CHAPTER 17 Disorders of the Proximal Biceps Tendon
ANATOMY
The LHB arises from the glenoid labrum and supraglenoid tubercle. It is an intra-articular but extrasynovial structure that is essentially static within the joint, sliding passively on the humeral head during elevation or rotation.1 The tendon is approximately 9 cm long and 5 to 6 mm in diameter, and the articular portion is flatter and a little larger than the groove portion.
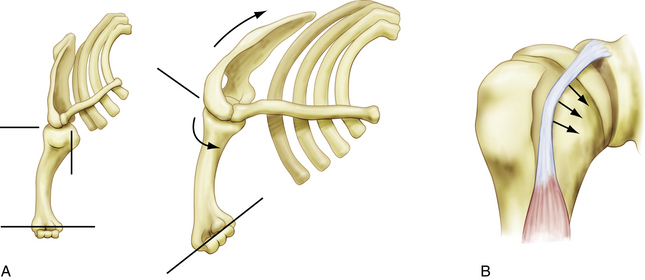
The location of the LHB just anterior to the supraspinatus tendon makes it susceptible to subacromial impingement. In addition, under load, the LHB often bears on the medial aspect of the groove, with the lesser tuberosity and soft tissues acting as a pulley (Fig. 17-1). This renders the tendon highly vulnerable to mechanical attrition and, if the soft tissue restraints of the biceps pulley become incompetent, subluxation.3
The contributions of the superior glenohumeral ligament and coracohumeral ligament to the biceps pulley mechanism are critical to the stability of the tendon. The transverse humeral ligament is not a significant stabilizer at the entry of the groove, and doubt has been expressed about its existence as a distinct entity, because it may be a continuation of the insertion of the subscapularis.4 Posteriorly, the leading edge of the supraspinatus is the primary restraint, although the anterior location of the groove and anterior vector of the pull of the tendon make this less important in most functional positions.
The function of the LHB at the shoulder is still a matter of debate. Some authors have considered it a purely vestigial structure with no true function at the glenohumeral joint, viewing it as the appendix of the shoulder. It functions as a weak abductor of the shoulder, but only when the arm is in external rotation, a position that is rarely used in activities of daily living.4,5 It has also been proposed as a depressor of the humeral head and, although some cadaver, biomechanical, and radiologic studies have supported this,6,7 electromyographic studies,8,9 clinical observation, and the long-term results of tenotomy in the presence of a rotator cuff tear10 appear to negate this role. The primary function of the biceps is at the elbow, where it acts as a flexor and supinator.
There has been recent interest in the role of the LHB in glenohumeral stability, especially following the description of superior labrum anteroposterior (SLAP) lesions,6,11–13 and mostly in the context of the throwing athlete.14,15 Anterior instability leads to increased activity in the muscle on electromyography, indicating the possible role of the biceps as a secondary glenohumeral stabilizer. However, the magnitude of this function is likely to be small.
PATHOANATOMY
Tenosynovitis, tendinosis, delamination, prerupture, and rupture probably represent the natural history of progressive degeneration of the biceps. The LHB is subject to tenosynovitis because of its anatomy, with a synovial sheath and constrained path in the bicipital groove.16–18 Arthroscopic evaluation shows fluid, adhesions, and increased vascularity around the tendon, but this must not be confused with the normal vascular pattern on the superficial surface of the tendon within the groove. Early tendinosis may be difficult to visualize arthroscopically, and may be best visualized using magnetic resonance imaging (MRI) or ultrasound imaging. Often, the tendon appears macroscopically normal, although there may be some increase in diameter. As the condition progresses, fibrillation, splits, and hypertrophy or attentuation occur, and may be described as delamination or prerupture.
Most degenerative changes in the LHB are associated with pathology of the rotator cuff, as highlighted by Neer.19 The relative importance of these structures in producing symptoms is still uncertain and will probably continue to be as long as our understanding of the mechanism of pain generation in disease of the rotator cuff remains incomplete.
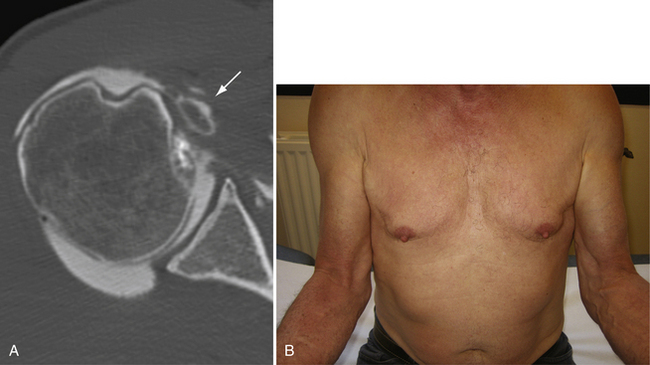
Spontaneous rupture of the LHB is usually secondary to progression of a chronic partial tear, and may happen during a movement of daily living or a minor injury. Rupture usually occurs in the presence of a cuff tear.19 The classic Popeye sign of a ruptured LHB is unmistakable, but not all rupture, or tenotomies produce this deformity.10,20 Dislocated tendons often become encased in fibrous tissue or adherent to the subscapularis before rupture, and hypertrophic tendons may become fixed within the bicipital groove, resulting in an autotenodesis. Dislocation itself may, by shortening the course of the tendon, produce a low-rising muscle belly, which we call a false Popeye sign (Fig. 17-2).
Mechanical incarceration of the tendon within the joint has been described as an hourglass biceps,21 which is often seen in association with advanced disease of the rotator cuff. The intra-articular portion becomes hypertrophic and is unable to slide into the bicipital groove, resulting in buckling of the tendon on elevation of the shoulder, with painful entrapment of the tendon between the humeral head and glenoid and a mechanical block to terminal elevation. The hypertrophic tendon may also dilate the entry to the groove and lead to subluxation.
Failure of the biceps sling leads to subluxation and eventually dislocation in the presence of a rotator cuff tear. Although the difference may be subtle, it is important to distinguish subluxation from dislocation. A subluxation is defined as a partial and/or transient loss of contact between the tendon and its groove. A dislocation is the complete and permanent loss of contact between the tendon and the groove. Dislocations of the LHB can be classified into intra-articular, intratendinous, and extra-articular subtypes, depending on its position relative to the subscapularis. In cases of subluxation and dislocation, the subscapularis is almost always torn and, most often, the supraspinatus is also torn.3 Instability of the LHB is almost always medial, but lateral instability has been described, mainly in a traumatic context in association with anterior dislocation and/or fracture of the greater tuberosity,22,23 but also in association with supraspinatus tears (see Fig. 17-2B).24
HISTORY AND PHYSICAL EXAMINATION
Spontaneous rupture of the tendon is often accompanied by retraction of the tendon and the classic Popeye deformity. With subluxation or dislocation of the tendon, the muscle belly can have the attenuated appearance of a false Popeye sign (see Fig. 17-1). A side to side comparison palpating the bicipital groove is often useful, and is felt most easily in 10 degrees of internal rotation.25 In dislocations of the LHB, the tenderness is more medial on the lesser tuberosity, and the tendon can sometimes be rolled under the fingers. We also find the Speed test (palm-up test) useful for diagnosing biceps pathology.
Patients with a dislocation of the LHB may present with a very typical clinical picture. Dislocation is often traumatic and almost always associated with a tear of the upper subscapularis. The patient presents with a loss of active elevation above 90 degrees, and it is common to find a limitation of active and passive external rotation with extra-articular and intratendinous dislocations because the dislocated biceps tendon tethers the inferior part of the subscapularis. The clinical sign of a hypertrophied and entrapped hourglass biceps is loss of the terminal 10 to 20 degrees of active and passive elevation without loss of rotation. This represents true mechanical locking of the shoulder, and should not be confused with a frozen shoulder.21
DIAGNOSTIC IMAGING
Radiographic examination should include a standard roentgenographic series (anteroposterior views in neutral, internal, and external rotation, axillary view, and supraspinatus outlet view), to rule in or out any associated abnormalities. We also find contrast studies (computed tomography [CT] arthrography, magnetic resonance [MR] arthrography) very useful to help diagnose pathology of the biceps tendon. With disruption of the medial sling, the LHB is frequently found to ride over the lesser tuberosity in a subluxated position, with a flattened appearance. With complete disruption of the sling, contrast material may escape from the biceps sheath and help outline the LHB in its dislocated position (see Fig. 17-2A).