pronation and supination are also useful for evaluating the biceps tendon and subtle abnormalities in the radioulnar joint. Both axial and sagittal images should be obtained. When motion studies are required, we have used gradient echo (GRE) sequences (see below) and cine studies. Quick et al.13 used fast imaging steady state precession (FISP) sequence to perform motion studies of the elbow and other joints. True FISP is a steady state precession GRE sequence. The parameters used in this study include repetition time/echo time (TR/TE) of 2.2/1.1 ms, flip angle (FA) 50°, field of view (FOV) 12 to 27 cm, section thickness of 6 mm, and a 256 × 135 matrix.13
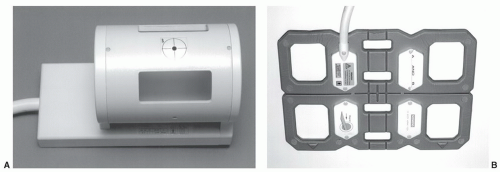
the elbow. Signal to noise ratios and spatial resolution were improved compared to conventional coil techniques.18
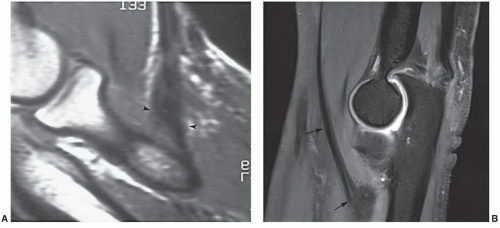
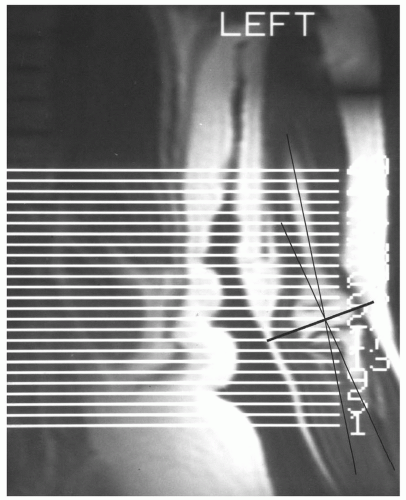
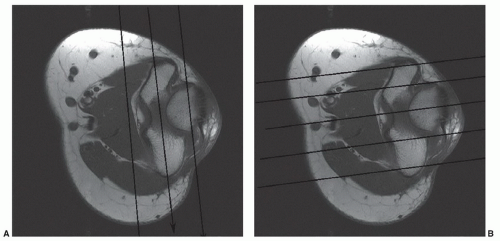
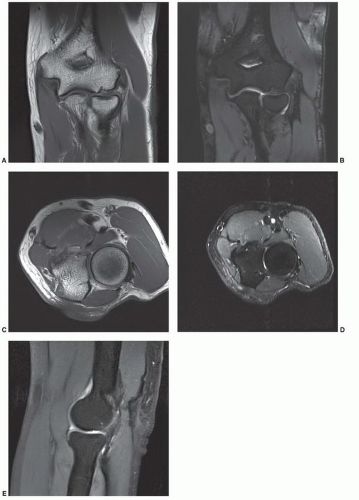
the coronal and sagittal planes (Table 10.1). We also obtain dual echo steady state (DESS) images in the coronal plane using 1-mm sections to better evaluate the articular cartilage and collateral ligaments. Coronal and sagittal images are oriented based upon the position of the epicondyles (Fig. 10.6).
Table 10.1 Routine Examination MRI of the Elbow and Forearm at 1.5 T | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
that pain, if present, is intra-articular. Following injection, fat-suppressed T1-weighted images are obtained in the axial, coronal, and sagittal planes. In addition, we obtain T2-weighted fat-suppressed FSE images in the coronal plane to better evaluate the capsule and collateral ligaments.
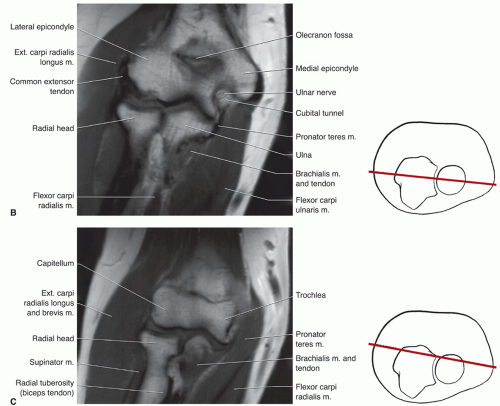
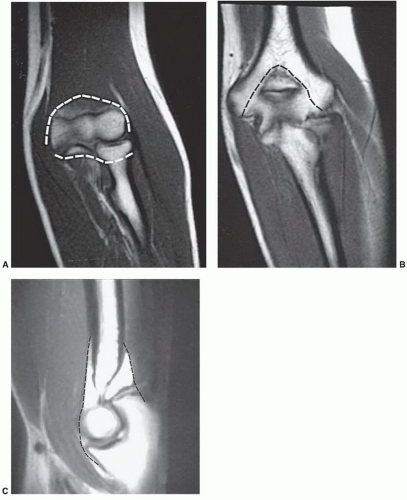
recesses are deep in the respective UCL and RCL. Synovial folds of various sizes and shapes normally project into the joint space and should not be mistaken for intra-articular loose bodies.27 These synovial folds usually occur at the junction of two synovial recesses or a triangular meniscuslike structure at the joint line margin.27
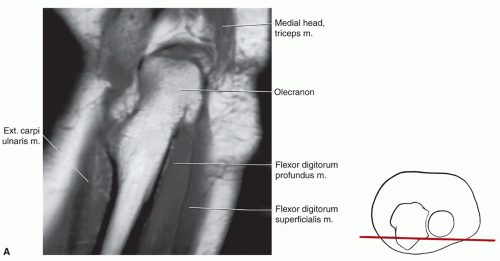
surface of the epicondyle to attach the medial edge of the coronoid process (Fig. 10.14A). The posterior band is smaller and has a fan-like configuration.25 It extends from behind the medial epicondyle and courses slightly posteriorly to attach onto the medial aspect of the olecranon (Fig. 10.14A). The transverse band is clinically less significant, small, or sometimes absent, and is often difficult to identify on MRI.2,3,30
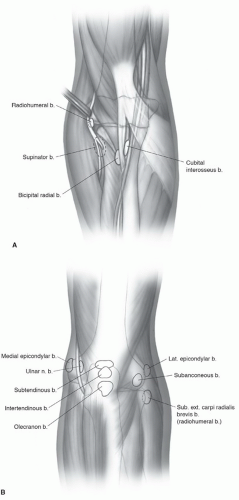
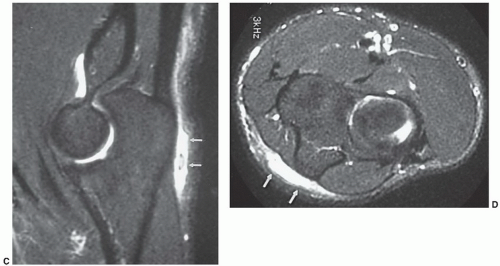
subcutaneous olecranon bursa. There are also intratendinous and subtendinous bursae in the olecranon region (Fig. 10.16) (Table 10.2).28,34 The subtendinous bursa (bicipitoradialis) is best seen on axial and sagittal MR images and should not be confused with an elbow effusion. An inflamed bursa can be differentiated from a simple effusion by the lack of fluid in the anterior compartment of the elbow. The other two