10 Chondral Injuries Treated with Osteochondral Autograft Transfer
Chondral defects of the weight-bearing area of the femoral condyles may be treated using an osteochondral autograft transfer (OAT). The procedure may be done open or under arthroscopic control. Cylindrical donor cores of hyaline cartilage with subchondral bone are harvested from a non-weight-bearing area of the knee and are transferred press fit to a recipient socket prepared over the chondral defect. The osteochondral graft restores joint surface congruity with hyaline cartilage. Although a concern, harvest-site morbidity has not been seen. Rehabilitation is fast, and outcome is predictably good.
Patient Presentation and Symptoms
Patients may have a history of recent trauma with concomitant localizing pain, swelling, and possible mechanical symptoms. Physical examination may reveal an effusion, joint line tenderness, or tenderness directly over the effected femoral condyle. The physician must have a high degree of suspicion for such an injury in adults (age <45) with known anterior cruciate ligament (ACL) or meniscal pathology.
Indications
- Full-thickness (Outerbridge grade IV) chondral lesions of the weight-bearing area of either femoral condyle
- The lesion should be well circumscribed with a sharp transition zone.
- Less than 2 cm in diameter
- Young patient (<45 years)
- Normal axial tibio/femoral alignment
Contraindications
- Older patient (>55 years)
- Osteoarthritis
- Lesion greater than 2 cm in diameter (rare)
- Osteochondritis dissecans (lesion may be too large with poor subchondral bone)
- Axial malalignment
Diagnostic Tests
- X-ray: alignment, osteoarthritis, avascular necrosis
- Magnetic resonance imaging (MRI) suppressed and pulsed images demonstrate edema at site of chondral defect.1
- Arthroscopy: may be concomitant with other pathology
Special Considerations
The quality of the surrounding hyaline cartilage is an important consideration particularly for middle-aged patients. Some individuals over the age of 45 may have a healthy chondral surface surrounding a defect, and therefore may be considered for an OAT. Most importantly, a transfer must not be done in an early arthritic lesion or a lesion with a poor transition zone.
Re-creating a flush articular surface during transfer requires rotational and depth control of the donor core during insertion. This is best accomplished by approaching the donor and recipient areas at 90 degrees, in both the coronal and sagittal planes. The donor core is harvested first and any obliquity is matched in creating the recipient socket. Depth of the core is noted and the recipient socket depth is matched.
Preoperative Planning and Timing of Surgery
- Lesion size may be determined by MRI.1
- OAT instruments should be available during ACL reconstruction or meniscal surgery and may be done concomitantly with these procedures.
- Surgery should be done in a timely manner in those known to have a chondral defect to prevent further injury. Small lesions get bigger over time.
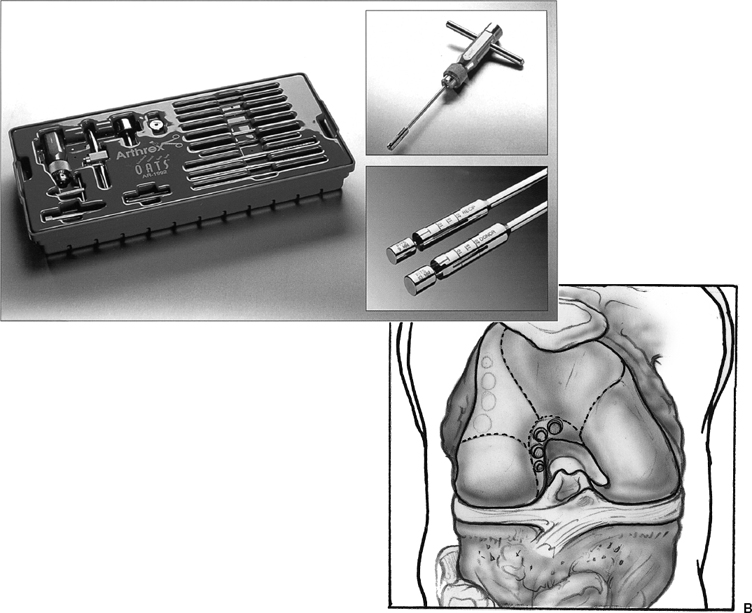
Special Instruments
- Osteochondral Autograft Transfer System (OATS, Arthrex, Naples, FL) (Fig. 10–1)
- Standard knee arthroscopy instruments
Anesthesia
General or spinal anesthesia
Patient Position
- Supine
- 120 degrees of knee flexion is needed.
Surgical Procedure
Standard anterolateral and anteromedial arthroscopy portals may be used. Thorough diagnostic arthroscopy should include inspection of the chondral surface. Ligamentous and meniscal pathology should be addressed.
Donor Harvest
- The donor area of choice is the lateral femoral condyle just above the sulcus terminalis (Fig. 10–2).
- The chondral defect is measured using the provided sizing instruments (Fig. 10–3). Sizes may be from 8 to 11 mm. More than one plug may be used. A small number of large plugs is better than many small plugs to minimize fibrocartilage dead space.
- With the arthroscope in the medial portal, the donor area is brought to the lateral portal by extending the knee.
- The harvester engages the donor cartilage at 90 degrees, then is impacted to a depth of 15 mm (Fig. 10–4). Twisting the instrument handle 180 degrees or more dislodges the core from the cancellous bone and allows for removal. (An assistant is needed during this step to hold the leg and arthroscope.)
- Observe for any obliquity of the harvested core within the harvesting instrument. Leave the core inside the harvester. View the core through the harvester window
Recipient Socket (Fig. 10–5)
- Bring the recipient site to the corresponding portal.
- Create a core using the recipient harvester (1 mm smaller than donor), and approach at an angle to match the donor core. Impact to 15 mm, rotate the instrument, and extract in a similar fashion (Fig. 10–5B).
- Use alignment stick to fine-tune recipient socket depth and to correct angle (Fig. 10–5C).
Transfer
- Place the depth stop on the back of the chuck handle loaded with the donor harvester (containing core) (Fig. 10–6).
- Flex the patient’s knee to match the recipient socket.
- Place the leading edge of the donor harvester at the orifice of the recipient socket (matching angles) (Fig. 10–7).
- Maintain knee flexion and harvester approach angle; tap the plunger pin until it is flush with the depth stop at the proximal end of the chuck handle. Observe the passage of the core arthroscopically through the window of the harvester. Withdrawing the harvester should leave the donor core 1 mm proud.
- A flush transfer is completed using a tamp of larger diameter (avoid countersinking and tap lightly) (Fig. 10–8).
Dressings, Braces, Splints, and Casts
Portals are covered with a soft dressing, and the knee is wrapped in an Ace bandage.
Tips and Pearls
- Portals may need enlarging to accommodate harvester (1 cm).
- Do not lever the instrument when harvesting the cores.
- Removing an inserted core weakens the fixation.2
- Larger-diameter cores will improve graft fixation and may be considered in those with poor bone quality.
Pitfalls and Complications
A large hemarthrosis may result from the surgery. Aspiration may be needed and sutures may need to remain in place for up to 2 weeks.
Postoperative Care3
- Soft dressing
- Immediate active, active assisted, and passive range of motion (ROM)
- Non—weight bearing for 2 weeks
- Thigh muscle stretching and strengthening for 3 months
- Avoid running and sports for 3 months.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








