I. Evaluation
A. History—As with all extremity injuries, preliminary evaluation of fractures of the supracondylar femoral region must include an account of the mechanism of injury, assessment of comorbidities, history of prior surgery in the affected area, preinjury symptoms, and preinjury level of function. Often these patients fall into two categories:
1. The elderly or osteopenic patient with a fracture after a low-energy injury due to a fall from standing or a twisting injury.
2. The younger, healthier patient who sustains a high-energy injury due to a motor vehicle accident or a fall from a significant height.
In either case, the force is usually transmitted through a flexed knee. Additional clues as to the energy of the injury can be obtained from the physical findings and X-ray pattern. Together, this information allows the surgeon to make appropriate management decisions, look for associated injuries, and prevent complications.
B. Physical Examination—In the setting of polytrauma, initial examination includes ATLS protocol, prioritizing the ABCs (airway, breathing, and circulation). Once this assessment is complete, evaluation of the extremities is performed. Deformity in and around the knee, bruising, swelling, and open wounds should be noted. In addition, a proper neurovascular exam is critical.
1. Neurologic—Evaluation of motor and sensory function of the tibial nerve, superficial peroneal, and deep peroneal nerves should be performed, and the results documented. Often, the exam is limited by pain, level of consciousness, sedation, or neurologic injury, and this should also be documented in the patient record.
2. Vascular—Palpable pulses are a good indicator of limb perfusion. If the pulses are not palpable, then a Doppler examination should be performed. Realignment of the limb using traction and splinting can help with restoration of pulses and limb perfusion. If pulses are unequal, or not detectable on Doppler examination, an ankle–brachial index (ABI) or arteriogram should be performed. An ABI of less than 0.9 warrants further workup. If pulses are initially absent but return after manipulation of the limb, an arteriogram should strongly be considered to rule out an intimal tear that could lead to thrombosis.
3. Soft tissues—Initial evaluation should include documentation of open wounds. Attention should be paid to the posterior aspect of the limb to make certain that wounds on the back of the leg are not missed. Patients with open fractures should receive antibiotic coverage for gram-positive organisms. Grossly contaminated wounds should also receive gram-negative coverage. Wounds contaminated with dirt should receive anaerobic coverage as well.
4. Compartment syndrome—Compartment Syndrome should be ruled out in all patients with extremity injuries. Special attention should be paid to the polytrauma patient who may have distracting injuries or is sedated. If the clinical exam is suggestive of compartment syndrome, fasciotomies should be performed. If the patient is not examinable, compartment pressure measurements should be performed. If the patient undergoes a revascularization procedure, prophylactic fasciotomies should be performed to account for edema associated with reperfusion injury.
5. Associated injuries—Particularly in the setting of polytrauma, associated injuries should be ruled out. Often, these are not obvious on the secondary survey and must be evaluated on tertiary survey or on exam under anesthesia in the operating room. Musculoskeletal injuries commonly seen in the ipsilateral limb include tibial shaft fractures (floating knee), femoral neck fractures or hip dislocations, patella fractures, and ligamentous knee injuries or dislocations. Falls from significant height may also result in calcaneus or pilon fractures, or fractures of the pelvis, acetabulum, or spine.
C. Radiographs
1. AP and lateral X-ray images of the hip, femur, and knee should be obtained. X-rays should be scrutinized for intra-articular fractures, and Hoffa fragments (Fig. 7-1).
2. More comminuted fractures and those with extension into the diaphysis are often the result of higher-energy mechanisms of injury and should prompt the surgeon to look for other associated injuries.
3. Intrarticular fractures should be imaged with CT scan. This is more valuable if provisional realignment has been performed with traction and splinting, or external fixation.

FIGURE 7-1 Sagittal cut from a CT scan of the distal femur demonstrates the fracture of the posterior condyle of the femur (Hoffa fragment). This fracture line is easily missed on plain X-rays.
4. If a ligamentous knee injury or dislocation is suspected, an MRI should be considered prior to instrumentation and after consultation with a specialist.
5. If a vascular injury is suspected—Often in association with a knee dislocation—A CT angiogram should be performed.
D. Classification—Orthopaedic Trauma Association Classification (Fig. 7-2)
II. Initial Management
A. Reduction using traction and splinting is usually sufficient for temporary stabilization of isolated supracondylar femur fractures. Skeletal traction is usually not necessary.
