CHAPTER 2 Chondral Lesions
ANATOMY AND PATHOANATOMY
Historically, arthroscopic techniques of the hip have been limited by the unique anatomy of the hip joint. The complex three-dimensional bony structures of the proximal femur, pelvis, and acetabulum create a small window through which instruments must be passed and manipulated. This unique anatomy limits arthroscopic access to certain intra-articular zones1 with respect to osteochondral grafting and even microfracture in some cases. Adequate visualization of the central and peripheral compartments requires arthroscopy performed with and without traction using varying degrees of capsulotomies.
The articular surfaces of the acetabulum and femoral head are covered by hyaline cartilage. A film of synovial fluid between the articular surfaces is maintained by the labrum, which acts as a seal, allowing for the distribution of contact forces. Ferguson and colleagues2 have used a finite model and hypothesized that the labrum’s sealing effect during load application maintains a pressurized layer of fluid, which prevents solid on solid, contact thus reducing wear. Loss of labral function may lead to increased cartilage degeneration or cartilage defects. The structure of hyaline cartilage can be divided into layers—superficial (tangential), middle (transitional), deep (radial), and calcified layers. The calcified layer plays an important role in chondral injuries sustained during increases in shear forces as seen in femoroacetabular impingement. As the chondral surface of the acetabulum encounters increased shear forces during impingement, the force is transmitted to the calcified layer, which is relatively weak and ultimately the site of failure. This produces the characteristic cleavage delaminations at the labrochondral junction. This shear force can also lead to a wave sign or chondral blister, and eventual deep delamination (carpet delamination) of the articular cartilage from the subchondral bone.
The causes of cartilage injuries vary. Cartilage defects may be associated with avascular necrosis (AVN), femoroacetabular impingement (FAI), dysplasia, Legg-Calve-Perthes (LCP) disease, osteochondritis dissecans, or trauma. FAI is a common cause of chondral lesions. Injuries to articular cartilage may vary in presentation from damage to the cellular matrix to osteochondral defects. Damaged cartilage may be visible, as characterized by the Outerbridge3 classification, or appear normal on initial inspection. Probing the articular cartilage will occasionally reveal softening or deep delamination that is not evident on initial inspection.
Cartilage lesions may be found on the femur, acetabulum, or both. Femoral lesions appear to be less common than acetabular lesions in patients who meet the indications for hip arthroscopy. Focal femoral chondral injuries can be iatrogenic, the result of hip dislocation or subluxation, or seen in association with AVN and Perthes (see Fig. 2-13A). For some conditions, such as FAI, the femoral surface may remain well preserved until late in the disease course. Thus, articular involvement on the femoral side is often reflective of advanced bipolar degenerative changes. Acetabular lesions can be associated with hip subluxation and dislocation, FAI, or secondary degenerative lesions as a result of femoral cartilage defects.
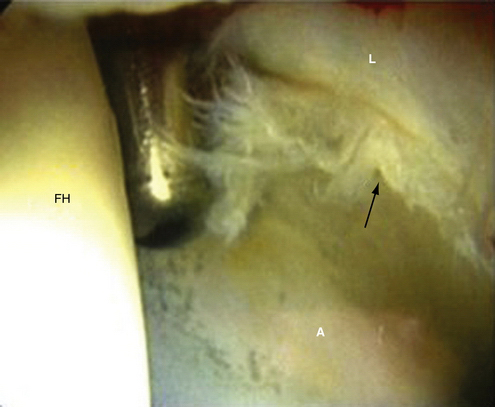
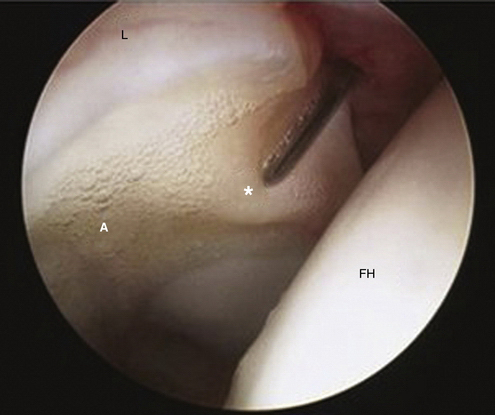
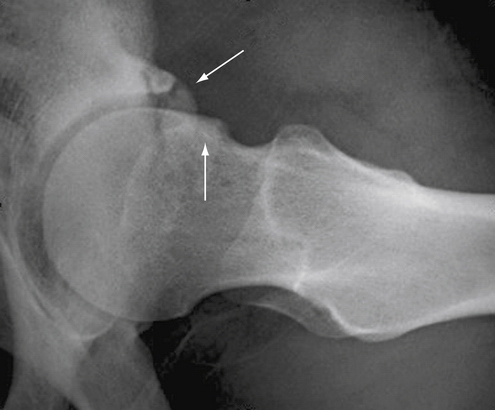
Chondral injuries may be found within specific locations on the femur or acetabulum according to cause. Most cartilage lesions treated in our practice arise in the setting of FAI. Chondral injuries seen in association with FAI have locations based on the type of impingement. Anterolateral cam impingement typically results in labrochondral disruption in the anterosuperior zones (zones 2, 3, and 4) with eventual cleavage delamination of the acetabular articular cartilage in this region (Fig. 2-1). Anterior-superior pincer impingement can lead to a more linear posterior acetabular chondral lesions (zones 4, 5) described as a contrecoupe lesion. Cam, Pincer, and mixed-type pathology can result in chondral blistering of the acetabular cartilage described as the wave sign (Fig. 2-2). This wave sign can indicate a predelamination injury or a deep carpet delamination of the articular cartilage or labrochondral complex without intra-articular extension. Chondral lesions can also be seen that involve detachment of the acetabular articular cartilage away from the labrochondral junction (toward the lunate fossa; see Fig. 2-17A). Each of these patterns has specific management options. In more advanced cases, full-thickness chondral lesions with exposed subchondral bone are seen (Fig. 2-3). Our observations are similar to those reported by McCarthy and Lee.4 They reviewed their findings of 457 hip arthroscopies and found the anterior and superior acetabulum to be the location of 73 % of the cartilage lesions. They also found that most anterior lesions were Outerbridge III or IV.
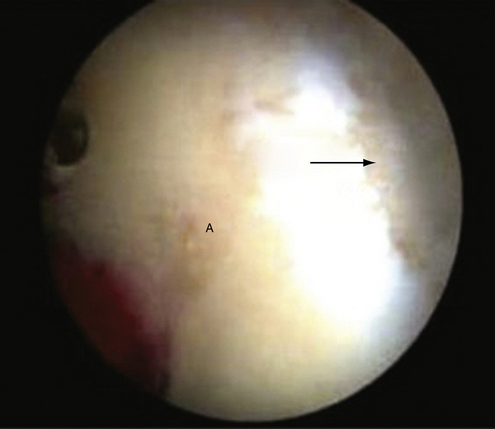
FIGURE 2-3 Full-thickness chondral defect in the anterosuperior acetabulum (arrow) in a left hip viewed through the anterior peritrochanteric portal. A, acetabulum.
Chondral injuries associated with dysplasia predominantly involve both the anterosuperior acetabulum and femoral head.5 Lesions involving the femoral head in the setting of dysplasia typically involve the superior weight-bearing portion of the head as opposed to involvement of the lateral, non–weight-bearing head-neck junction seen in FAI. In a series of hips that sustained lateral impact injuries, chondral lesions were located medially, with three patients demonstrating lesions on the medial weight-bearing region just superior to the cotyloid fossa and one patient with a lesion of the medial femoral head.6 Traumatic subluxation of the hip or dislocation may also result in osseous and chondral injuries. Philippon and associates7 reported on 14 professional athletes who were treated for traumatic dislocations of the hip, and each patient was reported to have an associated chondral lesion. Of these patients, 2 had isolated femoral head chondral defects, 6 had isolated acetabular chondral defects, and 6 had chondral defects on both surfaces. Moorman and coworkers8 have described an MRI triad for patients who sustained traumatic hip subluxations. The triad included a lesion located at the acetabular rim, based on the direction of injury, with a posterior osteochondral and labral avulsion from the acetabulum being most common. Traumatic subluxation or dislocation may also result in AVN or osteonecrosis of the femoral head. Nontraumatic causes of AVN are also common. Regardless of the cause, AVN most commonly results in osteochondral lesions of the anterosuperior femoral head. If subchondral collapse occurs, this typically leads to further degenerative changes throughout the hip.
HISTORY
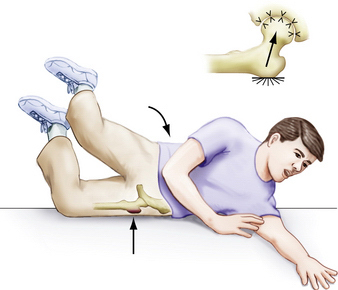
A thorough history and physical examination are essential when evaluating patients with suspected chondral lesions. A history of traumatic injury may be noted, such as hip subluxation, dislocation, or a fall directly onto the lateral hip (Fig. 2-4). More often, there is an insidious onset of hip pain, as seen in patients with FAI (Fig. 2-5). Patients with intra-articular pathology may complain of pain in the groin or anterior or deep lateral aspect of the hip. Occasionally, symptoms are referred to the posterior-buttock region or are a combination of anterior and posterior pain, as indicated by the C sign.9 Pain and discomfort are often exacerbated by activities such as running, cutting and pivoting in athletic endeavors, getting in and out of a car, arising from a seated position, and prolonged sitting. Patients occasionally note mechanical symptoms such as clicking, catching, or locking. In our experience clunking is more often associated with coxa saltans and not labral or chondral pathology. These complaints are indicative of intra-articular pathology and not specific to chondral injuries.
PHYSICAL EXAMINATION
Physical examination findings associated with chondral lesions tend to be vague and nonspecific. Gait evaluation is most often normal or mildly antalgic in patients with focal chondral lesions, with the exception of acute traumatic injuries. Inspection of the patient in the supine position is helpful. In the setting of acute trauma associated with a hip effusion or hemarthrosis, the patient may hold the leg in slight flexion, external rotation, and abduction. This position places the joint capsule at maximal volume and is a more comfortable position. Palpation of the involved hip should include the following areas: groin, trochanteric and peritrochanteric regions, anterior and inferior iliac spines, buttocks, lumbar spine, pubic rami and symphysis, insertion of the rectus abdominus, external oblique, and adductor origins. Extra-articular pain often accompanies intra-articular pathology and the primary or initial source of pain should be sought. Motion may be limited by guarding in the traumatic or chronic setting because of synovitis of the hip. The Stinchfield test and supine log roll test assess hip irritability and are suggestive of an intra-articular process.9 ROM, in particular internal rotation and flexion, may be limited in the setting of FAI. Alternatively, ROM may also be relatively increased in the setting of dysplasia or increased femoral anteversion. When performing provocative tests, it is imperative to verify whether the elicited pain is in fact the presenting complaint.
DIAGNOSTIC IMAGING
Initial imaging evaluation includes anteroposterior pelvis, false profile, and lateral hip radiographs. The anteroposterior radiograph should have the coccyx centered over the symphysis with 0 to 3 cm between these two structures. Plain radiographs can reveal rim fractures in the setting of hip dislocation or subluxation and structural abnormalities such as FAI, dysplasia, AVN, LCP, or loose bodies. Any significant joint space narrowing should be noted as this may significantly impact the success of hip arthroscopy. In the setting of hip subluxation or dislocation, Judet views allow for better assessment of the acetabulum, specifically the acetabular rim. Various radiographic measurements are routinely performed to understand the cause of the intra-articular pathology better. Our routine measurements and evaluation include the lateral center edge angle, anterior center edge angle, Tonnis angle, presence of femoral head lateralization, AP and lateral alpha angles, presence of a crossover sign, prominent ischial spines, coxa profunda or protrusio, os acetabuli or rim fractures, neck shaft angle, and Tonnis grading for degenerative changes.
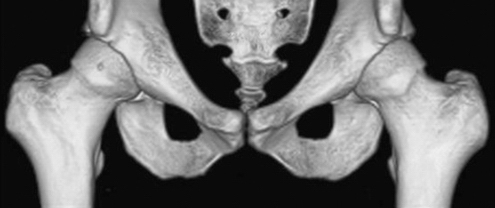
Computed tomography (CT) scans are helpful for further defining fractures, loose bodies, and structural abnormalities. In the setting of an acute subluxation, a CT scan is helpful to assess for posterior or, less commonly anterior, rim fractures. A concomitant radiographically guided aspiration can also aid in decompressing a traumatic hemarthrosis when present. We frequently obtain three-dimensional reconstructions for patients with FAI (Fig. 2-6). We find that it is helpful for defining the extent of impingement and planning the rim resection and proximal femoral osteochondroplasty commonly associated with most chondral lesions.
Magnetic resonance imaging (MRI) and MR arthrography (MRA) provide better assessment of soft tissues as well as more accurate staging of AVN. Nonarthrography MRI offers the advantage of being noninvasive but with less accuracy in identifying labral and chondral pathology. When assessing labral tears, Czerny and colleagues12 found that the sensitivity of MR arthrography was 90% and its accuracy was 91%, whereas the sensitivity of MRI was 30% and its accuracy was 36%, compared with open surgical findings. MRA, however is less sensitive for diagnosing chondral lesions in comparison to labral pathology. Keeney and associates13 published their results comparing MRA with hip arthroscopy. With respect to articular cartilage pathology, MRA had a sensitivity of 47%, specificity of 89%, positive predictive value of 84%, negative predictive value of 59%, and accuracy of 67%. The addition of a diagnostic anesthetic injection is helpful to verify the hip joint proper as the source of pain.33 New delayed gadolinium-enhanced magnetic resonance imaging of cartilage (dGEMRIC) MRI techniques may lead to improved detection of subtle chondral lesions.15
INDICATIONS AND CONTRAINDICATIONS
Contraindications to arthroscopic treatment of chondral injuries must be kept in perspective to optimize outcomes. Patients with moderate or severe osteoarthritis and a predominance of aching pain provide little opportunity for significant improvement, even in the short term. A recent study by Larson and coworkers15
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree