6.1 Diseases of the skin, the eye and the ear
Chapter 6.1a The physiology of the skin, the eye and the ear
At the end of this chapter you will be able to:
Estimated time for chapter: 90 minutes.
The physiology of the skin (the integumentary system)
The functions of the skin
• Protection of the body: the skin provides a mechanical barrier that protects the deeper tissues from mechanical injury, toxins in the environment and radiation from the sun.
• Regulation of body temperature: the skin contributes to the homeostasis of body temperature by means of mechanisms including sweating in the heat and erection of body hair in the cold (goose pimples). The blood vessels in the skin also are very responsive to body temperature – they dilate in the heat and contract in the cold.
• Formation of vitamin D: the skin is the main source of vitamin D, which is essential for the maintenance of the health of the bones. Vitamin D prevents rickets and osteomalacia. It is manufactured in the skin (from a steroid precursor chemical) as a response to the action of sunlight.
• Sensation: the skin forms the boundary between the external environment and the internal environment of the body. The nerve endings in the skin are adapted to sense light, touch, deep pressure, pain and temperature. In this way the skin can communicate to the internal tissues what is going on in the outside world.
• Excretion: the skin is able to excrete unwanted substances through the sweat. It is also able to secrete aromatic chemicals, which give each person a unique smell that contributes to the non-verbal communication between individuals.
• Absorption: although this function is believed conventionally to be limited, the skin can absorb substances from the external environment. This can be interpreted as another aspect of the sensory role of the skin, allowing the body to respond to what is happening in the outside world.
The structure of the skin
The epidermis is an example of stratified squamous epithelium, whereas the thicker dermis is made up of loose (areolar) and fatty connective tissue. Figure 6.1a-I illustrates the structure of these two delicate layers of the skin and how they rest on the underlying fat. The upper part of the dermis forms folds called ‘papillae’, and it is these that give rise to characteristic skin markings such as the fingerprint. The bumpiness prevents easy separation of the epidermis and dermis.
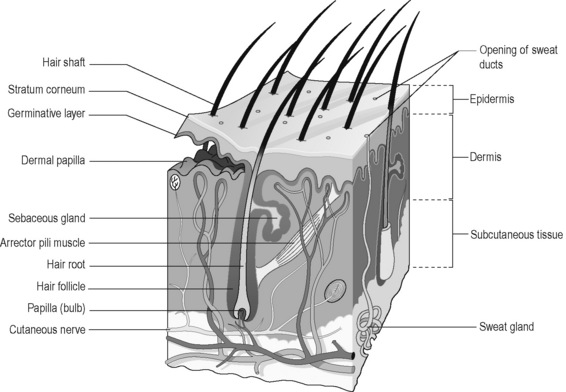
Figure 6.1a-I • A section of the skin, showing how the epidermis rests upon the dermis, which in turn rests on a layer of subcutaneous fat.
Figure 6.1a-II is a more detailed image of the stratified structure of the epidermis. The cells of the epidermis continually multiply from the germinative layer and grow upwards in layers. As they progress upwards the cells become progressively more hardened with the protein keratin. The uppermost layers, the stratum corneum and lucidum, consist of lifeless keratin-stuffed cells, which have a vital protective function. This layer thickens in response to repeated trauma, such as continually occurs to the palms of the hands and soles of the feet. As dead epithelial cells are shed from the skin they are replaced by new cells growing upwards from the germinative layer.
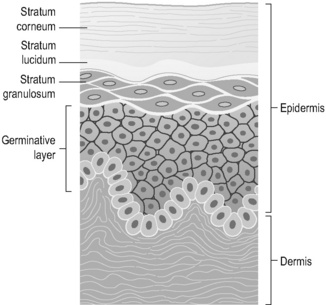
Figure 6.1a-II • The epidermis, illustrating the stratified squamous epithelial nature of this tissue.
The role of the skin in the control of temperature
The physiology of the eye
The eye and the optic nerve pathways in the brain
The eyes are sensory organs that are specialised to respond to the stimulus of light. The eyes contain the cell bodies and nerve endings of the sensory nerves known as the ‘optic nerves’ (second cranial nerves). Optic nerve fibres carry visual messages to the brain to a control centre in the thalamus. From here the information is taken further back via connector neurons to the visual areas in the occipital lobe at the back of the brain. Here the complex processing necessary for visual perception takes place. Before the optic nerve fibres reach the thalamus, some of the fibres cross to the opposite side. This crossing point, known as the ‘optic chiasm’, is adjacent to the site of the pituitary stalk (overlying the sphenoid bone of the skull). This explains why pituitary tumours often result in visual disturbance. Figure 6.1a-III illustrates the optic nerves and their pathways from the eyes, which cross before they reach the occipital lobe of the brain.
The structure of the eye
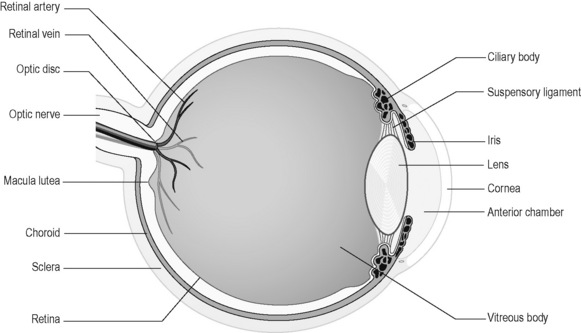
The eye has a very specialised structure that allows it to perform the function of focusing and sensing visual images. This structure is illustrated in simplified form in Figure 6.1a-IV.
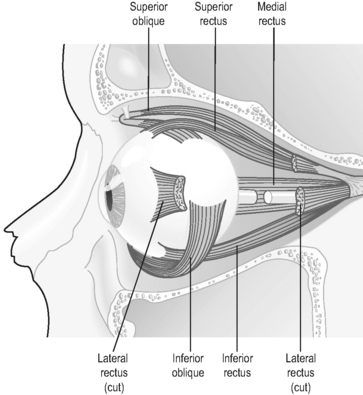
The globe of the eye sits embedded within fatty tissue in the bony orbit. The optic nerve extends from the back of each eye to pass posteriorly through the sphenoid bone towards the optic chiasm (optic nerve crossing) within the skull. Six strips of muscle extend from the walls of the orbit to attach to the sclera of each eye. These are the extrinsic or extraocular muscles of the eye. All these structures hold the eye in place (Figure 6.1a-V).
The extraocular muscles and accessory organs of the eye
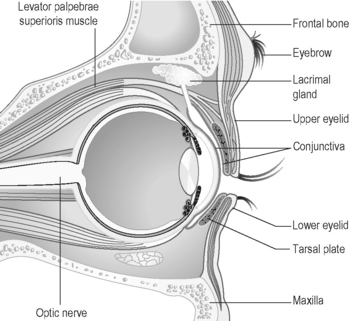
The six strips of skeletal muscle that form the extrinsic muscles of the eye guide the coordinated movements of the eyeballs (see Figure 6.1a-V). These movements, which are upwards, downwards, sideways and rotatory, are usually coordinated so that the two eyes move together. Figure 6.1a-VI illustrates the extrinsic muscles of the eye in the orbit and the muscles which control the movements of the eyelids. One of these muscles, the levator palpebrae, lifts the eyelid when it contracts, while the other muscle, orbicularis oculi, because its fibres run circularly around the eyelids, closes the eyelid when it contracts. Figure 6.1a-VI also shows how the conjunctiva forms a protective sac behind the upper and lower eyelids (see Q6.1a-12).
(see Q6.1a-12).
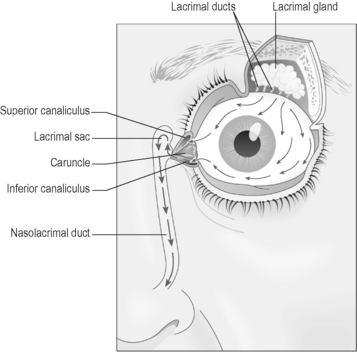
The eyebrows, eyelids and conjunctiva are adapted to provide mechanical protection for the eye. The lacrimal gland is a specialised organ for producing the tears. Tears are constantly produced by this gland (Figure 6.1a-VII) to lubricate the conjunctiva. Tears drain away via tiny channels called ‘canaliculi’ to the nasolacrimal duct (tear duct), and thence to the nose. This is why a watery discharge from the nose frequently accompanies an episode of crying (see Q6.1a-13) .
.
The physiology of the ear
The structure of the ear
The structure of the ear can be considered in three parts: the outer, or external, ear; the middle ear; and the inner ear. This structure is illustrated in Figure 6.1a-VIII.
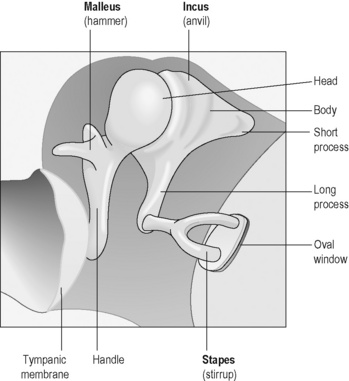
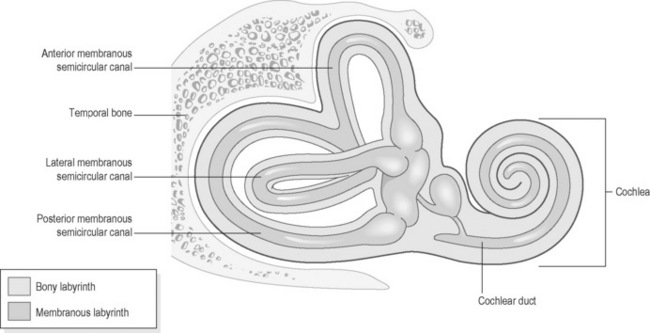
The middle ear is a chamber lined with respiratory epithelium, which contains three tiny interlinked bones (ossicles), known as the malleus (hammer), incus (anvil) and stapes (stirrup). The ossicles provide a link between the eardrum (tympanic membrane) and another membrane that separates the middle from the inner ear (the oval window). The purpose of the ossicles is to transmit the sound vibrations that strike the eardrum through to the cochlea of the inner ear. Tiny movements of the oval window lead to vibrations within the fluid (perilymph) that bathes the membranous cochlea (Figure 6.1a-IX). The largest ossicle, the malleus, can be seen through the eardrum when the eardrum is visualised by means of the hand-held otoscope (Figure 6.1a-X).
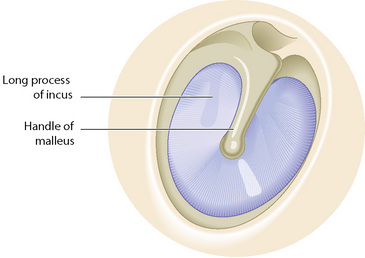
Figure 6.1a-X • Otoscopic view of the eardrum, showing the handle of the malleus and a shadow formed by the incus.
The spaces of the inner ear contain two interlinked fluid-filled membranous sacs which, like the middle ear, are safely protected, being bathed in fluid (perilymph) within bony cavities in the temporal bone of the skull. The first chamber, the cochlea, is spiral in form and contains fluid called ‘endolymph’. The cochlea is responsible for the interpretation of sound vibrations (Figure 6.1a-XI).
 Self-test 6.1a The physiology of the skin, the eye and the ear
Self-test 6.1a The physiology of the skin, the eye and the ear
1. Describe the role of the skin in:
2. What are the three layers of the eye? Describe how each of these layers is modified anteriorly to enable the eye to focus the light that enters it.
3. What are the three parts of the ear? Describe how sound waves travel through these three parts to lead to a sensory stimulus in the nerve fibres of the vestibulocochlear (auditory) nerve. Describe how a change in head position will also give rise to a sensory stimulus in the nerve fibres of this nerve.
Answers
2. The three layers of the eye are the sclera, the choroid and the retina.
The sclera forms the cornea anteriorly. This is the transparent window of the eye.
The retina is discontinued anteriorly, stopping just behind the ciliary body.
3. The three parts to the ear are the external ear, the middle ear and the inner ear.
Chapter 6.1b The investigation of the skin, the eye and the ear
At the end of this chapter you will:
Estimated time for chapter: 40 minutes.
Introduction
Investigation of disorders of the skin includes:
• a detailed inspection of the skin rash, including exposure to a Wood’s light
• culture and examination of samples taken by swab from the area of the rash
• examination of skin scrapings and nail clippings
• examination of a skin biopsy
• a physical examination to exclude underlying medical conditions
Investigation of disorders of the eye includes:
• examination of visual acuity using Snellen charts
• examination of the visual fields
• examination of colour vision
• examination of the eye movements
• examination of the structure of the eye by means of a hand-held ophthalmoscope
• examination of the structure of the eye by means of a slit lamp
• examination of the intraocular pressure by means of a slit lamp and tonometry
• examination of the blood flow to the retina using fluorescein angiography
• imaging tests, including ultrasound, computed tomography (CT) and magnetic resonance imaging (MRI)
• culture and examination of samples taken by swab from the eye.
