Fig. 1
Patient setup in the supine position for left hip arthroscopy
Gentle hip distraction is applied to obtain approximately 10 mm of joint distraction confirmed fluoroscopically (see Fig. 2a, b). The goal is to use the minimal force required to achieve adequate distraction and keep traction time as brief as possible (preferably less than 2 h). It is important that the distraction system employed allows for adequate mobility of the operative hip specifically in flexion, abduction, and/or adduction of the hip. Freedom of movement in these planes is essential to achieving sufficient visualization and optimal maneuverability during surgery [19, 20].
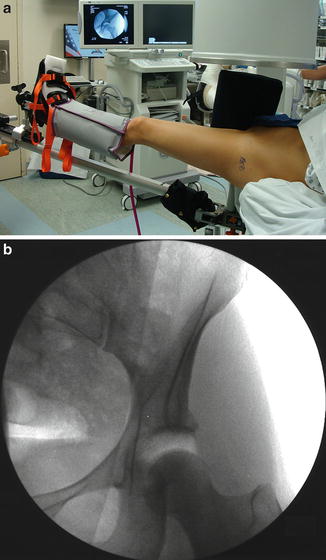
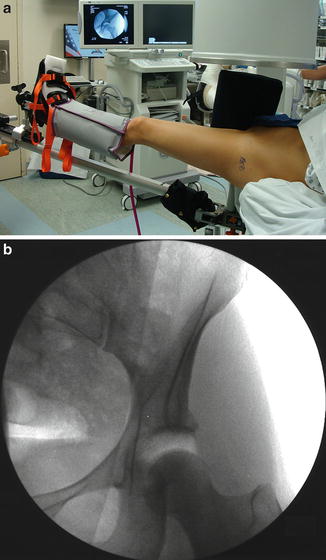
Fig. 2
(a) The left lower extremity is seen in approximately 10 mm of distraction and (b) confirmed fluoroscopically
Portal Placement
After proper traction is applied, the operative extremity is placed in neutral abduction. Slight hip flexion can be added, as it may relax the anterior capsule and aid in portal placement. The principal landmarks are identified and marked including the greater trochanter, anterior superior iliac spine (ASIS), pubic symphysis, and femoral shaft. Arthroscopic access to the central compartment of the hip joint is based on two to three standard portals that are routinely established: anterolateral (AL), anterior, and/or posterolateral (PL) portals. A more commonly used portal in recent years is the midanterior portal (MAP). The AL portal is used as the introductory portal for virtually all routine hip arthroscopy. The anatomical landmarks and position of these portals are demonstrated in Fig. 3.
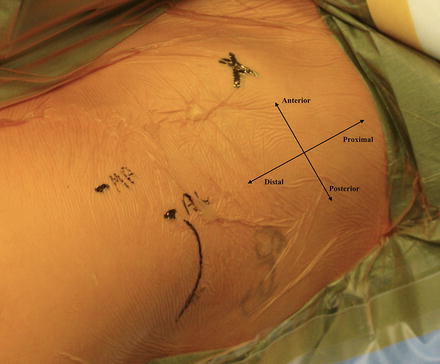
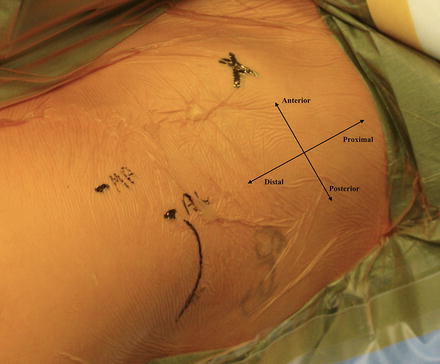
Fig. 3
Anatomical landmarks are outlined including the greater trochanter (curved line) and anterosuperior iliac spine (marked “X”); the anterolateral (AL) and midanterior (MA) portals are also labeled
Anterolateral Portal
The AL portal is usually established as the introductory portal. It is easier to access, reproducible, and presents relatively less risk to the surrounding neurovascular structures. The entry point on the skin is approximately 1 cm anterior and 1 cm superior to the anterosuperior tip of the greater trochanter. This portal was traditionally described as penetrating the gluteus medius muscle and entering the lateral capsule at its anterior margin [17]. Another well-described technique for establishing the AL portal is through the intermuscular interval between the abductors and the tensor fasciae latae. In some patients, when traction is applied to the operative extremity, a palpable ridge can be identified along the anterolateral thigh at the level of the AL portal insertion site. This palpable ridge is formed by the transition zone between the posterior border of the tensor fascia lata and the anterior border of the gluteus maximus fascia, which merge in line with the anterior aspect of the greater trochanter. When done properly, the portal will penetrate the gluteal fascia and then pass down to the joint capsule with minimal soft-tissue resistance as it passes atraumatically between the tensor fasciae latae anteriorly and the gluteus medius posteriorly [11].
The joint capsule is punctured with a large-gauge spinal needle (17 G or 16 G) under fluoroscopic guidance. The needle should be inserted through the AL portal insertion site with a slightly posterior (20–30°) and cephalad (10–20°) trajectory toward the hip joint and between the femoral head and acetabular labrum. A tactile feedback of a resistance felt when the needle penetrates the thick joint capsule with an immediate decrease of this resistance after penetration of the capsule can signify proper positioning of the needle without injury to the intra-articular structures at risk.
