CHAPTER 24 Suprascapular Nerve Releases
PREOPERATIVE CONSIDERATIONS
Suprascapular nerve (SSN) dysfunction is an uncommon cause of shoulder symptoms and is therefore often overlooked as a potential source of pathology. Compression of the nerve occurring at the suprascapular notch was originally described by Thomas1 in 1936 and later by Kopell and Thompson2 in 1959. However, compression at the spinoglenoid notch was not described until 1982 by Aiello and colleagues.3 Of all causes of shoulder pain, isolated SSN pathology represents just 1% to 2% of cases presenting to shoulder surgeons.4
SSN dysfunction can result from a variety of mechanisms, including direct trauma, indirect trauma (traction), space-occupying lesions (e.g., ganglion cysts, lipomas), repetitive overuse (e.g., overhead sports such as volleyball,5,6 baseball7), rotator cuff tears,8,9 and anatomic variants such as suprascapular artery passage through the suprascapular notch10 and an anomalous transverse ligament.11
Until recently, open decompression has been the mainstay of surgical treatment for this disorder, using an anterior, superior, or posterior approach.12 These approaches inevitably required some degree of muscle splitting or detachment to gain adequate exposure.13 Despite this wide dissection, the supraspinous notch is often difficult to visualize because of its close proximity to the clavicle and its deep position.
ANATOMY AND PATHOANATOMY
Anatomy
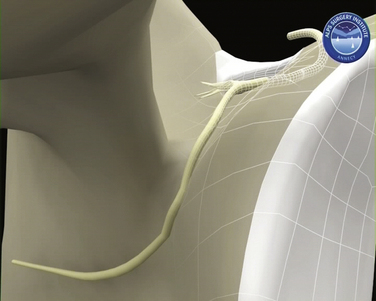
The SSN arises from the upper trunk of the brachial plexus, usually from the ventral fibers of the C5 and C6 nerve roots. The nerve then takes a course through the posterior triangle accompanied by the suprascapular artery and vein, passing inferior and parallel to the posterior belly of the omohyoid and deep to the trapezius. It enters the supraspinous fossa deep to the supraspinatus. As these neurovascular structures approach the suprascapular notch, their courses become briefly divergent so that the nerve takes a path deep to the transverse scapular ligament (TSL), whereas the artery remains superficial to this (Fig. 24-1). Variations have been reported in this arrangement, with the artery passing beneath the ligament in up to 2.5% of shoulders.10
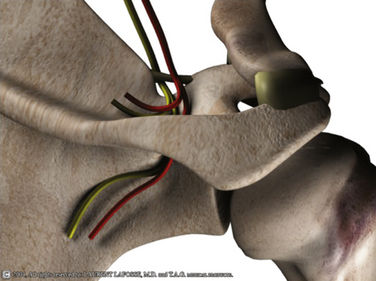
FIGURE 24-1 Three-dimensional representation of SSN and suprascapular artery and their relationship with the TSL.
The transverse scapular ligament spans the suprascapular notch, extending from the base of the coracoid and creating the suprascapular foramen. Because it is a ligament that connects two parts of the same bone, it is considered by some to represent a continuation of the coracoclavicular ligaments.10 Variable degrees of ossification have been reported in the ligament, with complete ossification in 3.7% in one series14 and partial ossification seen in 18%.15 It has also been seen to be bifid or trifid in 3% of cases in the same cadaveric series. It is important to remember, therefore, that in up to 25% of cases, the TSL is represented by an ossified variant or one with multiple bands.
As the nerve passes beneath the TSL, it gives two motor branches to supraspinatus, with the first branch generally being the larger of the two. It has been reported that one of these motor branches can pass superficial to the TSL.16 According to Hilton’s law, the SSN gives articular branches to the acromioclavicular and glenohumeral joints.10 On a microscopic level, it can be seen that the superficial part of the nerve carries afferent fibers (i.e., proprioception, pain), whereas the deeper fibers are responsible for motor innervation.17
The nerve then descends around the lateral margin of the scapular spine (Fig. 24-2) to split into three or four terminal motor branches supplying the infraspinatus. In doing so, it passes beneath the spinoglenoid ligament, forming the soft tissue boundary of the spinoglenoid notch. This quadrangular ligament extends from the posterior glenoid neck and capsule to insert onto the scapular spine.18
A cutaneous branch has been found in 14.7% of cadaveric specimens examined, which supplies the skin overlying the proximal lateral third of the arm.17,19 These cutaneous and articular branches may in part explain the nature and location of pain in some patients with SSN dysfunction.
Pathoanatomy
Rengachary and associates20 have described six different types of suprascapular notches of varying depths and profiles, ranging from a wide depression on the superior border of the scapula to complete osseous enclosure. The morphology of these notches may predispose some patients to developing SSN pathology by virtue of having a narrower and therefore more constrictive notch, or one that is entirely osseous. They also offered a second mechanism to explain local nerve trauma through the principle of the sling effect. They proposed that this is caused by the change in angulation of the nerve as it passes through the foramen, especially with the arm in hyperabduction or depression combined with retraction. Kopell and Thompson2 preferred a traction friction mechanism of injury to the nerve as it passes through the notch.
Repetitive overuse is postulated to result in chronic irritation of the SSN, particularly in those who regularly engage in overhead activities.12 This is because these activities exacerbate traction on the sites of nerve fixation and expose the nerve to compressive and frictional forces on any sharp turns made by the nerve. Movements involving scapular depression and retraction, hyperabduction, or cross-arm adduction with forward flexion20,25 all place increased tension on the nerve in the notch.
Glenohumeral joint dislocations, scapular fractures, and penetrating injuries can all result in direct or indirect traumatic injuries to the SSN. Iatrogenic injuries have been reported in surgery for distal clavicle resection, shoulder stabilization, and positioning of spinal patients for procedures.12
HISTORY AND PHYSICAL EXAMINATION
The principal complaint is usually one of deep diffuse pain or aching, often localized posteriorly or laterally in the proximal arm. Some have described this pain as burning in nature, which can radiate down the arm or into the neck. The onset of symptoms is usually insidious in nature, however, if trauma has been a precipitating feature; the cause is commonly compression at the level of the TSL.4 Patients also complain of weakness, particularly in movements involving external rotation and abduction and their symptoms are typically exacerbated with overhead activities. However, all these symptoms can be difficult to differentiate from those of rotator cuff tears or impingement, which may be coexistent. As such, pathology related to the SSN continues to be underdiagnosed. Symptoms from nerve compression at the suprascapular notch tend to be more severe than those compressive causes occurring distally.26 Because of the poorly defined nature of the symptoms, patients frequently present many months after symptoms have begun and, in many cases, after having had previous surgery. These patients remain troubled by persistent symptoms; by this stage, their pain has become chronic and muscle atrophy has become apparent. One of the most important aspects in the management of SSN neuropathy is to detect it early to prevent it reaching this late stage.
Clinical examination reveals only a subtle loss of external rotation and abduction strength in the early stages of compression. Atrophy is seen later in the course of the disorder; it affects the supraspinatus and infraspinatus in cases of proximal nerve entrapment at the suprascapular notch, although in some cases isolated infraspinatus wasting is seen with proximal compression.4 Nerve compression at the level of the spinoglenoid notch causes only infraspinatus atrophy. Tenderness may found in the suprascapular notch, but this is a relatively nonspecific sign. Long-standing compression can cause profound weakness in external rotation and abduction, with marked muscle atrophy, although deltoid mass should be reasonably maintained (Fig. 24-3).
DIAGNOSTIC IMAGING
Magnetic resonance imaging (MRI) remains the best imaging tool in suspected SSN pathology because of its soft tissue resolution. It can be used to visualize the course of the nerve and integrity of the rotator cuff, demonstrate the presence of fatty infiltration, and is very helpful for identifying space-occupying lesions. The presence of muscle edema on MRI scanning has been suggested as a more sensitive and specific early sign of SSN entrapment than that of muscle atrophy and fatty infiltration.27 Caution should be exercised in interpreting the clinical significance of a cyst because the presence of a cyst does not always indicate whether there is SSN compression (Fig. 24-4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree