5.2 Diseases of the reproductive system
Chapter 5.2a The physiology of the reproductive system
At the end of this chapter you will:
Introduction
Section 5.2 focuses on the male reproductive system and the non-pregnant female reproductive system. The study of the male reproductive system is conventionally termed ‘andrology’, and the study of the non-pregnant female reproductive system is termed ‘gynaecology’ (derived from the Greek words for man and woman, respectively). Section 5.3 is dedicated to the conditions of pregnancy, labour and the postnatal period. The study of these conditions is conventionally referred to as ‘obstetrics’. The present chapter considers the physiology of the male and the female reproductive system in turn, and concludes with a brief discussion about the physiology of sexual intercourse.
The physiology of the male reproductive system
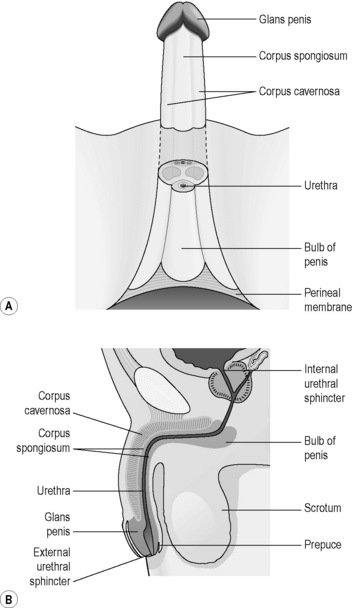
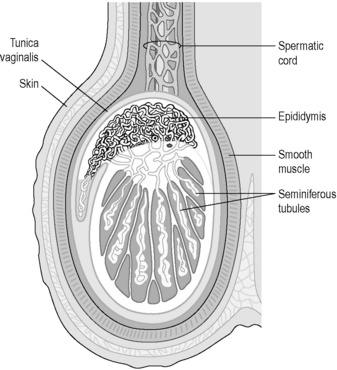
The male reproductive system consists of the testes, the epididymis, the urethra, the penis and associated glands, including the prostate gland. Figure 5.2a-I illustrates the anatomy of this system and Figure 5.2a-II shows the structure of the testis and scrotum in more detail.
The female reproductive system
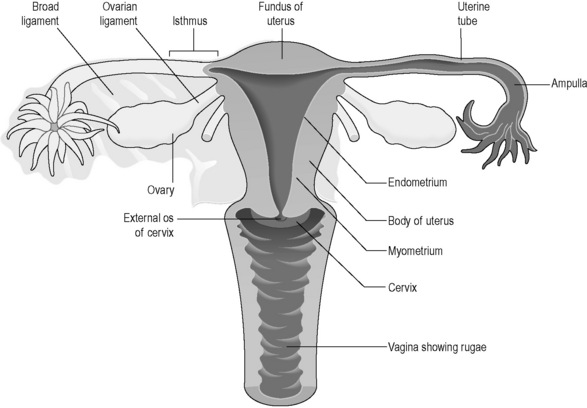
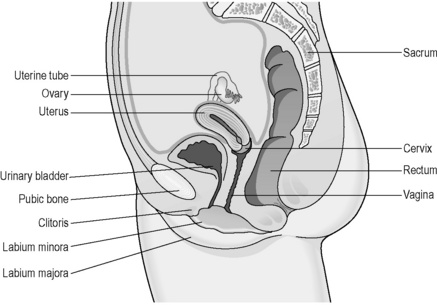
The female reproductive system lies at a deeper level in the body than in the male (Figures 5.2a-III and 5.2a-IV). The ovaries sit deep in the basin formed by the pelvis, and lie either side of the womb (uterus). The ovaries lie so that they are close to the openings of two tubes (the fallopian tubes) that extend sideways from the uterus. The uterus is a pear-sized organ sitting just behind and above the bladder, protected in front by the bridge formed by the pubic bone. The neck of the uterus (the cervix) opens into the bodily space called the ‘vagina’. The entrance of the vagina, the vulva, is surrounded by the fleshy lips of the labia minora and labia majora in the perineum.
The ovary
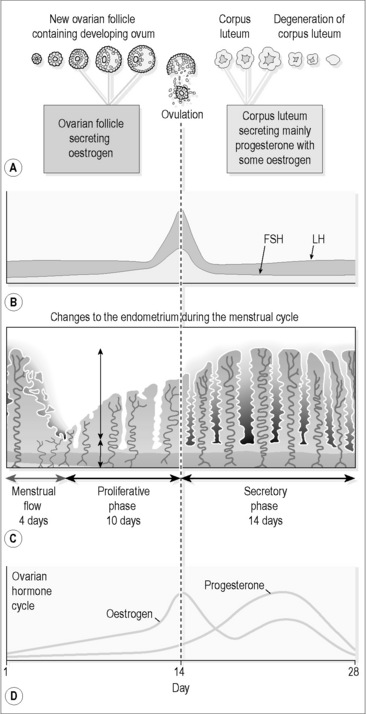
During the first half of the menstrual cycle, a single ovarian follicle begins the process of maturation (Figure 5.2a-V). This means that, over the course of approximately 14 days, the follicle enlarges and develops a fluid-filled cavity. This so called Graafian follicle then merges with the outer part of the ovary and ruptures to release the single ovum into the space surrounding the ovary. This process of rupture and release is what is termed ‘ovulation’. The whole process is stimulated firstly by FSH from the pituitary gland, and this explains its name. FSH is the same hormone that in men stimulates the development of spermatozoa from germinal cells.
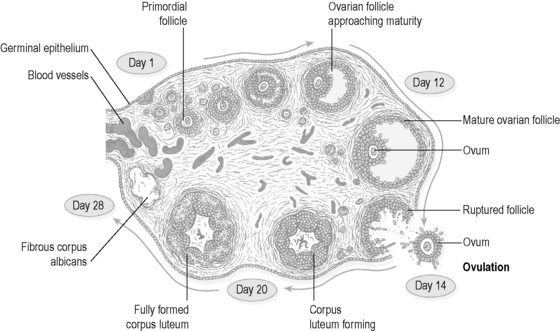
Figure 5.2a-V • Section of the ovary showing the development of one follicle over the course of one month.
The onset of puberty in the girl
Menstruation
Progesterone can be considered to be the hormone that prepares the body for pregnancy and promotes the first 3 months of pregnancy. After ovulation, the rising levels of progesterone stimulate a watery swelling of the endometrium and the production of a thick mucus. This mucus is believed to encourage the passage of the spermatozoa into the fallopian tubes, where fertilisation can take place. The changes in the endometrium provide a suitable environment for the zygote. If implantation does not occur, at about 6–8 days after ovulation the corpus luteum starts to degenerate, and progesterone levels drop. It is this drop that causes the lining of the endometrium to start to break down, culminating in menstruation at 14 days after ovulation. There are thus two distinct phases to this second half of the menstrual cycle, termed the ‘secretory phase’ and the ‘premenstrual phase’ (Figure 5.2a-VI).
The physiology of sexual intercourse
• Sexual desire: the emotional/mental response to the thought, sight, touch or smell of another person.
• Sexual arousal: following sexual desire, physical changes take place in the sex organs (genitalia). The penis and clitoris become erect and the vagina becomes lubricated. The nipples can become erect. The heart rate can increase. There is a strong desire for sexual intercourse. This phase is mediated by the parasympathetic aspect of the nervous system.
• Plateau: sexual pleasure is intensified and sustained before and after penile penetration has taken place. This phase is also mediated by the parasympathetic nervous system.
• Orgasm: orgasm usually results in ejaculation of semen in men. In penile/vaginal intercourse, the semen is directed deep into the vagina, close to the entrance of the cervical canal. 90% of women are able to achieve orgasm, although only 25% will be able to reach orgasm through penile penetration into the vagina alone. There are rhythmic contractions of the perineal muscles of the women at orgasm. These contractions encourage the upward movement of the semen towards the cervix. The orgasmic phase is mediated by the sympathetic aspect of the nervous system.
• Resolution: after orgasm, both partners are relaxed, and the body gradually returns to a non-aroused state. In this phase the parasympathetic nervous system is dominant. The resolution state encourages rest, and for the woman this is the ideal state for the continued passage of the spermatozoa into the cervical canal and thence into the uterus.
 Information Box 5.2.a-II The female reproductive system: comments from a Chinese medicine perspective
Information Box 5.2.a-II The female reproductive system: comments from a Chinese medicine perspective
• Menstruation: Blood is moving, and is reliant on smooth Liver Qi and Liver Blood.
• Postmenstrual (proliferative phase): Blood and Yin are Empty and Chong Mai and Ren Mai are Empty.
• Mid-cycle (secretory phase): Blood and Yin fill up in Chong Mai and Ren Mai.
• Premenstrual (premenstrual phase): Yang Qi rises and Liver Qi moves. This phase does not occur if implantation takes place.
 Self-test 5.2a The physiology of the reproductive system
Self-test 5.2a The physiology of the reproductive system
1. What is the composition of semen? Name the origin of its constituents.
2. What are the bodily effects of (i) testosterone and (ii) oestrogen?
3. How do the levels of oestrogen and progesterone vary throughout the menstrual cycle? What is the stimulus for menstruation?
4. What is one conventional medical reason why some women suffer more during the menopause than others?
Answers
1. Semen is composed of the male sex cells, the spermatozoa, and fluid. The spermatozoa originate from germ cells within the testes. The fluid contains nutrients for the spermatozoa, and provides an environment in which the spermatozoa can swim freely. The fluid originates from the seminal vesicles and the prostate gland.
3. Oestrogen is produced in increasing amounts in the first (proliferative) half of the menstrual cycle. Progesterone is produced in the first part of the second half of the menstrual cycle (secretory phase), although levels decline after about 7 days. It is the drop in progesterone that is the stimulus for menstruation.
4. The symptoms of the menopause are attributed to falling levels of oestrogen. Sudden drops in oestrogen are considered to induce more profound symptoms than a more gradual drop in oestrogen levels.
Chapter 5.2b The investigation of the reproductive system
At the end of this chapter you will:
The investigation of the female reproductive system
The investigation of the female reproductive system includes
• a thorough physical examination, including internal examination of the uterus and ovaries
• blood tests and urine tests to assess hormone levels
• examination of samples of vaginal mucus
• cervical ‘smear’ (Pap smear) test
• imaging tests (in particular, pelvic ultrasound, endoscopy of the vagina and the womb, laparoscopy, and hysterosalpingography) to visualise the structure of the reproductive organs
The investigation of breast diseases
The investigation of breast diseases includes
The investigation of the male reproductive system
The investigation of the male reproductive system includes:
• a thorough physical examination, including examination of the testes and penis
• blood tests to assess hormone levels and to look for tumour markers
Physical examination of the male reproductive system
The prostate is examined by means of digital rectal examination.
The investigation of sexually transmitted diseases
The investigation of sexually transmitted diseases includes:
Blood tests
 Self-test 5.2b The investigation of the reproductive system
Self-test 5.2b The investigation of the reproductive system
1. Anthea is a 35-year-old woman who has gone to her doctor with a concern that she is developing a moustache on her lip. The GP does not think that the hair growth is excessive, but offers a referral to a gynaecologist, as there are some hormone treatments that might be offered.
Answers
1. Anthea will first be given a thorough gynaecological examination. This will involve examination of her skin and body hair. She will also have to have an internal pelvic examination so that the doctor can check that her ovaries feel normal in size. If she is not up to date with her smear tests, she may be offered one at this appointment.
 .
.
 .
. .
. .
.
 Information Box 5.2.a-I
Information Box 5.2.a-I .
. .
.
 .
. .
. .
. Information Box 5.2c-I
Information Box 5.2c-I .
. Information Box 5.2c-II
Information Box 5.2c-II Information Box 5.2c-III
Information Box 5.2c-III Information Box 5.2c-IV
Information Box 5.2c-IV