Investigation of disorders of the ear includes:
• visual inspection of the external ear and eardrum
• clinical assessment of hearing
• testing of hearing by means of audiometry
• testing of the flexibility of the middle ear by means of impedance tympanometry
Investigation of skin disorders
Investigation of eye disorders
Investigation of ear disorders
Visual inspection of the external ear and eardrum
The external ear (the pinna), the external ear canal and the outer aspect of the eardrum can be assessed by means of a hand-held instrument called an ‘auriscope’ (or otoscope). The auriscope provides illumination of the external ear canal by means of a fibre-optic light source. The auriscope is inserted painlessly into the outer ear by means of a plastic conical ‘speculum’. The examining practitioner places gentle traction on the pinna of the ear to enable straightening of the external ear canal and so to permit visualisation of the eardrum (see Figure 6.1a-X).
Electrophysiological tests (electric response audiometry)
 Self-test 6.1b The investigation of the skin, the eye and the ear
Self-test 6.1b The investigation of the skin, the eye and the ear
1. A patient is referred to the ophthalmology department by his optician because the optician suspects that a cataract (cloudy opacity) is developing in the lens of one eye. What investigations do you think this patient might expect to undergo when he attends his appointment?
2. How do you think that a child with an onset of reduced hearing following a cold 2 months ago might be investigated? (Before you answer this question, you might wish to reread the section on glue ear in Chapter 5.4e.)
3. A patient is referred to the dermatology department with an unexplained itchy red rash affecting the palms of both hands. Describe how you think the dermatologist will investigate the rash.
Answers
1. The optician should have already tested the visual acuity in each eye by means of the Snellen chart, the visual fields by means of confrontation with a moving object, and the eye movements. Evidently, reduced visual acuity was found affecting the eye in which the optician suspects cataract formation. Ophthalmological examination will then have revealed a cloudy obscurity in the lens, which will have prevented clear visualisation of the retina.
2. In the first instance, the child is likely to be investigated by the GP or health visitor. With young children, simple distraction tests can be used to assess hearing loss. The child is distracted by means of an entertaining event while sounds are made or words whispered behind each ear in turn. A child with healthy hearing will normally turn from the entertainment to investigate the origin of the noise.
3. The most important aspect of dermatological assessment is pattern recognition. The experienced dermatologist might have a good idea of the diagnosis in this case simply by detailed inspection of the rash and its pattern of distribution.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



 (see Q.6.1a-1). The functions of the skin include:
(see Q.6.1a-1). The functions of the skin include:
 effect (see Q6.1a-5 and Q6.1a-6).
effect (see Q6.1a-5 and Q6.1a-6). Information Box 6.1a-I
Information Box 6.1a-I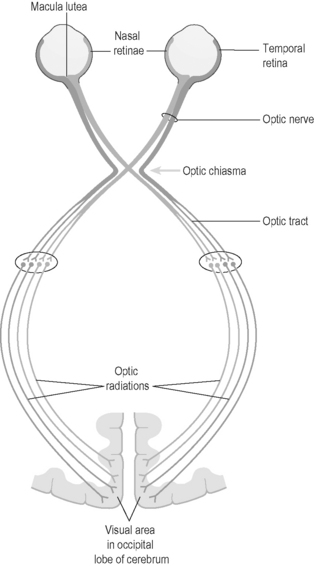
 .
. .
.
 Information Box 6.1a-II
Information Box 6.1a-II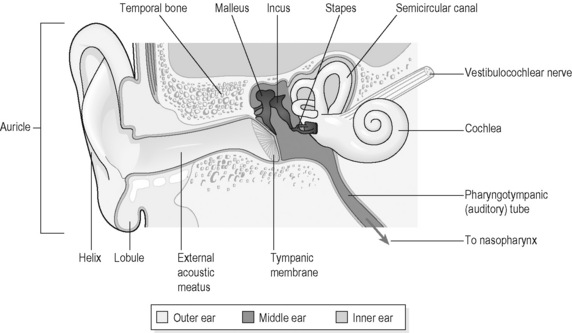
 of the head (see Q6.1a-14-Q6.1a-19).
of the head (see Q6.1a-14-Q6.1a-19). Information Box 6.1a-III
Information Box 6.1a-III