CHAPTER 4 Cam-Type Femoroacetabular Impingement
Surgical correction of various hip impingement problems was described even early in the last century.1,2 In 1975, Harris and coauthors described the pistol grip deformity of the femoral head observed in association with early-onset osteoarthritis.3 In 1998, we described arthroscopic correction of impingement caused by post-traumatic osteophytes and also reported an arthroscopic technique of cheilectomy for femoral protuberances associated with Legg-Calvé-Perthes disease.4,5 However, it was Myers, Ganz, Lavigne and colleagues6–8 who formulated the concept of femoroacetabular impingement, describing pincer, cam, and combined types. Subsequently, we have reported arthroscopic methods for correcting this disorder.9–11
We have identified a bimodal population of patients with cam-type femoroacetabular impingement (FAI).11 One is the typical middle-aged patient (average age, 43 years, with a 1.9:1 male-to-female ratio) who presents with early-onset osteoarthritis. The second population is much younger, with an even greater male preponderance (average age, 20 years, with 3.1:1 male-to-female ratio) and most (70%) are involved in athletic activities. These are active individuals who have pushed their hip beyond its diminished physiologic limits and have sustained substantial joint breakdown at a young age.
ANATOMY AND PATHOANATOMY
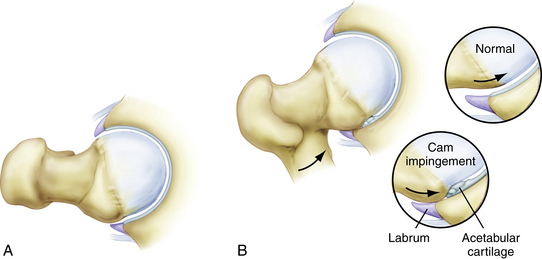
Cam-type FAI refers to the cam effect created by a nonspherical femoral head. During flexion, the prominence of the out-of-round portion rotates into the acetabulum, engaging against its surface and resulting in delamination and failure of the acetabular articular cartilage (Fig. 4-1). Early in the disease process, the labrum is relatively preserved but, with time, it begins to sustain secondary damage.
Cam impingement is classically attributed to a slipped capital femoral epiphysis, resulting in a bony prominence of the anterior and anterolateral head-neck junction. However, the most common cause is the pistol grip deformity, attributed to a developmental abnormality of the capital physis during growth. The exact cause is unclear; it may represent premature asymmetrical closure of the physis; it has been postulated that this could be caused by late separation of the common proximal femoral growth plate that forms the physis of the greater trochanter and femoral head.12
HISTORY AND PHYSICAL EXAMINATION
Patients with cam impingement have typical hip joint–type symptoms.13 The onset may be gradual or associated with an acute episode, which is the culmination of altered wear developing over a protracted period of time. Patients with cam impingement usually have reduced joint motion, which can result in other secondary disorders. Athletes compensate with increased pelvic motion, often resulting in problems with athletic pubalgia.14 More stress is placed on the lumbar spine, resulting in concomitant lumbar disease.
Pain with flexion, adduction, and internal rotation is almost uniformly present and is referred to as the impingement test (Fig. 4-2).7 However, in our experience, this maneuver is uncomfortable for most irritable hips, regardless of the underlying cause, and thus is not specific for impingement. Laterally based cam lesions may result in painful abduction or external rotation (Fig. 4-3). Internal rotation of the flexed hip is usually diminished, but may be preserved in some patients (Fig. 4-4). Limited range of motion may be present bilaterally because the morphologic variation is often present in both hips.