superficial bursae, the medial epicondylar and lateral epicondylar, should not be confused with disruptions or tears in the medial and lateral collateral ligaments. Figure 10.17 demonstrates the location of the other superficial and deep bursa in the elbow region. The relationship of these bursae to branches of the radial and ulnar nerves (Fig. 10.17) is important.27,34 These bursae are normally
not identified, but when inflamed and fluid-filled (due to trauma, infection, synovitis, or gout), they can be demonstrated on T2-weighted or GRE images.5 In this setting, the bursae will appear as homogeneous, high intensity structures with clearly defined margins.1,2
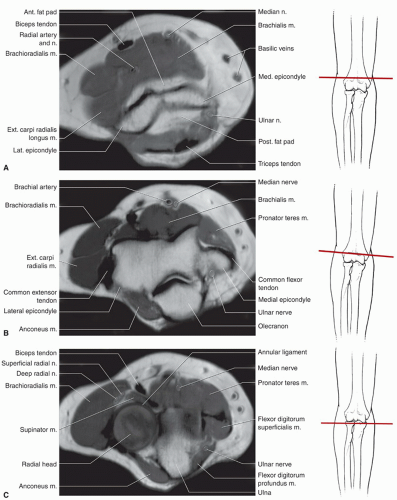
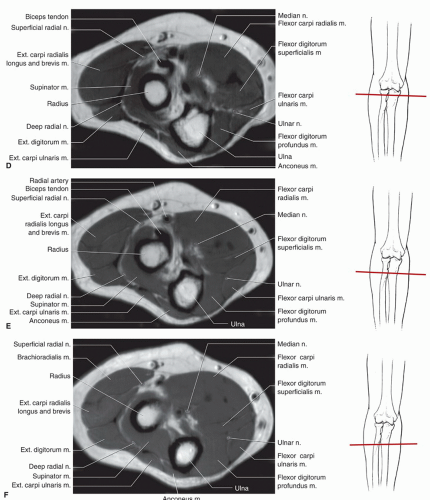
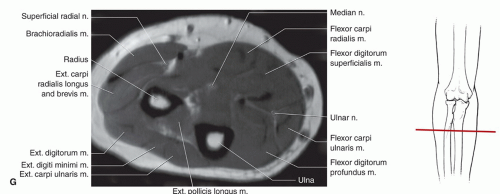
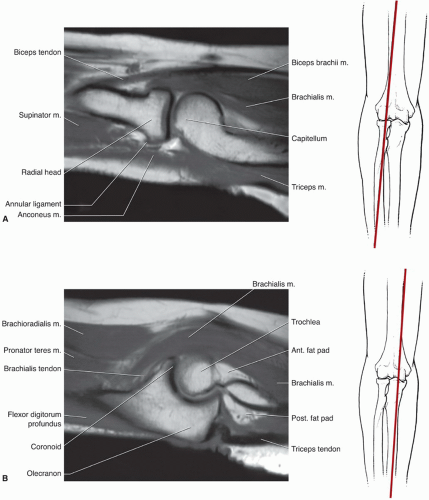
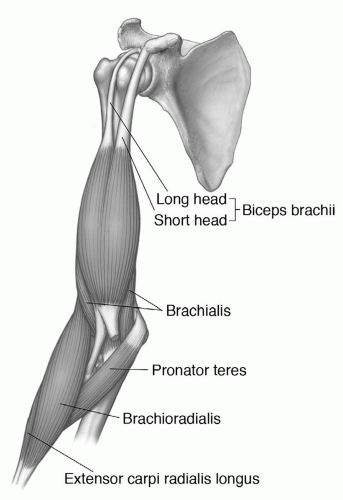
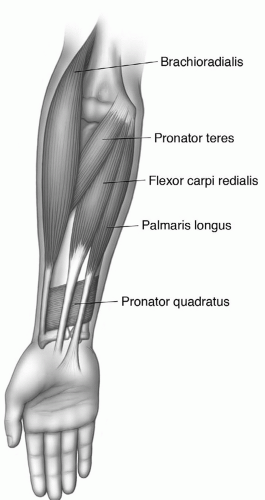
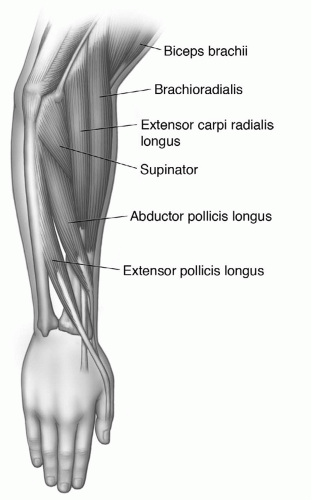
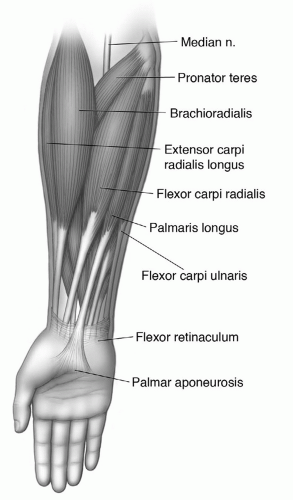
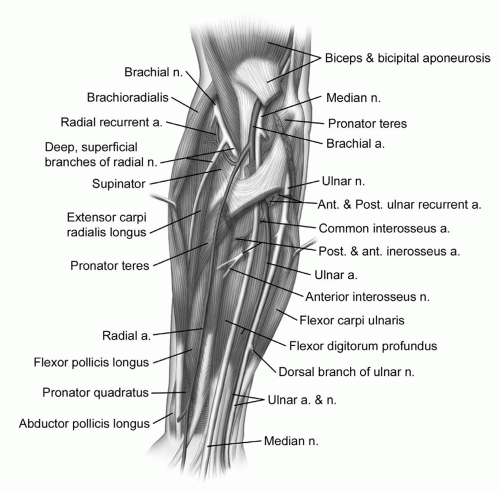
brachioradialis (Figs. 10.8, 10.10, and 10.18) (Table 10.3). The biceps brachii crosses the elbow anteriorly to insert onto the radial tubercle and serves as a supinator and flexor (Figs. 10.3, 10.8, and 10.18).27 The brachialis is a large muscle that arises from the anterior humerus and passes anterior to the elbow before inserting onto the proximal