therapy | Radiation (infrared light) and conduction (hot packs, paraffin, or water) are mechanisms for superficial heat/cold generation that are applied for 20 minutes. Superficial heat increases the pain threshold, decreases muscle spasms, and produces analgesia by acting on free nerve endings. Note: AVOID heat therapy in the presence of acute inflammation or in persons with altered sensation. Cold therapy may be applied using ice packs, ice massage, vapocoolant sprays, or cold water baths. Cold therapy induces superficial and intra-articular tissue vasoconstriction, reduces local metabolism, and slows nerve conduction, thereby reducing pain and inflammation. Complications of cryotherapy include frostbite, cold-induced urticaria, and nerve damage. Use cryotherapy with caution in patients with Raynaud’s phenomenon or with cryoglobulinemia.35 Although evidence for physiologic benefits of heat and cold therapy indicates small effects,9 patients report psychological benefits. |
| Electrotherapy | Uses electricity to stimulate nerves and muscles and to alleviate pain. Surface electrodes are the common transfer medium. Only electro-acupuncture and dorsal horn stimulation use needle electrodes percutaneously. Electrotherapy uses direct continuous galvanic currents and modulated direct currents. Galvanic currents decrease pain conduction in slow unmyelinated nerve fibers (C fibers) to reduce pain. Modulated middle-frequency electrotherapy results in inhibition of pain-related potentials at spinal and supraspinal levels. Electrical stimulation of fast-conducting myelinated nerve fibers can partially decrease pain through inhibition of pain impulses carried more slowly by unmyelinated fibers. Faster impulses arrive at the level of the dorsal horn first and “close the gate.” Transcutaneous electrical nerve stimulation (TENS) is used for musculoskeletal pain, posttraumatic or postsurgical pain, peripheral nerve injury, neuropathic pain, and sympathetically mediated pain.35 Electrotherapy is contraindicated in patients with cardiac pacemakers or implanted cardiac defibrillators, and is used with caution in patients with atrophic skin.35 A systematic review of randomized controlled trials of TENS in arthritis reports inconsistent results in managing RA symptoms13 and low back pain, and some benefits for pain and knee stiffness in patients with knee osteoarthritis.70 |
| Deep tissue heating/ ultrasound and diathermy | Parameters for application vary by the device; the device must be applied by a skilled provider owing to the risk of deep tissue burns of the skin, fat, muscles, and bones. Heating occurs mostly at tissue interfaces (e.g., bone–soft tissue interfaces). Ultrasound may penetrate 7-8 cm of fat, but less than 1 mm of bone, depending on the energy level and frequency chosen. In practice, ultrasound with frequencies of 0.1-1 MHz can increase temperature by 4° C–5° C at depths of 7-8 cm.35 Two systematic reviews of ultrasound8,71 reported small benefits for pain, knee and hand stiffness, grip strength, and tender and swollen hand joints.8 Note: Avoid deep heating in patients with altered sensation, implants, or history of cancer. Ultrasound must be applied using continuous movement over joints and bony surfaces or in a water bath to avoid heating of bone. |
| Devices to Stabilize and Protect Joints | |
| Orthotics/braces | Orthotic devices include braces, splints, corsets, collars, and shoe modifications. Orthotic devices restore or maximize function by altering biomechanics through stabilizing, realigning, and/or maximizing joint position, thereby reducing pain. Orthotics provide some pain relief but inconclusive evidence of improved function long term.18,19 Successful prescription and use of orthotics require the identification of functional limitations (on all ICF levels) and patient collaboration to adjust the orthotic. Devices can be simple and inexpensive, but may be specially designed and consequently expensive.35 Bracing is prescribed to stabilize joints. The most common are knee braces typically prescribed for OA.19 |
| Dynamic splints | Dynamic splints maintain joint alignment and reduce pain during functional activities. The most common dynamic splints used in RA are functional wrist splints, although many others are available for the small hand joints. In OA, thumb splints are common. A Cochrane review from 2003 concluded that dynamic wrist splints significantly increase grip strength but do not impact pain, morning stiffness, pinch grip, or quality of life. No evidence suggests that resting splints changed pain, grip strength, or the number of painful or swollen joints. Patients preferred using these splints to nonuse.20,35 |
| Collars/corsets | Cervical collars include soft collars, Philadelphia collar, and sterno-occipitomandibular plaster immobilization. These provide varying levels of stability. None prevent subluxation or displacement.72 Patients with night pain resulting from a cervical disk syndrome may profit from wearing a soft collar at night. Corsets and abdominal binders provide feedback but limited stability to patients in terms of body position.35 |
| Assistive devices | A multitude of devices may be used to assist function and reduce barriers to independence. Examples include button hooks, long-handled reachers, sock aids, modified eating utensils (padded handles), bottle openers, and modified container lids. A physical or occupational therapist may recommend modified door handles, a raised toilet seat, a commode, safety bars on the bathroom wall, or a lift in the bath to ensure safety and maximize independence with hygiene activities. |
| Mobility devices | Mobility devices, such as canes, crutches (axillary, forearm, and platform), wheeled walkers, and wheelchairs, are used when walking is limited by lower extremity joint instability, pain, weakness, and fatigue or balance problems. These devices are easily accessible and provide immediate assistance, but they require more physical effort than is required for normal ambulation. The choice of a mobility device is based on impairments and resulting disability (e.g., patients with RA with bilateral upper extremity involvement and leg weakness may be safer ambulating with platform than axillary crutches). Patients with balance disturbances and leg weakness may be better suited for walkers. The device type also impacts the weight-bearing status. For example, a single-point cane can bear about 25% of body weight, axillary or forearm crutches about 50%, and a wheeled walker more than 50%.73 Wheelchairs are necessary if patients are unable to walk with devices. In these cases, a wheelchair can improve the quality of life by maintaining some mobility. Persons unable to navigate a manual wheelchair can profit from an electrical chair. Accidents can occur while traversing ramps, sidewalks, and streets.35 |
| Vocational rehabilitation | Vocational rehabilitation is an interdisciplinary approach that enables patients to acquire and maintain gainful employment and varies among countries. A common feature consists of problem assessment at work and the development of individual solutions. Studies demonstrate that vocational support prevents or delays work disability and improves fatigue and mental health.74 |
| Work hardening/functional restoration programs | These highly structured, goal-oriented, individually tailored programs are provided by an interdisciplinary professional team to address functional, physical, behavioral, and vocational needs to facilitate return to work.75 Work hardening programs bridge the gap between initial injury and return to work. Most programs include a formal worksite ergonomic to address workplace design issues and to reduce injury risk while improving function, as well as social interventions. The Commission on Accreditation of Rehabilitation Facilities defined and developed standards for work hardening practice to standardize program content and implementation.75 Work hardening programs integrate real or simulated work activities to model appropriate behaviors and assess functional, biomechanical, neuromuscular, cardiovascular/metabolic, behavioral, attitudinal, and vocational performance.75 A systematic review of these programs provides evidence for significant reductions in sick days.12 |
| Self-management and patient education | Patient education is defined as a set of planned educational activities used to improve a patient’s health behaviors and/or health status. Most patient education programs are provider driven and developed. Self-management programs are patient oriented and patient active, and combine education with cognitive-behavioral strategies to influence patients’ attitudes toward disease and disease management.85 |
| Cognitive-behavioral therapy (CBT) | CBT acknowledges that pain and its resulting disability are influenced by somatic pathology, and by psychological and social factors. In general, three behavioral treatment approaches are distinguished: operant, cognitive, and respondent. The primary focus is to reduce disability. A review of 21 studies found no significant differences between the various types of CBTs; also, CBTs did not differ from exercise. A conclusion regarding whether clinicians should refer patients with chronic low back pain to behavioral treatment programs or to active conservative treatment was not possible.76 |
ICF, International Classification of Functioning, Disability, and Health; OA, osteoarthritis; RA, rheumatoid arthritis.
Self-management programs are patient focused, patient driven, and action oriented.85 These programs combine education, behavioral interventions, and cognitive strategies to enable patients to problem-solve, cope, and develop strategies to maximize function and independence. A focus of these programs is to assess and influence patients’ attitudes and beliefs about disease and their ability to manage their disease. Self-management programs demonstrate benefits with respect to disease outcomes85,86 and have proved cost-effective.86
Evidence of the benefits of physical modalities, therapeutic relaxation techniques (massage, trigger point therapy) and splinting, orthotics, and gait deviation interventions varies across intervention type and disease. Overall, the evidence is weak.8–10,13,87 However, it is important to note that relaxation and physical modalities are adjunct therapies designed to prepare a patient for dynamic exercise, flexibility training, or gait training and are not stand-alone interventions.87 Additionally, many patients report satisfaction with and preference for these therapies.88