B. External fixation spanning the knee is indicated when definitive fixation is delayed due to soft tissue injury or wound contamination, and in the setting of a vascular repair. Ideally, external fixation should be converted to definitive internal fixation within 2 weeks to decrease the infection risk secondary to pin track colonization.
III. Definitive Treatment
A. Principles of ORIF
The goal of open reduction and internal fixation is to restore anatomic alignment of the limb while providing a stable environment for healing and sufficient stability to allow for early range of motion. This is accomplished by following these steps:
1. Anatomic reduction of the articular surface—In fractures with intra-articular extension, the first goal should be to restore articular congruity. This is best achieved using interfragmentary screws. Cancellous, and sometimes cortical screws, ranging from 3.5 to 6.5 mm are commonly used. Smaller screws (2.0 to 3.0 mm) should also be available for fixation of smaller fragments in the setting of fracture comminution. Care must be taken to keep the starting point and trajectory of these screws from interfering with a subsequent intramedullary nail, or plate and screw positioning. One must consider the three-dimensional structure of the distal femur to avoid violation of the notch anteriorly and also the fossa posteriorly. Prominent screw penetration medially may also lead to irritation of the soft tissues along the medial condyle.
2. Restoration of mechanical axis—Realignment of the axis of the femur can be achieved with the use of plates and screws, or an intramedullary implant such as a supracondylar nail. In the setting of intra-articular fractures, a plate-and-screw construct is often preferred to avoid displacing the articular reduction or fixation. Ultimately, implant selection depends on surgeon experience and preference.
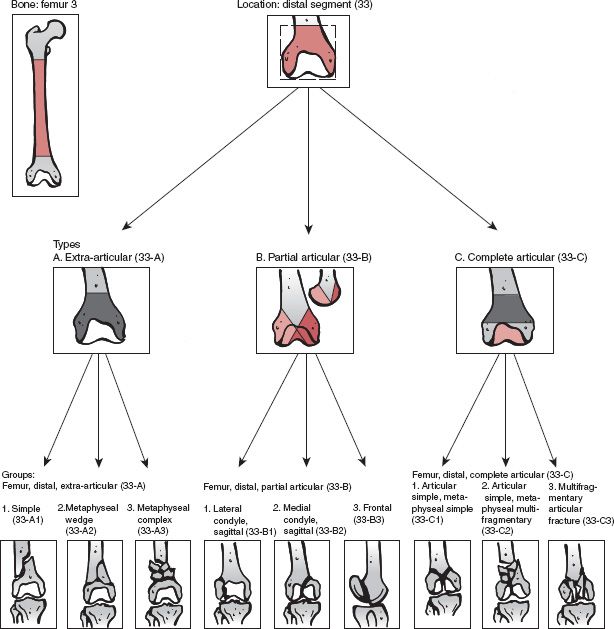
FIGURE 7-2 The Orthopaedic Trauma Association classification of distal femur fractures. The alphanumeric code used to classify these fractures is made up of a number for the bone segment—in this case 33 (for femur, distal)—followed by a letter to describe the general type of fracture. Fractures classified as 33-A are extra-articular fractures in the metadiaphyseal region. 33-B refers to partial articular fractures, where at least one portion of the articular surface is in continuity with the diaphysis. 33-C fractures are complete articular fractures, where no part of the articular surface remains in continuity with the diaphysis. More extensive classification is possible, with subdivision into groups. (From Collinge CA, Wiss DA. Distal femur fractures. In: Bucholz RW, Court-Brown CM, Heckman, JD, et al, eds. Rockwood and Green’s Fractures in Adults. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2010, with permission.)
B. ORIF with Plate Fixation
Fixed angle plates provide excellent fixation for maintaining reduction, but this comes at the expense of the soft-tissue envelope, as greater dissection is required for insertion.
1. Plate fixation is usually achieved from the lateral side. In simple fracture patterns, this is sufficient, as stability of the medial column of the femur is provided by restoration of bony alignment and contact. In comminuted fractures, no stability is provided by restoration of bony alignment alone.
2. Locking plates now play an important role in the management of these types of fractures. Their fixed angle construct has allowed for stable fixation of fractures in the setting of comminution, avoiding the need for additional medial plates, and with easier insertion than older fixed-angle devices (Fig. 7-3).
3. The development of minimally invasive plate osteosynthesis (MIPO) techniques have also been helped by the design of these plates, which are very amenable to MIPO insertion.



FIGURE 7-3 A. AP and lateral X-ray of a supracondylar fracture stabilized with a 95° blade plate. B.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






