Heel and Subcalcaneal Pain
Keith L. Wapner
INTRODUCTION
Pain about the heel is a common problem presenting to the orthopedic surgeon. Successful treatment depends on a proper identification of the cause of the pain with a careful history and physical examination, so that an appropriate treatment regimen can be initiated. Patients should be informed of the challenge inherent in treating the problem while allowing ambulation. The duration for the resolution of symptoms can be a great source of frustration to the patient and physician. Most authors recommend that conservative modalities should be employed for 6 to 12 months prior to consideration for surgical intervention. Heel pain can be divided into two primary entities: subcalcaneal pain and posterior heel pain syndromes. It has been suggested that although these heel pain syndromes are familiar to all orthopedic surgeons, probably they are not completely understood as yet.
POSTERIOR HEEL PAIN
INTRODUCTION
Pain located in the posterior portion of the calcaneus can be produced by multiple causes and should be distinguished from subcalcaneal heel pain by history and physical examination. Pain in the posterior, superior portion of the calcaneus may arise as a result of the following:
Retrocalcaneal bursitis
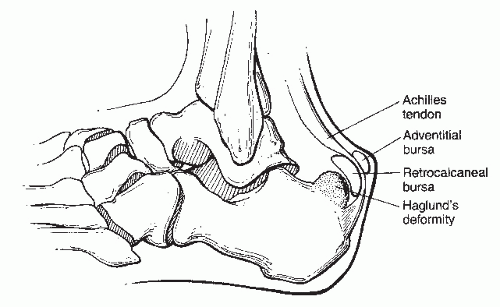
Enlargement of the superior bursal prominence of the calcaneus known as Haglund deformity (Fig. 9.1) Insertional Achilles tendinosis
Inflammation of an adventitious bursa between the
Achilles tendon and the skin (Fig. 9.1).
Each of these entities may exist as an isolated condition or may be part of a symptom complex. Careful analysis of the patient’s subjective complaints and objective findings is required for correct diagnosis.
PATHOGENESIS
Etiology
Enlargement of the posterior, superior aspect of the calcaneus (Haglund deformity) can lead to impingement on the insertional fibers of the Achilles tendon, producing irritation over the bony prominence and the tendon fibers. Haglund syndrome is a combination of the enlarged bony prominence creating insertional tendinosis, retrocalcaneal bursitis, and adventitial bursitis. When Achilles tendinosis occurs with Haglund syndrome, it is generally located in the area of the Achilles tendon just at or above the insertion of the Achilles at the posterior portion of the os calcis but not more proximally. Ossification within the Achilles tendon in this area represents ossification in a degenerative area of the tendon. Achilles tendon pathology can be divided into insertional and noninsertional dysfunctions. Insertional tendinosis occurs within and around the Achilles tendon at its insertion and may be associated with Haglund deformity or spur formation within the tendon itself. Insertional Achilles tendinosis represents a biologic disorder of tendon degeneration from constant intrinsic loading, whereas retrocalcaneal bursitis is a manifestation of impingement of the bursa between the Achilles tendon and the calcaneal process. Inflammation of the adventitious bursa, between the Achilles tendon and the overlying skin, is usually caused by pressure of the counter of the shoe against the prominent area. It is more common in women and less common in athletes.
Epidemiology
Retrocalcaneal bursitis tends to manifest in younger populations (30s), whereas insertional Achilles tendinosis with a calcific spur is present in an older population.
Anatomy
The Achilles tendon inserts into the middle of the posterior part of the posterior surface of the calcaneus. A retrocalcaneal bursa located between the Achilles tendon and the superior tuberosity of the calcaneus is a constant finding.
Dorsiflexion of the foot and ankle produces increased pressure in the retrocalcaneal bursa; plantarflexion decreases the pressure in the retrocalcaneal bursa. Anatomically, the retrocalcaneal bursa has an anterior bursal wall comprising fibrocartilage laid over the calcaneus, whereas the posterior wall is indistinguishable from the thin epitenon of the Achilles tendon. It is a disc-shaped structure lying over the posterior superior aspect of the calcaneus, fitting like a cap over the calcaneus and having a concave aspect anteriorly. The retrocalcaneal bursa maintains the relatively constant distance between the axis of the ankle joint and the insertion of the Achilles tendon. If the posterior prominence were not present, there will be shortening of the distance between the ankle joint axis and the insertion of the Achilles tendon during dorsiflexion. As this lever arm shortens, the ability of the gastrocnemius—soleus muscle to function is affected. Thus this projection works as a cam, allowing the tension of the gastrocnemius—soleus muscle group through the Achilles tendon to remain constant with dorsiflexion and plantarflexion.
Dorsiflexion of the foot and ankle produces increased pressure in the retrocalcaneal bursa; plantarflexion decreases the pressure in the retrocalcaneal bursa. Anatomically, the retrocalcaneal bursa has an anterior bursal wall comprising fibrocartilage laid over the calcaneus, whereas the posterior wall is indistinguishable from the thin epitenon of the Achilles tendon. It is a disc-shaped structure lying over the posterior superior aspect of the calcaneus, fitting like a cap over the calcaneus and having a concave aspect anteriorly. The retrocalcaneal bursa maintains the relatively constant distance between the axis of the ankle joint and the insertion of the Achilles tendon. If the posterior prominence were not present, there will be shortening of the distance between the ankle joint axis and the insertion of the Achilles tendon during dorsiflexion. As this lever arm shortens, the ability of the gastrocnemius—soleus muscle to function is affected. Thus this projection works as a cam, allowing the tension of the gastrocnemius—soleus muscle group through the Achilles tendon to remain constant with dorsiflexion and plantarflexion.
The superior tuberosity of the os calcis may be hyperconvex, normal, or hypoconvex. The radiographic anatomy of the os calcis has been described in terms of the following anatomic landmarks on the lateral projection.
The superior aspect of the talar articulation marks the most proximal portion of the posterior facet.
The bursal projection is the area of the superior tuberosity of the os calcis.
The tuberosity of the posterior surface marks the site of the Achilles insertion.
The medial tubercle is the site of insertion of the central portion of the plantar aponeurosis.
Pathophysiology
Retrocalcaneal pain syndrome is commonly associated with a high-arched cavus foot with a varus heel. The combination of these factors tends to produce a foot that does not dorsiflex as readily as a normal foot. There is prominence of the heel, which is more susceptible to increased pressure from the tendons and the counter of the shoe. Retrocalcaneal bursitis generally occurs in the circumstances of compensated rearfoot varus, compensated forefoot valgus, and a plantar-flexed first ray because of the abnormal motion of the subtalar joint and the frontal and sagittal plane relationships. Varus hindfoot tends to accentuate the posterior superior prominence by making the heel more vertical.
Ruptures of the Achilles tendon occur most commonly in the segment between 2 and 6 cm proximal to its insertion in the os calcis, an area of decreased vascularity and nutrition. This is an important finding relative to the retrocalcaneal bursal syndrome because this classic type of Achilles tendinosis is proximal to the area usually associated with the retrocalcaneal bursal syndrome. This may suggest that insertional tendinosis is brought on by impingement on the tendon because of the morphology of the foot or the prominence of the calcaneus rather than decreased circulation.
DIAGNOSIS
Physical Examination and History
The history in general comprises the following:
Slow onset of dull ache in the retrocalcaneal area aggravated by activity and certain shoe wear.
Start up pain after sitting or when arising out of bed in the morning.
Gradual swelling at the area of the Achilles insertion.
Clinical Features
Careful palpation of the Achilles tendon down to the area of insertion will allow identification of insertional tendinosis.
The tendon insertion may be warm, swollen, and tender to palpation.
If the tendon itself is neither swollen nor tender, palpating the anterior border of the tendon both medially and laterally allows identification of retrocalcaneal bursitis.
In some instances, ballottement of the bursa is appreciated.
In the case of retrocalcaneal bursitis, dorsiflexion of the foot increases the pain as it compresses the bursa between the tendon and the calcaneus.
This condition may coexist with insertional tendinosis with thickening and swelling of the Achilles tendon.
An adventitial bursa may be located between the skin and the posterior portion of the Achilles tendon rather than deep into the tendon.
The posterior heel prominence may be warm and the overlying skin may be thickened and inflamed.
The presence of a Haglund deformity can be palpated through the skin in the area of the superior portion of the heel and may be associated with overlying callus formation.
There may be an area of periostitis, which is a discrete localized area of tenderness of the calcaneus, usually on the lateral side of the posterior portion and produced by pressure from the shoe counter.
Passive dorsiflexion of the ankle should be assessed to determine whether there is an Achilles tendon contracture increasing the tension at the insertion of the Achilles tendon.
This test should be performed with the knee in extension as well as flexion and with the forefoot in both abducted and adducted positions to assess for isolated gastrocnemius tightness.
Radiologic Features
A lateral view of the foot is taken with the patient standing. This allows biomechanical evaluation of the foot as well as evaluation of the specific pointed areas of the calcaneus. The points of the calcaneus are identified as follows:
The posterior margin of the posterior facet at the superior bursal projection.
The tuberosity indicating the site of the Achilles tendon insertion.
The medial tubercle and the anterior tubercle.
The shape and appearance of the superior bursal prominence are noted.
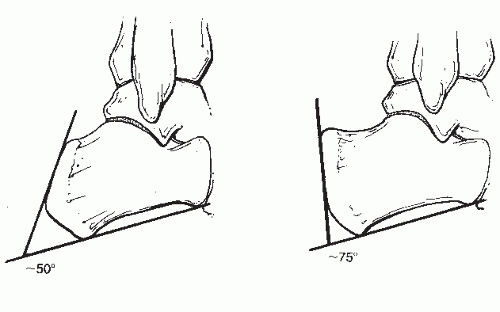
Radiographic evaluation of the lateral X-ray can include measuring the posterior calcaneal angle that is considered prominent if the angle is greater than 75°. Patients with symptomatic Haglund disease often demonstrate the combination of the posterior calcaneal angle greater than 75° and the angle of calcaneal inclination greater than 90° (Fig. 9.2). Parallel pitch line is measured by placing a line along the medial tuberosity and the anterior tubercle, and a second parallel line is drawn from the posterior lip of the talar articular facet. The bursal prominence is considered abnormal if it extends above this line. Radiographically, the syndrome is characterized by the following:
Retrocalcaneal bursitis (loss of the lucent retrocalcaneal recess between the Achilles tendon and the bursal projection).
Achilles tendinitis (an Achilles tendon measuring more than 9 mm located 2 cm above the bursal projection).
Superficial tendo-Achilles bursitis (a convexity of the soft tissues posterior to the Achilles tendon insertion).
The cortex is intact, but there is a prominent bursal projection with a positive parallel pitch line.
Some experts do not think X-ray measurements are helpful and rely more on physical examination and the patients history in clinical decision making.
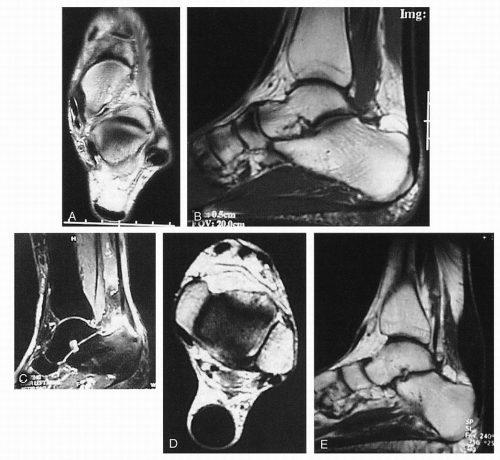
Magnetic resonance imaging (MRI) allows visualization of the Achilles tendon, the bursa, and demonstrates any bony abnormalities in the posterior superior calcaneus (Fig. 9.3). In patients refractory to nonoperative treatment, a preoperative MRI will define the anatomic structures that need to be addressed. The degree of tendinosis present in the Achilles tendon is easily visualized and distinguished from isolated bursitis with MRI.
Laboratory Studies
Retrocalcaneal bursitis may occasionally be a manifestation of systemic arthritis or gout. Specific laboratory studies can be obtained to rule out these disorders. Painful heel syndrome with plantar fasciitis or Achilles tendinosis has been found in patients suffering from a seronegative spondyloarthropathy, but is rare in patients with rheumatoid arthritis.
TREATMENT
Nonsurgical Treatment
Conservative management of posterior heel pain includes the following:
Modification of activity to decrease the load on the tendon.
Cross-training with elliptical or stationary bike.
Stretching activities for the gastrocsoleus complex.
Modification of shoewear to avoid direct pressure from the counter of the shoe onto the posterior aspect of the heel.
Padding of the area will often assist in relieving the pressure.
Adjustment of shoe counter material and height.
A small heel lift that decreases the pitch angle, allowing the prominent bony projection to slip forward away from the shoe counter.
Nonsteroidal anti-inflammatory drugs.
Injection of steroid in this area, if at all, should be done with great care, as this may precipitate tendon rupture.
The use of night splints to decrease morning pain and assist in improving the flexibility of the Achilles tendon.
Athletes, particularly runners, who presented with acute or chronic posterior heel pain, were successfully managed
nonoperatively by activity modification using a combination of the following:
nonoperatively by activity modification using a combination of the following:
Decrease in or cessation of the usual weekly mileage.
Temporary termination of interval training and workouts on hills.
Change from a harder bank surface to a softer surface.
Stretching and strengthening the gastrocnemius—soleus complex.
In cases where there is severe pain, significant tendinosis, or failure to respond to conservative modalities, cast immobilization can be employed. Patients can be placed into a short leg walking cast for a period of 4 to 8 weeks until the area becomes nontender to palpation. In instances where there is existing tendinosis, prolonged immobilization with the use of a molded ankle foot orthosis may allow healing over a 6- to 9-month period.
In the pediatric athlete, heel pain may result from osteochondrosis of the apophysis of the calcaneus (Sever disease) or Achilles tendinitis—characterized by pain on palpation of the tendon just above its insertion. In severe cases, there may crepitation of the tendon. Treatment includes rest and anti-inflammatory agents. In differentiating these two entities it may be helpful to note that the pain due to osteochondrosis occurs on the inferior portion of the os calcis; in Achilles tendinitis, it is proximal to the insertion of the Achilles tendon.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree