A. Overview
1. Function of the scapula—The scapula plays an important role in the mechanics of the shoulder girdle. It has 18 muscular attachments, which link the axial skeleton to the appendicular skeleton. Dyskinesis can lead to painful upper extremity use and if not treated, can be chronic in nature. The scapula is important for rotator cuff function, which is translated to upper extremity motion. It has several articulations, including the scapulothoracic, acromioclavicular, and glenohumeral joints.
2. Frequency of injury—Fractures to the scapula are rare and account for 0.5% to 1.0% of all fractures and 3% to 5% of shoulder girdle injuries.
3. Biomechanics—Shoulder elevation is composed of glenohumeral motion (120°) and scapulothoracic motion (60°). The scapula is the foundation for all complex upper extremity motions with its multiple muscle attachments. It acts as a fulcrum for the deltoid while allowing the rotator cuff muscles to keep the humeral head centered in the glenoid during abduction. The coracoid maintains vertical stability through soft-tissue attachments with the clavicle and muscles of the chest and arm. The acromioclavicular joint allows for horizontal and vertical stability.
B. Mechanism of Injury
1. Injury may occur from a direct blow to the scapula or with force acting through the humerus. As a general rule, scapular injuries require high-energy trauma and when seen should raise suspicion for other associated injuries including rib fractures, hemo/pneumothorax, pulmonary contusion, brachial plexus injury, cervical spine fracture, clavicle fracture, and arterial injury.
C. Imaging
1. Orthogonal—High-quality orthogonal views are the most helpful when evaluating scapular fractures. The AP scapula and transscapular Y view are the most helpful.
2. Computed tomography (CT) scans—CT scans, particularly with three-dimensional reconstructions, may aid in diagnosis, and help with preoperative planning of periarticular and articular fractures.
3. Stryker view—If a coracoid fracture is suspected, a 45° cephalic tilt view (Stryker view) is useful. If soft-tissue injury is diagnosed, an MRI may be useful.
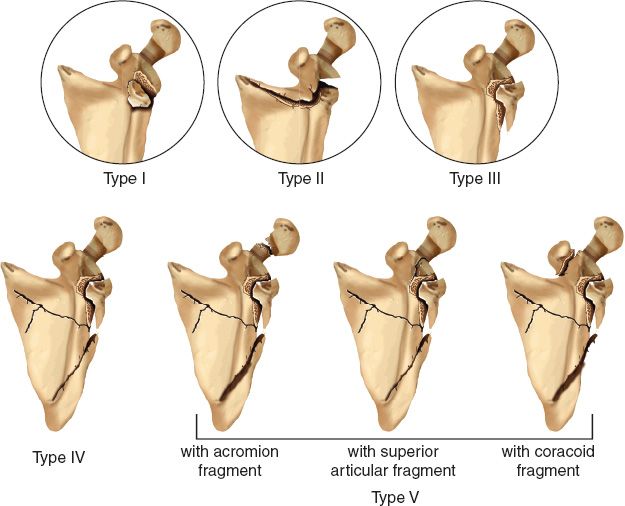
D. Classification (Fig. 18-1)
1. Mayo
• Type I—Involvement of the anteroinferior glenoid; the injury may be associated with complete dislocation or subluxation of the humeral head. The scapular body is intact.
• Type II—Involvement of the superior third to half of the glenoid; the superior fragment contains the intact coracoid. The scapular body is intact.
FIGURE 18-1 Mayo’s modification of the Ideberg classification of intraarticular fractures of the glenoid distinguishes five types. The figure shows Types I through IV and three variants of Type V. Type V is a Type IV pattern plus an additional coracoid, acromion, or free superior articular fragment.
• Type III—Involvement of the inferior or inferoposterior glenoid; the injury includes the lateral scapular border. The scapular body is intact.
• Type IV—Involvement of the inferior glenoid with extension into the scapular body.
• Type V—Type IV with the addition of a coracoid, acromion, or free superior articular fragment.
E. Treatment
1. Types
• Nonoperative—Indications include scapular body fractures and periarticular/articular fractures with only minimal displacement. These will generally heal well without complications.
• Surgical—Indications include displaced glenoid fossa fractures and fracture-dislocations, glenoid neck fractures with displacement, coracoid and acromion fractures with displacement, and ipsilateral fractures of the clavicle and glenoid neck or a fracture of the glenoid neck associated with disruption of the soft tissues attaching the clavicle to the scapula.
2. Scapular body fractures—Although scapulothoracic motion is important in preservation of normal motion, scapular body fractures do well with nonsurgical management. Almost all of these fractures heal due to the abundant blood supply and musculature covering the surface of the scapula. If dyskinesis exists, it typically responds to therapy. If the fracture extends into the scapular spine and displacement is greater than 5 mm, open reduction and internal fixation (ORIF) is recommended. Be aware that these are typically high-energy injuries and are associated with a high incidence of life-threatening injuries, including scapulothoracic dissociation.
3. Acromion fractures—Any significant displacement of the acromion warrants ORIF. Acromionectomy should be avoided as this may lead to deltoid weakness and loss of function as the tension is lost across the glenohumeral joint. If the injury was transmitted through the humerus, a rotator cuff tear should be suspected and treated simultaneously.
4. Coracoid fractures—Coracoid fractures occur most commonly through the base and are best visualized with the Stryker view (45° cephalad tilt). Because it serves as an important attachment for the arm flexors and coracoacromial ligaments, displacement of greater than 1 cm requires ORIF. If displacement is less, analgesics with a simple arm sling is indicated with return to motion at approximately 6 weeks if the pain has subsided. If an associated AC separation exists, this should be fixed in conjunction.
5. Glenoid neck fractures—Isolated glenoid neck fractures with less than 1 cm of displacement can be treated conservatively. Because the AC joint and clavicle are spared, the glenoid will heal in the position of original displacement. Surgical indications include more than 1 cm of displacement of the glenoid, more than 40° of rotation of the glenoid, and a floating shoulder. If displacement of greater than 1 cm is left untreated, abductor weakness can persist, and the patient may end up with pseudoparalysis. With a floating shoulder, the weight of the extremity will most likely lead to further displacement; therefore, surgical treatment is recommended.
6. Glenoid fossa fractures—Glenoid fossa fractures require ORIF if greater than 25% of the anterior glenoid surface is fractured, if more than one-third of the posterior glenoid surface is fractured, if any subluxation of the humeral head exists, or if there is more than 5 mm displacement of the articular surface (in any of these instances are treated nonoperatively, a poor outcome is likely). Good to excellent results with surgical intervention are obtained in 80% of cases. Poor outcomes are related to iatragenic nerve palsies. The goal of surgery is anatomic restoration of the articular surface.
F. Surgical Approaches
1. Anterior deltopectoral approach—This approach is used for Mayo Types I and II injuries.
2. Posterior Judet approach—This approach uses the internervous plane between the infraspinatus and the teres minor. The deltoid is released from the posterior acromion and retracted laterally giving a view of the posterior glenoid and lateral scapula. A posterior arthrotomy may be made to inspect the joint. The suprascapular nerve branch to the infraspinatus, which exits the spinoglenoid notch, is at risk during this exposure and should be identified and protected. Mayo Types III to V injuries are typically treated using this approach; however, some fractures may require a combined approach.
II. Scapulothoracic Dissociation
A. Description—A scapulothoracic dissociation is a rare entity caused by high-energy trauma.
B. Mechanism—The mechanism of injury is most likely a traction injury caused by a blunt force to the shoulder girdle, which leads to a complete, traumatic dissociation of the scapulothoracic articulation the shoulder girdle, which leads to a complete, traumatic dissociation of the scapulothoracic articulation.
C. Clinical Presentation—The skin is typically intact, and there is massive soft-tissue swelling, which is caused by an avulsion of the deltoid, pectoralis minor, rhomboids, levator scapulae, trapezius, and latissimus dorsi muscles, as well as a fracture of the clavicle, AC dislocation, or SC dislocation. Scapulothoracic dissociation is typically accompanied by a severe neurovascular insult. The subclavian artery and vein are usually torn, and the axillary artery and brachial artery are at risk as well. The neurologic deficit is most often the result of a complete avulsion of the brachial plexus. An incomplete neuropraxia is possible and cannot be excluded.
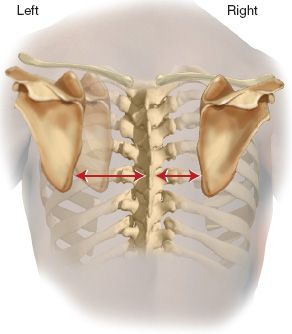
D. Radiographic Findings (Fig. 18-2)—Diagnosis is based on a clinical and radiologic exam. The upper extremity is often flail and pulseless. The shoulder girdle exhibits massive soft-tissue swelling. The chest X-ray will show lateral displacement (measured as more than 50%) of the affected scapula. The measurement may be performed as the distance from the sternal notch to the glenoid fossa or more commonly from the inferior angle of the scapula to the midline. Close scrutiny of the chest X-ray must be performed to ensure that the image it is not rotated. Often there will be an associated clavicle fracture, AC dislocation, or SC dislocation.
E. Treatment—Initial resuscitation should be followed by an emergent angiography if a pulseless extremity is diagnosed. Rapid evaluation by a vascular surgeon is necessary and emergent surgical repair is required in the unstable patient. Following vascular repair, the clavicle and AC/SC joints should be surgically stabilized. Exploration of the brachial plexus, and cervical myelography should be done to determine the prognosis of the upper extremity. If a complete avulsion of the brachial plexus is found, a primary above-elbow amputation with early prosthetic fitting should be considered, as functional recovery is unlikely. Partial injuries have a fair prognosis and musculotendinous transfers may be performed at a later time.
FIGURE 18-2 Scapulothoracic dissociation demonstrating lateral displacement (of at least 50%) on the injured left side as compared with the normal right side.
III. Fractures of the Clavicle
A. Anatomy—The clavicle is the first bone to ossify (intramembranous ossification) in the fifth week of development and the last to fuse (medially). It is an S-shaped structure, which changes from a prismatic shape medially to a flattened shape laterally. It is anchored to the scapula via the AC and CC ligaments and to the trunk via the SC ligaments.
B. Function—The clavicle acts as a strut and is responsible for bracing the shoulder against motions, which would otherwise cause it to collapse. It also permits optimal muscle–tendon unit length to allow the thoracohumeral muscles to maintain optimal working distance. The clavicle acts to suspend the scapula both dynamically with an upward force from the trapezius through the CC ligaments and with a static force via the SC ligaments. It also affords protection for the closely related neurovascular structures. Biomechanically, the clavicle rotates 50° on its axis when the arm is elevated to 180°.
C. Mechanism of Injury—Approximately 87% of clavicle fractures occur as a result of a fall onto the shoulder. Another 6% fracture secondary to a direct blow, and the remainder occur via indirect injury with force being transmitted up the humerus.
D. Classification (Fig. 18-3)—Allman described the initial classification; however, it was modified by Neer, Rockwood, and later Craig. The Craig classification combines the Allman and Neer types, providing more descriptive and functional information.
1. Group I (80% of all clavicule fractures)—Fracture of the middle third
2. Group II (12% to 15% of all clavicule fractures)—Fracture of the distal third
• Type I—Minimal displacement (interligamentous)
• Type II—Displaced secondary to a fracture line medial to the CC ligaments
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree