Infected Total Knee Replacement: Cement Spacer
An antibiotic-containing bone cement spacer can be a valuable adjunct during the treatment of an infected total knee replacement with the two-stage reimplantation of another prosthesis. By simultaneously delivering high local concentrations of antibiotics and preserving the soft tissue envelope, bone cement spacers can be beneficial to both the patient and the revision knee surgeon. A well-made cement spacer confers stability to the knee, enhances early patient mobilization, and limits a patient’s period of disability. In addition, by preventing marked joint contracture, an appropriate cement spacer simplifies the exposure of the knee at the time of reimplantation of another prosthesis. In contrast a poorly constructed spacer can lead to marked bone loss, and if left in place for too long, a cement spacer can become a foreign body to be colonized by bacteria.
Indications
Useful during the interval between resection of an infected total knee replacement and the reinsertion of a new prosthesis as part of a planned two-stage reimplantation protocol.
Contraindications
A prolonged interval between resection and reimplantation is a relative contraindication. Beyond 6 weeks concerns arise that the cement spacer will become an inert foreign body subject to bacterial colonization.
Physical Examination
Determine the integrity of the skin and soft tissue envelope to ensure that wound healing problems will not occur after resection and placement of the cement spacer. If in doubt, preoperative consultation with a plastic surgeon for consideration of muscle flap coverage is useful.
Diagnostic Tests
A typical workup for suspected infection should include a complete blood count with differential, C-reactive protein, and sedimentation rate, knee aspiration for cell count and culture, and selective use of bone and indium scanning.
Special Considerations
Be certain that the patient is not allergic to one or more of the antibiotics that will be used in the bone cement spacer.
Preoperative Planning and Timing of Surgery
Timing is dictated by the acuity of the infection. A chronic low-grade infection can often be dealt with on an urgent but not emergent basis. A fulminant acute infection should be addressed quickly, particularly if there is the risk of seeding other total joint arthroplasties or other prosthetic devices.
Special Instruments
- Appropriate extraction equipment must be obtained to allow removal of the infected knee prosthesis with minimal bone loss.
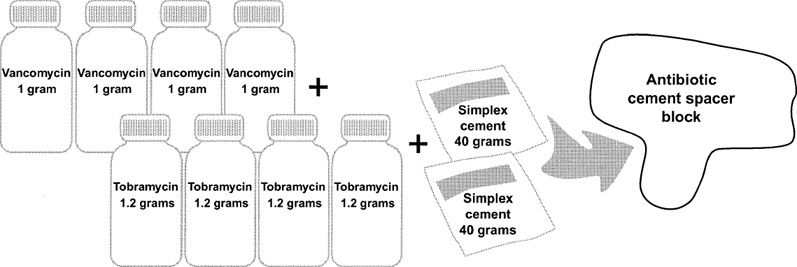
- Adequate amounts of the appropriate antibiotics in powder form must be available. We will often mix 4 to 8 g of vancomycin powder and 4.8 to 9.6 g of tobramycin powder with one or two batches (40 to 80 g) of cement to form the spacer (Fig. 41–1).
Anesthesia
We typically employ general anesthesia in the face of infection.
Patient and Equipment Positions
The patient is positioned supine with a tourniquet proximally on the thigh.
Surgical Procedure
Approach
The previous skin incision is used whenever possible. When multiple incisions are present, it is most appropriate to use the most lateral anterior incision to avoid skin necrosis.
Dressings, Braces, Splints, and Casts
- The knee is initially placed in a well-padded Robert-Jones dressing.
- Until the time of reimplantation, the knee is protected in a knee immobilizer.
Tips and Pearls
- An appropriately fashioned spacer block will not overdistract or stretch the collateral ligaments but should fill the extension space enough to impart moderate mediallateral stability to the knee. A knee immobilizer is used to supplement the mediallateral stability conferred by the spacer block.
- Prevent settling of the cement spacer into soft cancel-lous bone by making the cement spacer block as wide as the host tibia and femur in both the anteroposterior and the lateral planes so as to rest on a cortical rim.
- Early mobilization with partial weight bearing may be done if the knee is stable in the knee immobilizer and the cement spacer caps the exposed bone of the distal femur and proximal tibia.
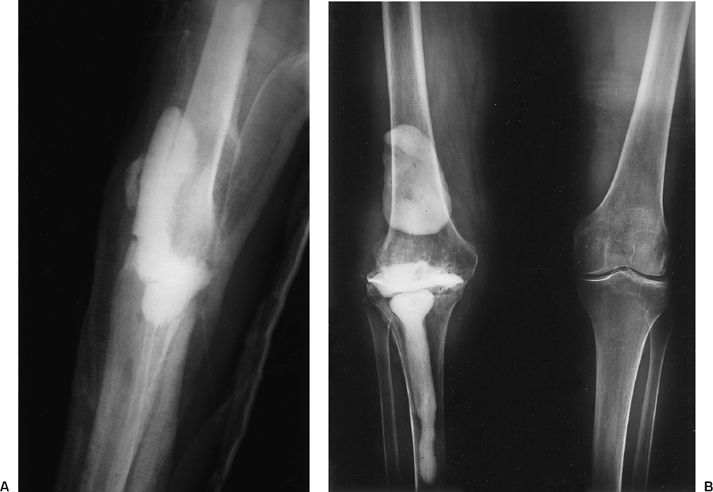
- An effective cement spacer block can be made in many different shapes. The basic criteria for success are (a) fill but do not overdistract the extension space, (b) extend the cement over the anterior portion of the femur to preserve the patellofemoral joint and prevent fusion of the patella to the femur, (c) extend the cement to the cortices of the distal femur and proximal tibia in all planes, and (d) allow for intramedullary extension of cement to prevent spacer migration. Those criteria can be met with spacer blocks that are L-shaped blocks or are molded to resemble tibial and femoral components or with largely amorphous and serpiginous blocks (Figs. 41–2, 41–3, and 41–4).
- When cement is used to fix an implant, the dose of antibiotics should be limited to 1 g per 40 g batch of cement. With a spacer block, however, one goal is the sustained elution of high local concentrations of antibiotics, and in that setting, it is more appropriate to use 4 g or more of antibiotics per 40 g batch of bone cement. Combining two antibiotics in the cement spacer is also beneficial as it broadens the antimicrobial coverage and improves the elution characteristics of the antibiotics from the bone cement. Our current clinical practice is to mix at least 2 g of vancomycin with 2.4 g of tobramycin per 40 g batch of Simplex cement. Often that antibiotic ratio is doubled.
- Reimplantation of a new total knee replacement should be planned for 4 to 6 weeks after the resection, provided that the infection has not recurred, and should be done with antibiotic-containing bone cement for prosthetic fixation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