ulna near the coronoid process (Figs. 10.8, 10.9, 10.18, and 10.19). The brachioradialis arises from the radial side of the distal humerus (Fig. 10.18), crosses the lateral epicondyle, and extends distally to insert just proximal to the metaphysis of the radius (Figs. 10.8, 10.9, 10.10). In its activity as a flexor, the brachioradialis is aided by the adjacent muscles of the extensor group, especially the extensor carpi radialis longus.3,27,34 A fourth and less important flexor of the elbow is the pronator teres, which functions optimally only when the forearm is pronated. The pronator teres arises from the supracondylar
portion of the humerus, extends obliquely across the medial aspect of the elbow, and inserts onto the upper third of the radius (Figs. 10.8, 10.9, and 10.18).27,34
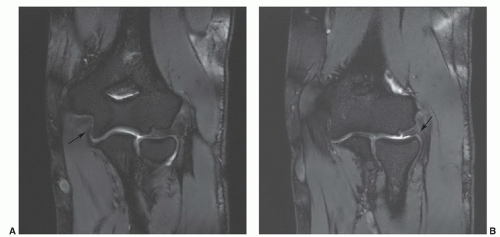 Figure 10.12 Coronal DESS images at 3.0-T demonstrating the ulnar (arrow in A) and radial (arrow in B) collateral ligaments. |
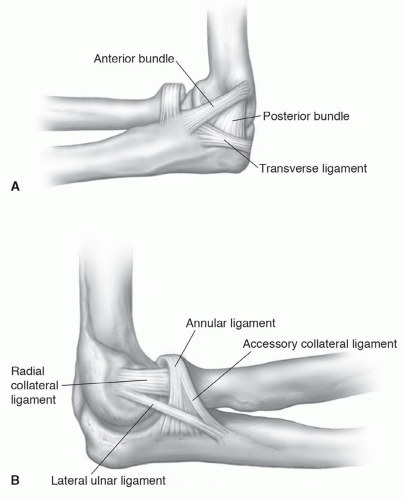 Figure 10.14 Lateral illustrations of the ligaments of the elbow from the medial (A) and lateral (B) sides. |
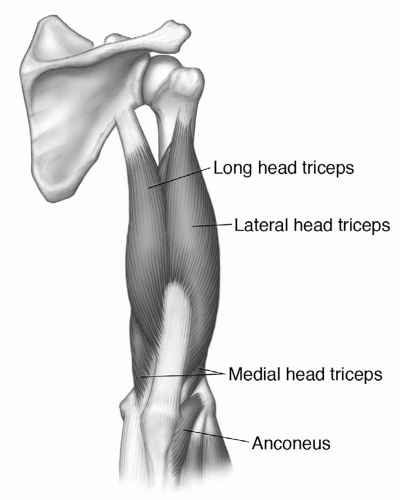
groove, and the lower posterior humerus.27,34 It inserts onto the olecranon. The anconeus (Figs. 10.8 and 10.20) arises from the posterior lateral epicondyle and extends distally and medially to insert onto the lateral ulna (Fig. 10.20).
Table 10.2 Elbow Bursae | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
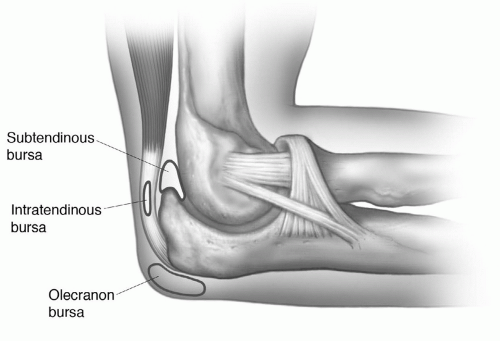 Figure 10.16 Illustration of the olecranon bursae. The superficial subcutaneous bursa is most commonly seen. The intratendinous and subtendinous bursae are less frequently identified. |
Table 10.3 Muscles of the Elbow | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
the wrist through the pisohamate and pisometacarpal ligaments to insert onto the hamate hook and fifth metacarpal base.27,29,30
Table 10.4 Muscles of the Forearm | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
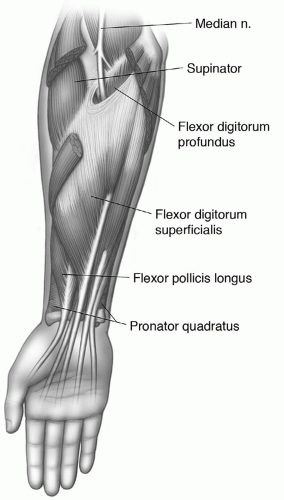
flexor retinaculum, the flexor digitorum superficialis gives off four tendons. After passing through the flexor retinaculum and carpal tunnel, these four tendons have common sheaths with the flexor digitorum profundus and split distally to insert onto either side of the bases of the second through fifth middle phalanges.27,29,30,34
 Figure 10.19 Sagittal 3.0-T fat suppressed proton density weighted image demonstrating the insertion of the brachialis muscle/tendon near the coronoid process of the ulna (arrow). |
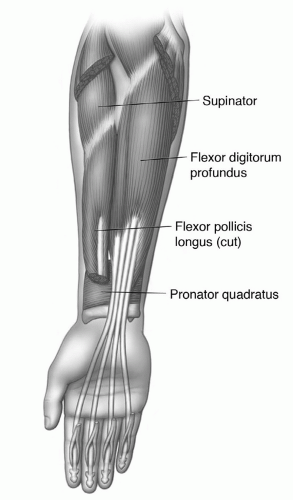
digitorum longus and flexor pollicis longus. This muscle arises from the distal ulna to insert onto the distal radius in a near-transverse direction (Fig. 10.25).27,28,29,34
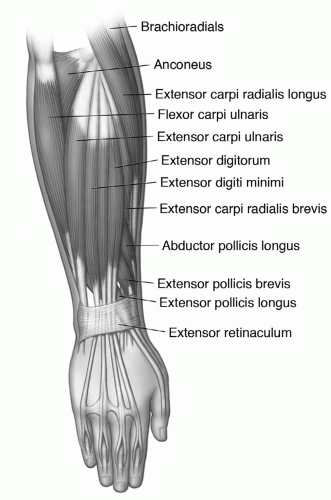
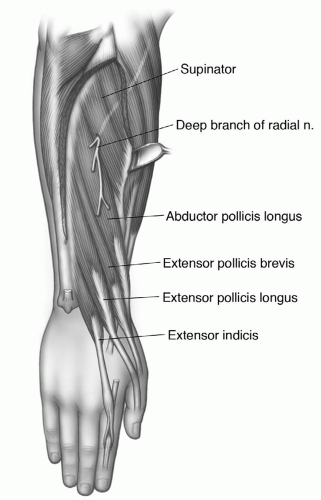
portion of the dorsal forearm. It originates from the common extensor tendon and shares an origin with the belly of the extensor digiti minimi. Distally, three to four tendons are present with a common sheath within the extensor retinaculum. The sheath is shared with the extensor digiti indicis. The tendons pass under the extensor retinaculum and receive slips from the lumbricals and interosseous muscles in the hand, thereafter dividing into central and lateral bands (see Chapter 11). The central bands insert onto the middle and lateral bands on the sides of the distal phalanges. The primary function of the extensor digitorum is to serve as an extender and abductor of the fingers. The extensor digiti minimi arises largely from a septum adjacent to the extensor digitorum and occupies a superficial position on the dorsal forearm between the extensor digitorum and extensor carpi ulnaris. The slender tendon of this muscle continues in a separate compartment under the extensor retinaculum to insert onto the dorsal aspect of the small finger in a similar fashion to the extensor digitorum. The extensor carpi ulnaris is the most medial of the superficial muscles. It has two heads, the first arising from the lateral epicondyle via the common extensor tendon, and the second from the posterior border of the ulna. The tendon of this muscle passes through a special compartment in the extensor retinaculum and also through the ulnar groove. The insertion is the medial side of the base of the fifth metacarpal. Its primary functions are wrist extension and ulnar abduction.27,29,30,34
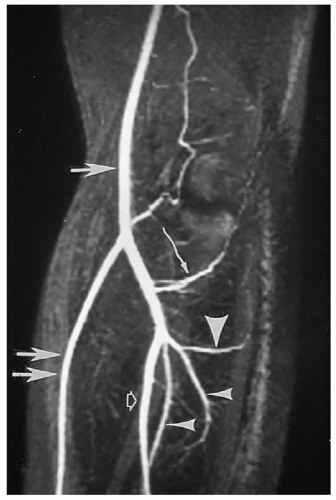
usually accompanies the median nerve along its course superficial to the flexor digitorum profundus. Figure 10.28 demonstrates the major neurovascular anatomy of the forearm and elbow.27,41 Figure 10.29 depicts the normal MR angiogram of the elbow and proximal forearm.
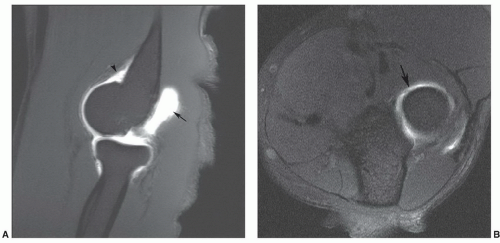
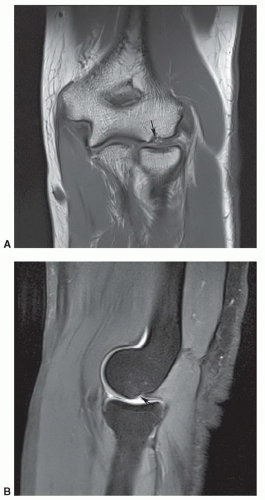
ridge in the trochlear notch that is not covered with hyaline cartilage. This finding is most easily appreciated on sagittal images and should not be mistaken for a cartilage lesion (Fig. 10.31).44
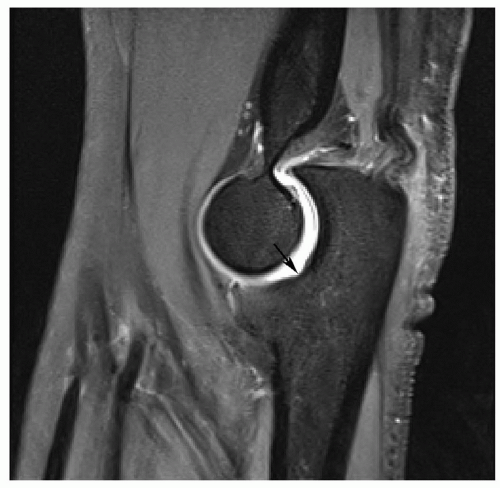 Figure 10.31 Trochlear notch. Sagittal turbo spin-echo fat-suppressed proton density image demonstrating the normal trochlear notch (arrow). |
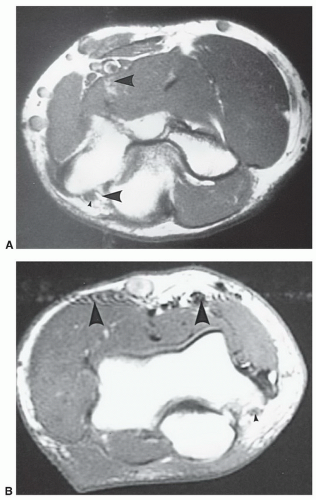
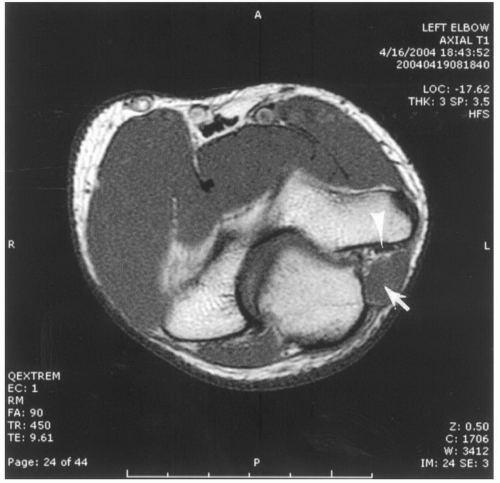 Figure 10.32 Axial T1-weighted image of the elbow demonstrates an anconeus epitrochlearis (arrow) compressing the ulnar nerve (arrowhead). |
however, it is still useful to change the phase encoding direction to prevent artifacts from degrading important areas on the image (Fig. 10.33).1,2,53
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree