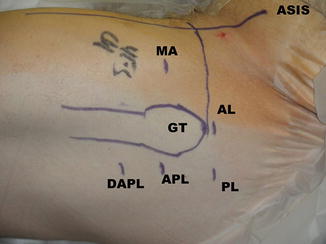
Fig. 1
The borders of the subgluteal space. (a) Cadaveric dissection of a right subgluteal space, visualized from posterior. Note the entrance of the sciatic nerve just below the piriformis tendon and lying on the common tendon (B/ST common tendon of biceps and semitendinosus that has been partially detached and slightly everted, IT ischial tuberosity, QF quadratus femoris). (b) A diagrammatic representation of a right subgluteal space (CT conjoint tendon of the superior and inferior gemelli, along with the obturator internus, GM gluteus maximus muscle, everted, IT ischial tuberosity, QF quadratus femoris). (c) An axial, T1-weighted image of a right hip. The yellow line outlines the borders of the space (SN sciatic nerve, P piriformis muscle, GT greater trochanter, GM gluteus maximus)
The contents of the space include the sciatic nerve, the piriformis, the obturator internus/externus, the gemelli, the quadratus femoris, the hamstrings, the superior and inferior gluteal nerves, the lateral ascending vessels of the medial femoral circumflex artery, the ischium, the sacrotuberous and sacrospinous ligaments, and the origin of the ischiofemoral ligament.
Some specifics of the anatomy are critical to understanding the pathological processes that are encountered within the space. From the sciatic notch, the piriformis muscle originates from the ventrolateral surface of the sacrum and courses between the iliotibial band and inserts on superior and posterior aspect of the greater trochanter (Fig. 1). Distal to the piriformis is the cluster of short external rotators: the gemellus superior, obturator internus, and gemellus inferior (Fig. 2). The gemelli blend with the obturator internus onto the anterior aspect of the medial surface of the greater trochanter [3]. The piriformis tendon can be partially blended with this common tendon in its insertion [4]. The obturator internus arises from the inner surface of the anterolateral wall of the pelvis and exits the pelvis through the lesser sciatic foramen. The superior gemellus arises from the outer surface of the ischial spine, and the inferior gemellus arises from the ischial tuberosity. Inferior to this complex is the quadratus femoris, which arises from the upper part of the external border of the ischial tuberosity and inserts on the posterior surface of the femur, along the intertrochanteric ridge. The quadratus assists in external rotation, while the piriformis and short external rotators assist external rotation and abduction of the flexed hip. At the ischium, the biceps femoris and semitendinosus have a common tendinous origin that separates about nine cm from the proximal border of the origin [5] (Fig. 3).
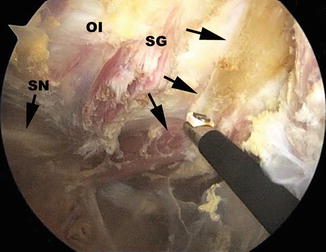
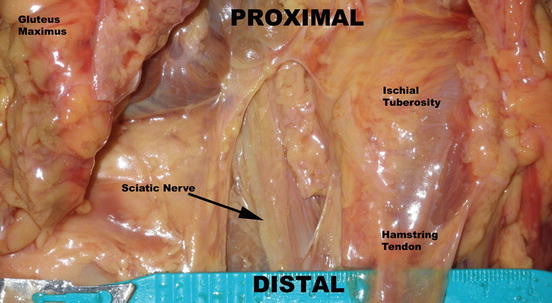
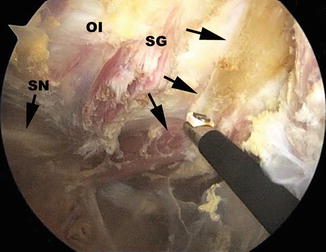
Fig. 2
The sciatic nerve (SN) resting on the common tendon and exiting below the piriformis (arrows) (OE obturator externus, SG superior gemellus)
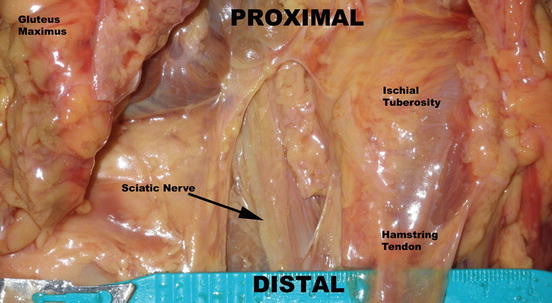
Fig. 3
The lower portion of the deep gluteal space (the view is of a left hip, from the posterior aspect)
Six neural structures exit the pelvis through the greater sciatic notch. The neural structures include the sciatic, pudendal, posterior femoral cutaneous, superior gluteal, and inferior gluteal nerves and the nerve to the obturator internus. In addition, the superior and inferior gluteal arteries also exit through the greater sciatic notch. The sciatic nerve courses distally through the space anterior to the piriformis muscle and posterior to the obturator/gemelli complex as well as the quadratus femoris. There are, however, a number of anomalies that are commonly encountered that include entry into the space either through or posterior to the piriformis. These have been documented in up to 17 % of cases in several cadaveric studies [6]. The superior gluteal artery and nerve divide 1–2 cm above the superior border of the piriformis and fan out in a course anterior and distal to the greater sciatic foramen between the gluteus minimus and medius, supplying those muscles and the tensor fascia femoris [7]. The inferior gluteal nerve and artery enter the pelvis at the greater sciatic notch medial to the sciatic nerve between the piriformis and coccygeus muscles [3]. It descends, along with the sciatic and posterior femoral cutaneous nerves, between the greater trochanter and the ischial tuberosity. Clinically, this nerve is found penetrating the gluteus maximus five cm above its inferior border.
The medial circumflex artery is also relevant within the space. If follows the inferior border of the obturator externus and crosses over its tendon and under the external rotators and piriformis muscle. This vessel terminates as the lateral retinacular vessels, which are the principal blood supply of the femoral head in adults.
The sciatic nerve is located at an average of 1.2 ± 0.2 cm from the most lateral aspect of the ischial tuberosity. Under normal conditions, the sciatic nerve is able to stretch and glide to accommodate strain or compression that occurs with hip motion. One study has documented that with a straight leg raise and knee extension, the sciatic nerve experiences a proximal excursion of 28 mm medial toward the hip joint [8]. Any entrapment of the nerve, therefore, may increase the likelihood of decreased translation of the tissues and subsequent development of pain in the nerve’s distribution. Sources of sciatic nerve entrapment include hamstring tendon disruptions and their consequent scar formation immediately adjacent to the nerve. The piriformis tendon is also commonly implicated in compression of the nerve. In addition, malunited ischial avulsion or lesser trochanteric fractures can lead to perineural scar formation. Other etiologies include vascular anomalies, tumors, as well as the gluteus maximus tendon in cases of prior iliotibial band releases. Remote acetabular fractures can also lead to nerve impingement.
One other source that is starting to be understood is ischiofemoral impingement. The disorder has been described in the radiological literature to some extent [9–11]. The mechanism is that of entrapment of the nerve between some portion of the posterior femur and the ischium. The anatomy of this space makes it susceptible to impingement as the clearance between the structures is minimal, especially at the extremes of motion (Fig. 4). In some cases, the quadratus femoris is hypertrophied, and surgical release is indicated. As well, the lesser trochanter, lying underneath this muscle, may be prominent. Care must be taken during the release of this muscle, as the medial circumflex femoral vessels are within the surgical field. It is vitally important not to compromise these, since they are the primary blood supply to the femoral head, as stated previously.
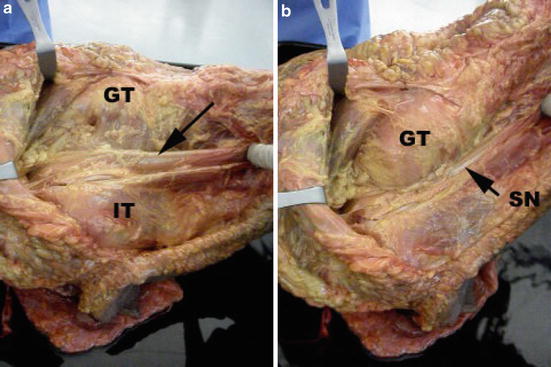
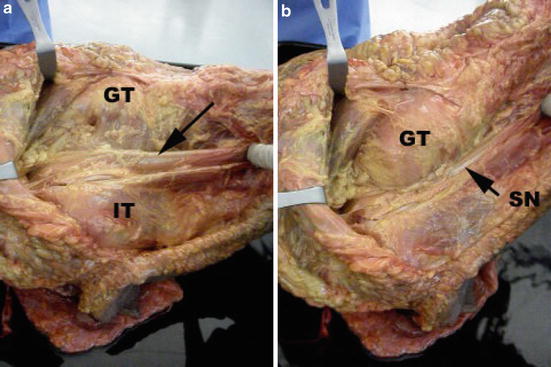
Fig. 4
Ischiofemoral impingement in a cadaver. The view is of a right hip and the proximal portion is to the left. (a) With the leg in neutral rotation that is the space between the trochanter (GT) and the ischium for the sciatic nerve (SN) to glide. (b) With external rotation, there is a diminished space between the GT and the ischium (IT)
Surgical Technique
In most cases, the procedure is performed in the supine position and may be performed concomitant to a hip arthroscopy of the central and/or peripheral compartments, if indicated. The procedure is performed with the 30° arthroscope. In some cases, however, it is useful to employ the 70° device for added visualization. It is also possible to require the use of a longer arthroscope (probably a 70° device) in larger patients. The procedure can also be performed in the lateral position with the leg in a slightly abducted position (Fig. 5). This is done in cases where there is no central or peripheral compartment pathology that needs to be addressed.


Fig. 5
Positioning for access to the deep gluteal space in the lateral position. Note the leg is abducted about 30°
In the supine position, following the completion of the central and peripheral work, any traction is discontinued, and the leg is abducted to about 30° in order to open the interval between the trochanter and the iliotibial band. The leg is internally rotated, for the same reason. Entrance into the subgluteal space is accomplished by traveling through the peritrochanteric space, which is between the greater trochanter and the iliotibial band. A modified anterior (MA) portal, which has been used for anterior visualization of the central and peripheral compartments, is used to enter the peritrochanteric space between the tensor fascial femoris (laterally) and the rectus femoris (medially) [1] (Fig. 6). This is accomplished by palpating the interval between these two muscle bellies with the blunt arthroscopic probe and cannula. Ultimately, the space is successfully entered when the lateral aspect of the greater trochanter is palpated and can be confirmed with the use of fluoroscopic guidance. An anterolateral (AL) portal is then employed as a working portal in the trochanteric bursa. The procedure then continues by exposure of the bursa and resection of abnormal bursal tissue, as necessary (Fig. 7).