Infected Total Knee Replacement: Two-Stage Exchange Using the PROSTALAC System
Between 1 and 2% of knee replacements are complicated by deep infection. In most cases, the infection will not be eradicated without removal of the implants. The ideal treatment includes reimplantation of another knee replacement, with good function1 and without infection.2,3 Although a one-stage exchange of the infected knee replacement with a new implant at the same time as a thorough debridement has been reported with good results, these results have been reported, for the most part, from one center, and excellent results have not been reproduced elsewhere. The standard of treatment therefore, continues to be a two-stage exchange arthroplasty, where the implants are removed and the knee is debrided at one operation, and the revision total knee arthroplasty components are reimplanted at a second operation, at least 6 weeks later.2,3 In the interim, intravenous antibiotics are administered for 6 weeks. Apart from the need for two operations, the next most obvious misgiving about this approach is that the knee is compromised between stages, with nothing to maintain stability and mobility following the excision arthroplasty at the first stage.
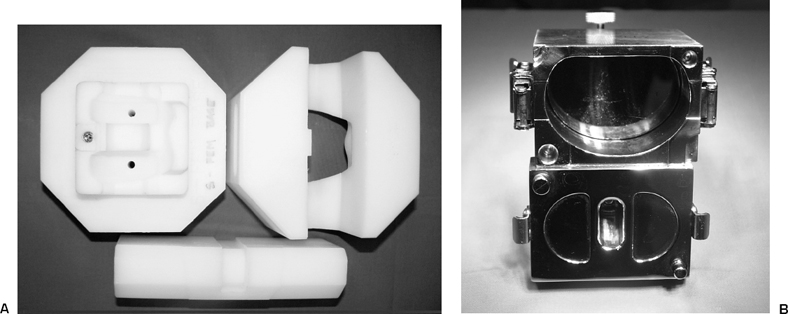
Although a variety of spacers in the form of antibiotic-loaded bone cement have been used to maintain at least an extension space between stages, for the most part these spacers have been static rather than dynamic spacers that do not allow much mobility, and in particular do not allow enough stability to allow reasonable ambulation between stages without immobilization devices. The authors introduced the prosthesis of antibiotic-loaded acrylic cement (PROSTALAC), which is an interim functional spacer made primarily of antibiotic-loaded acrylic cement, and allows motion and some weight bearing between stages in a two-stage exchange arthroplasty for infection after a total knee arthroplasty.3–5 Since the introduction of this system, other articulated spacers have been introduced and are currently in use.
Indications
Chronic infection after total knee arthroplasty in a patient in whom retention of a mobile knee is preferred
Contraindications
- Persistent uncontrolled infection elsewhere, such as another infected joint arthroplasty, infected heart valve, infected ulcer, or another infected prosthetic device
- Lifestyle issues that are incompatible with a major joint replacement, such as ongoing intravenous drug use
- Bone and/or soft tissue defects that cannot be reconstructed using standard orthopaedic and plastic surgical techniques
- Severe immune compromise making reimplantation of another knee replacement too risky
- Inadequate circulation in the lower extremity to support a revision total knee arthroplasty procedure
- Previously failed two-stage exchange arthroplasty for infection
Physical Examination
- Assess deformity and range of motion.
- Swelling, with a large effusion or boggy synovitis
- Draining or recently closed sinuses may or may not be present.
- Wound-edge necrosis may be present after the last operation.
- Beware of multiple incisions about the knee.
Diagnostic Tests
- The erythrocyte sedimentation rate (ESR) and the C-reactive protein (CRP) are often elevated.
- An aspiration of the knee joint is almost always positive for the infecting organism. This will be misleading if the patient was being treated with antibiotics before referral.
- Nuclear medicine scans such as serial technetiumindium scans are rarely needed.
- Standing anteroposterior, lateral, and skyline views, in addition to leg-length films, are essential for pre-operative planning.
- Nuclear medicine scans such as serial technetiumindium scans are rarely needed.
Special Considerations
The sensitivity profile of the infecting organism should be known preoperatively to select the appropriate antibiotics for incorporation within the cement, and to choose the appropriate antibiotics for parenteral therapy postoperatively. These knees are often stiff, and the components are almost always solidly fixed, and therefore an extensile exposure that allows the safe removal of the implants without adversely affecting the remaining bone stock is important.
Preoperative Planning and Timing of Surgery
Most knees that require a two-stage exchange arthroplasty are chronically infected. If an infection is detected within 2 to 3 weeks after operation, or within a few days of the onset of symptoms in a knee that was otherwise doing well with no symptoms, a debridement and irrigation with retention of the components may be attempted. Otherwise, a two-stage exchange arthroplasty should be recommended and should be performed as urgently as possible to avoid further bone loss due to infection. It is the authors’ experience that bone loss can deteriorate much more rapidly after an infected knee arthroplasty than after an infected hip arthroplasty, particularly when intraosseous abscesses are present. This is difficult to determine preoperatively.
Preoperative planning should include the following steps:
- Determine the appropriate antibiotics to be used in the cement as well as parenterally after the first stage operation.
- Determine the alignment of the existing components, and determine how best to correct the alignment (changing the alignment of the femoral or tibial components).
- Determine the status of fixation of each component, and the type of fixation (with or without cement).
- Determine the sizes of the revision implants that may be required. This will determine the size of the PROSTALAC components.
Special Instruments
- Implant extraction instruments
- Straight and curved osteotomes
- Moreland knee instruments (DePuy, Warsaw, IN)
- Moreland cement removal instruments (DePuy, Warsaw, IN) for removing excess cement within the intramedullary canal of the tibia
- High-speed burr for removing excess cement with in the intramedullary canal of the tibia, and for removing small amounts of buried cement, partic ularly within lug-fixation holes in the femur and in the patella
- Component extraction devices other than the Moreland extraction punch may rarely be required (Innomed, Savannah, GA)
- Gigli saws for removing solidly fixed cementless femoral components
- The appropriate screw drivers for cementless tibial components
- Straight and curved osteotomes
- PROSTALAC molds (Fig. 42–1)
- Antibiotic-loaded cement: the authors prefer Palacos (Smith and Nephew, Richards, Memphis, TN)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