DIAGNOSTIC IMAGING
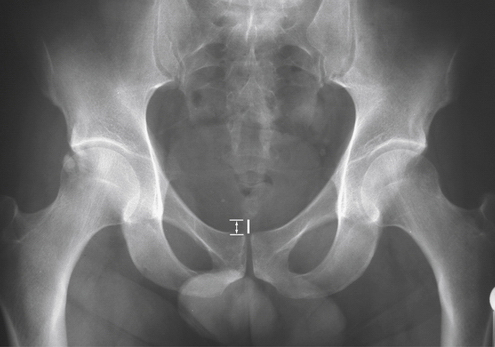
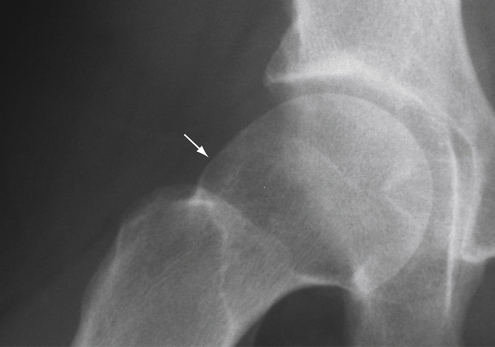
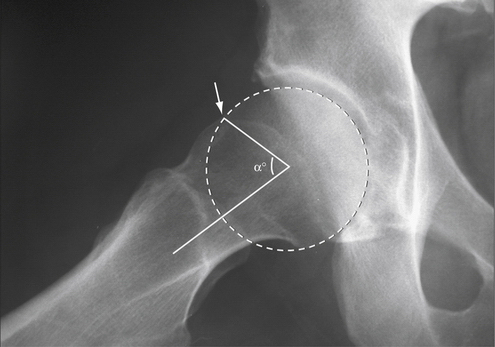
Radiographs are essential for the routine evaluation of impingement. A well-centered anteroposterior (AP) pelvis x-ray is important for assessing the acetabular indices of pincer impingement, but also allows observations on the cam lesion comparing both hips (Fig. 4-5).15 The epicenter and shape of the cam lesion are variable. Thus, although the 40-degree Dunn view has been reported as the best image, we have found that no single lateral radiographic view is reliable for optimally assessing the cam lesion in all cases (Fig. 4-6).16 Sometimes, the cam lesion is more anteriorly based and sometimes more lateral. The characteristic feature is loss of sphericity of the femoral head. The alpha angle has been described to quantitate this observation (Fig. 4-7).17 However, imaging will underinterpret this measurement unless it catches the maximal location of the cam lesion. Also, no studies have shown a significant correlation between the amount of correction of the alpha angle and the results of surgery, indicating that there may be other factors at play.
Magnetic resonance imaging (MRI) and gadolinium arthrography with MRI (MRA) aid in assessing secondary damage to the articular cartilage and labrum associated with cam impingement.18 These studies are better at detecting labral pathology but reveal the severity of articular involvement less often. The alpha angle can again be recorded, but is still variable, depending on whether the cross-sectional images catch the maximal location of the cam lesion.
INDICATIONS AND CONTRAINDICATIONS
The indication for hip arthroscopy is imaging evidence of intra-articular pathology amenable to arthroscopic intervention, or sometimes recalcitrant hip pain that remains refractory to efforts at conservative treatment. It must be kept in mind that imaging studies may often underestimate the severity of intra-articular pathology. Correction of an accompanying cam lesion has been performed, when present, especially when there was arthroscopic evidence that it was responsible for the concomitant joint pathology. This secondary joint damage is best characterized by failure of the anterolateral acetabular articular surface. The failure is most typically represented by articular delamination with the peel-back mechanism, but earlier in the disease process may be characterized by deep, closed, grade I articular blistering, referred to as the wave sign.19
It is our opinion that radiographic findings of impingement, in the absence of clinical findings of a joint problem, are not solely an indication for arthroscopy. Some individuals with impingement morphology may function for decades without developing secondary joint damage and symptoms. For some, it is unclear when, or if, they will develop problems warranting surgical intervention. For example, many individuals may present with symptoms in one hip when radiographic findings of impingement are present in both. Although intervention in the asymptomatic joint would not be appropriate, it is important to educate the patient about warning signs of progressive joint damage. It is a clinical challenge in the decision not to intercede too early or too late. In our experience, 93% of patients undergoing arthroscopy for cam impingement demonstrate Grade III or IV articular damage, reflecting that the disease process is already substantially advanced at the time of intervention.11
Contraindications include advanced disease states, such as grade III Tonnis changes, and sometimes there are patients who do not have reasonable expectations of what can be accomplished with the procedure.20 Because the success of the operation is ultimately dictated by the patient’s impressions, it may be important to modulate the patient’s goals. Also, in the presence of secondary degenerative disease, the potential advantages of a joint-preserving procedure must be weighed against the high level of satisfaction associated with arthroplasty procedures.
TREATMENT
Conservative Management
Conservative management begins with an emphasis on early recognition of the underlying impingement disorder. The mainstay of treatment is identifying and modifying offending activities that precipitate symptoms. Some individuals can modify their lifestyles and stabilize the process for years. Efforts can be made to optimize mobility of the joint, but these are only modestly effective because motion is limited by the bony architecture, which cannot be corrected with manual techniques. Decompensatory disorders are those secondary problems that develop as individuals struggle to compensate for the chronic limitations imposed by the impingement. A conservative strategy must include assessment and treatment of the secondary problems, which can contribute substantially to the patient’s symptoms.
Surgical Technique
The procedure begins with arthroscopy of the central compartment to assess for the pathology associated with cam impingement. This is carried out with the standard supine three-portal technique that has been well described in the literature (Fig. 4-8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree