A. Definition—Intraarticular fracture of the distal end of the tibia, also known as a tibial pilon fracture, involves disruption of the distal tibial weightbearing articular surface. It represents a wide spectrum of injury severity and accounts for approximately 5% to 7% of all tibia fractures and less than 1% of all lower-extremity fractures. These injuries are distinctly different from ankle fractures. Anatomic areas injured include the weightbearing articular surface of the distal tibia (epiphysis) and the distal tibial metaphysis, as well as the distal fibula (injured in approximately 75% of cases) and, sometimes, diaphyseal extension into the tibial shaft.
B. Mechanism of Injury—Most commonly, the mechanism of injury is axial loading, but it may be rotation (shear loading) or a combination of axial loading and rotation. Axial loading injuries generally result in greater disruption of the articular surface (than rotational injuries) and commonly occur as a result of a fall from a height or a motor-vehicle accident; pure rotational injuries are lower-energy injuries that result in a lesser degree of articular cartilage disruption. (These injuries commonly occur as a result of a ski accident.) The direction of force applied to the distal tibia and the position of the foot and ankle at the time of injury determine the injury pattern.
1. Axial loading while the ankle is plantar flexed—Posterior articular comminution predominates.
2. Axial loading while the ankle is dorsiflexed—Anterior articular comminution predominates.
3. Shear forces (rotational)—Shear forces result in a wide array of injury patterns.
II. Evaluation
A. Clinical Presentation—Signs and symptoms include an inability to bear weight, marked pain, marked swelling, and evidence of soft tissue injury.
B. Physical Examination
1. Neurovascular examination—The neurovascular examination includes evaluation of the distal pulses and capillary refill, a motor examination, and a sensory examination.
2. Soft tissues
• Closed fractures—Closed fractures may be classified using the method of Tscherne.
• Open fractures—Open fractures may be classified using the method of Gustilo.
C. Imaging
1. Plain radiographs—Plain radiographs show the extent of damage to the weightbearing articular surface. Anteroposterior (AP), lateral, and mortise views of the ankle are taken. AP and lateral views of the tibial shaft are obtained to assess for diaphyseal extension. Complementary views of the opposite ankle may also be helpful for comparisons.
2. CT scanning (Fig. 12-1)
• Evaluation of the injury—CT provides further evaluation of the extent of articular disruption, including the size and location of the articular fragments, the extent of metaphyseal injury, the location and orientation of die punch articular fragments, and the orientation of the fracture lines that extend into the diaphysis.
• Preoperative planning—CT helps determine the orientation in which the hardware, including interfragmentary screws and transosseous implants of thin wire circular external fixators, should be placed. It also helps determine open surgical approaches.
3. Plain tomography
III. Injury Classifications
A. Overview—The variation in classification schemes reported in the literature makes the comparison of clinical series very difficult. The key distinctions between the various injury patterns and classifications are rotational (usually low-energy) versus axial loading (usually high-energy) mechanisms and the extent of injury of the articular surface of the distal tibia.
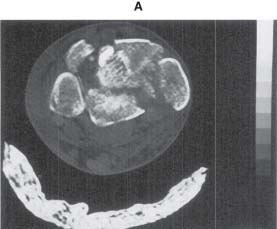
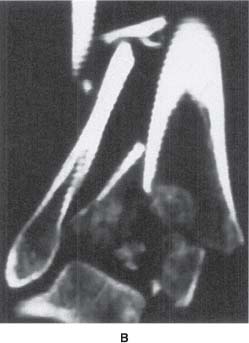
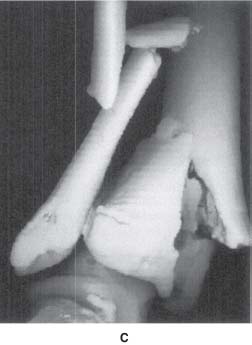
FIGURE 12-1 CT scan demonstrating a comminuted high-energy tibial plafond fracture. A. CT cross-sectional image. B. CT coronal reconstruction. C. CT three-dimensional reconstruction.
B. Specific Classifications Systems
1. Rüedi and Allgöwer (1979)—The system of Rüedi and Allgöwer (Fig. 12-2) is perhaps the most widely used classification of tibial plafond fractures reported in the literature.
• Type I—It involves a cleavage fracture of the distal tibia without major displacement of the articular surface.
• Type II—It involves significant displacement of the joint surface without comminution.
• Type III—It involves impaction and comminution of the articular surface.
2. Kellam and Waddell (1979)
• Type A—Rotational fractures consist of minimal or no cortical comminution of the tibia, two or more large tibial articular fragments, and usually a transverse or short oblique fracture of the fibula above the plafond.
• Type B—A compressive fracture pattern from axial loading demonstrates marked cortical comminution of the anterior tibia, multiple tibial fracture fragments, superior migration of the talus, and narrowing of the ankle joint seen on the X-ray film.
3. Ovadia and Beals (1986)
• Type I—It involves a nondisplaced articular fracture.
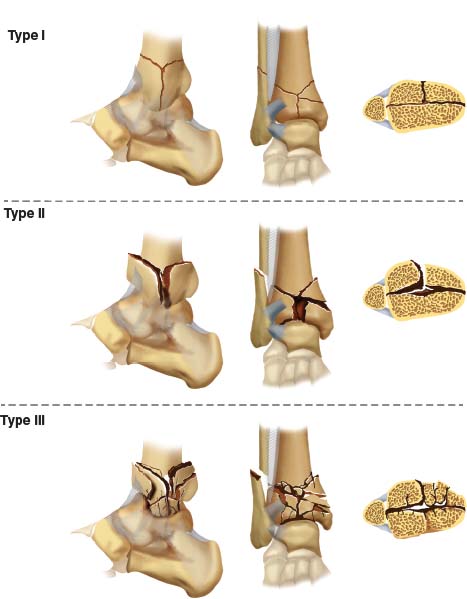
FIGURE 12-2 The Rüedi and Allgöwer classification for pilon fractures. Type I is undisplaced with splitting fracture lines. Type II has displacement of the articular surface, with split type fractures. Type III is a crush or impacted injury with comminution and displacement of the articular surface.
• Type II—It involves a minimally displaced articular fracture.
• Type III—It involves a displaced articular fracture with several large fragments.
• Type IV—It involves a displaced articular fracture with multiple fragments and a large metaphyseal defect.
• Type V—It involves a displaced articular fracture with severe comminution.
4. AO/ASIF and the Orthopaedic Trauma Association (OTA) (1996)
• Types
(a) Extra-articular (43-A)
(b) Partial articular (43-B)
(c) Complete articular (43-C)
• Groups and subgroups
(a) Metaphyseal simple (43-A1)
• Spiral (43-A1.1)
• Oblique (43-A1.2)
• Transverse (43-A1.3)
(b) Metaphyseal wedge (43-A2)
• Posterolateral impaction (43-A2.1)
• Anteromedial wedge (43-A2.2)
• Extending into diaphysis (43-A2.3)
(c) Metaphyseal complex (43-A3)
• Three intermediate fragments (43-A3.1)
• More than three intermediate fragments (43-A3.2)
• Extending into diaphysis (43-A3.3)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