Successful entry into the central compartment of the hip joint is confirmed with an air arthrogram. This is performed by removal of the spinal needle stylus and breaking the vacuum seal of the joint. This should provide for additional distraction of the hip joint and often enables fluoroscopic visualization of a silhouette of the acetabular labrum. The joint can also be filled with saline at this time with observed backflow confirming the intra-articular position of the spinal needle. A nitinol guidewire is then placed through the spinal needle, and a stab incision is made through the skin adjacent to the needle. The needle is removed, leaving the nitinol wire and cannulated dilators placed over the guidewire to allow for easier passage of the final obturator. It is important to direct the various cannulas superiorly away from the convexity of the femoral head in order to avoid inadvertent scuffing of the articular cartilage [18].
A 70° arthroscope is then used to perform a diagnostic arthroscopic examination and to establish the other portal(s) under direct visualization. This process of spinal needle, nitinol wire, dilators, and obturator placement is used for all subsequently portals and is an important aspect of safe portal placement. After placement of other portals, the arthroscope can be introduced into another portal in order to visualize the position of the anterolateral portal in relation to the acetabular labrum and make adjustments if necessary.
The anterolateral portal in the central compartment enables arthroscopic visualization of the following structures: cotyloid fossa, pulvinar, ligamentum teres, posterior medial acetabulum and labrum, anterior labrum, anterior capsule, paralabral sulcus, and the intra-articular portion of the psoas tendon and corresponding bursa. The anterior triangle, containing the anterior capsule, anterior labrum, and femoral head, is a very helpful landmark allowing for direct visualization of the spinal needle when establishing the anterior portal (see Fig. 4) [18].


Fig. 4
Structures visualized through the anterolateral portal including the anterior triangle, anterior labrum/capsule (asterisk), and femoral head (FH)
Risks
The anterolateral portal is located centrally within the safe zone of access to the hip joint, minimizing the risk of damage to neurovascular structures. The superior gluteal nerve, coursing on the deep surface of the gluteus medius, and the sciatic nerve are the closest neurovascular structures to this portal located a mean distance of 64.1 and 40.2 mm, respectively, from the anterolateral portal [11].
The main concern when establishing the AL portal under solely fluoroscopic control is possible damage to the intra-articular structures such as scuffing the articular cartilage of the femoral head or perforating the acetabular labrum. A recent study of 250 patients reported an iatrogenic labral puncture rate of up to 20 % [13]. Strategies to minimize labral injury include using adequate distraction, joint distention, tactile feedback, reintroducing the spinal needle after distention of the joint with saline, as well as spinal needle repositioning with or without arthroscopic visualization from other portals. Careful attention to detail and proper technique can reduce the likelihood of iatrogenic injury [10, 13, 18].
In addition, novel techniques for minimizing the risks while accessing the central compartment of the hip joint have been described and published in recent years. One technique describes placing the arthroscope first in the peripheral compartment through the anterolateral portal followed by placement of a spinal needle and guidewire into the central compartment via an anterior portal under direct arthroscopic visualization [3]. Another technique describes directing the AL portal needle slightly anteroinferior to the clear space of the distracted joint overlapping the superior part of the femoral head, thereby directing the needle away from the labrum [14].
Anterior Portal
Several variations of positioning the anterior portal have been described. The traditional location of the skin entry point of the anterior portal was at the intersection of a sagittal line drawn down from the anterior superior iliac spine (ASIS) and a transverse line from the superior border of the greater trochanter. Insertion of the spinal needle is aimed approximately 45° cephalad and 30° toward the midline. It was found that when positioned this way, in line with the ASIS, this portal penetrates the sartorius muscle and the rectus femoris muscle before entering the anterior joint capsule and passes in dangerously close proximity to branches of the lateral femoral cutaneous nerve (3 mm) and the ascending lateral circumflex femoral artery (3 mm) [11, 12, 17]. Some have advocated placing the AP portal 1 cm lateral to its traditionally described location (i.e., 1 cm lateral to the ASIS) reducing the risk of lateral femoral cutaneous nerve (LFCN) and lateral circumflex femoral artery (LCFA) iatrogenic injury. When positioned laterally, the portal penetrates the muscle belly of the tensor fasciae latae (TFL) and passes through an interval between the gluteus minimus and rectus femoris before entering the joint through the anterior capsule. It courses a mean distance of 15 mm lateral to the LFCN and its branches, 31 mm proximal to the ascending LCFA, and 15 mm lateral to the ascending LCFA terminal branch [11].
The anterior portal is established under direct visualization using a 70° arthroscope in the anterolateral portal. The spinal needle is directed toward the anterior triangle. The anterior portal in the central compartment enables arthroscopic visualization of the following structures: ligamentum teres, posterior transverse ligament, posteromedial labrum, anterior transverse ligament, anterior labrum, superior articular cartilage, lateral labrum, and posterolateral capsule.
Risks
Special care and attention should be taken when inserting the AP portal. As mentioned, branches of the lateral femoral cutaneous nerve and lateral circumflex femoral artery are in close proximity to the portal and most at risk. Positioning the skin entry point 1 cm laterally places the portal path further away from these structures and may mitigate this risk. An important consideration is the anatomical variation of the proximal LFCN branching site, present in nearly 25 % of patients [19]. In these cases, the most lateral branch of the LFCN might be even closer to the AP portal. Stab incisions should be avoided in the anterior portal in an effort to prevent iatrogenic injury to these branches. The femoral neurovascular bundle is normally located a safe mean distance of more than 3 cm from the portal, and the vertical line marked from the ASIS distally can be used as the medial border of the safe zone. Because this portal is established under direct visualization, the risk to intra-articular structures should be minimal.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








