49 Foot and Ankle Pain
Foot and ankle pain are independent risk factors for locomotor instability, impaired balance, and increased risk for falling, as well as compromised functional activities of daily living.1–5 Foot and ankle pain appear to affect approximately one in five middle-aged to older individuals. Interference with daily activities occurs in one-half to one-third of affected individuals but is rarely disabling outside the context of rheumatoid arthritis. Foot and ankle pain is significantly more common in women, a finding that has been attributed to gender-specific footwear.
Causes of Foot and Ankle Pain
The differential diagnosis of foot and ankle pain is vast and includes conditions of tendons, ligaments, muscle, bone, joints, periarticular structures, nerves, and vessels, as well as referred pain (Table 49-1).
Table 49-1 Differential Diagnosis of Foot and Ankle Pain
| Tendon, Ligament, and Muscle |
Anterior talofibular ligament tear Anterolateral impingement due to complete tear of anterior talofibular ligament and anterior inferior tibiofibular ligament Syndesmotic impingement due to tear of syndesmosis Sinus tarsi syndrome (lateral hindfoot pain and instability due to injury of contents of the sinus and tarsal tunnel) Posterior tibial tendon dysfunction Flexor hallucis longus dysfunction |
| Bone |
| Joint |
| Periarticular Structures |
| Nerves |
| Vessels |
| Referred Pain |
Courtesy Dr. George Raj, Non Surgical Spine and Joint Clinic PS, Bellingham, Wash.
Foot and ankle pain is the presenting complaint in approximately 15% to 20% of newly diagnosed rheumatoid arthritis (RA) patients.6 Further, of those patients already diagnosed with RA, the prevalence of foot and ankle involvement has been estimated to be greater than 90%.7
Diagnostic Evaluation
Physical Examination
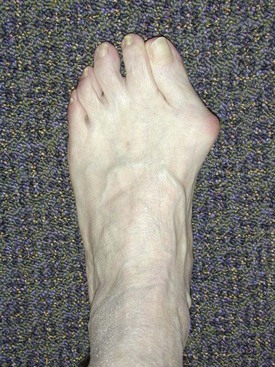
Following gait analysis, the foot and ankle are inspected, both with the patient sitting and standing. The location of swelling is usually well correlated with the joint(s) involved (e.g., ankle vs. talocalcaneal joint). Deformity should also be noted. Commonly seen deformities in patients with RA include hallux valgus, or bunion (Figure 49-1); hammertoes; and flatfoot deformity (characterized by hindfoot valgus/forefoot abduction). Callosities develop over regions of increased pressure and are associated with deformity and fat pad atrophy. Rheumatoid nodules can appear anywhere on the foot but are often found in areas of repetitive trauma (i.e., at the site of irritation from a tight shoe counter). Similarly, ulcerations appear in areas of repeated injury such as those found in tight-fitting shoes. Finally, wear patterns on shoes should also be noted. As Hoppenfeld observed8: “A deformed foot can deform any good shoe; in fact, in many cases the shoe is a literal showcase for certain disorders.”
A more detailed description of these conditions and their correlation with anatomic location is provided later in the chapter and in Table 49-2.
Table 49-2 Anatomic Characteristics of Pain in the Foot and Ankle
| Location | Dysfunction |
|---|---|
| Forefoot | |
| Midfoot | Plantar fasciitis, arthritis, synovitis (rare) |
| Hindfoot | |
| Anterior ankle | Arthritis, synovitis, impingement, osteochondral defect |
| Posterior ankle | < div class='tao-gold-member'> Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|