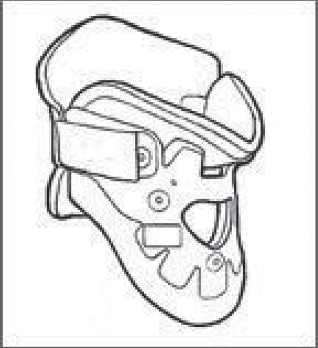
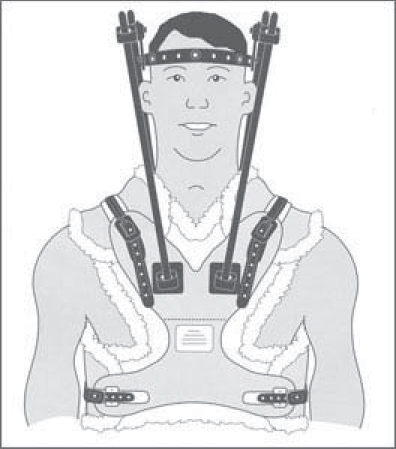
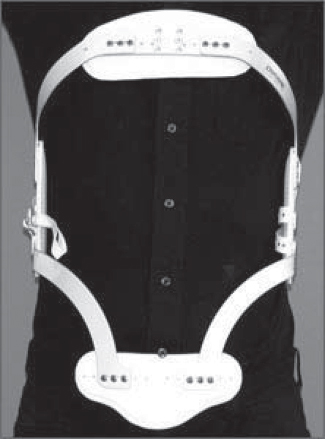
71 External immobilization of the spine has been used for centuries to treat spinal conditions from acute trauma to chronic deformity. Current use is controversial and remains variable in clinical practice, as good-quality evidence is often lacking. The goal of bracing is to eliminate or to neutralize the forces acting on the spine to provide stability when normal physiologic stability has been compromised by a pathologic process. This situation arises in acute trauma, tumor, or infection as well as in idiopathic scoliosis and degenerative conditions of the spine. It is important that there should be a foreseeable endpoint to brace treatment. If no such end to bracing can be predicted, surgery or an alternate treatment must be strongly considered. To immobilize the spine effectively, a brace must overcome both intrinsic forces, such as muscle pull or imbalance, and external forces, such as gravity. Unlike braces and orthoses used in the extremities, a spine brace is limited by the difficulty in obtaining fixation points, particularly in the upper and lower extremes of the spine. It is also limited by the distance between the brace itself and the bony spinal column, a space which is filled with soft tissue, including the visceral organs and large muscle groups. Many braces overcome this difficulty by extending beyond the area of pathology to fix on very proximal or distal points. In the cervical spine, some orthoses capture fixation on the skull, mandible, or the occiput, while in the lumbar spine, these devices fix to the bony prominences of the pelvis or the thigh. Braces should be fitted by a qualified orthotist working closely with the spine team. Because of the risk of complications, close surveillance is required, and brace adjustments should be made if necessary. Patient factors, including body size and habitus, as well as concurrent injury, must all be considered before the choice to use an orthosis is made. Patients and their caregivers should also be aware of the considerable cost of many customized braces and need to be taught the appropriate techniques for donning and removing the device. Without proper use, a patient may use a brace inappropriately or ineffectively, leading to treatment failure and potential morbidity. Patient preference must be strongly considered when deciding on a brace for treatment, as a brace that is not worn through poor compliance will fail to be of any use to the patient or physician. A broad range of cervical and cervicothoracic orthoses are available. These vary from soft collars that have very limited effect on spinal motion to rigid external devices that fix the position of the skull relative to the shoulders and chest. The different devices vary both in the material of construction and the points of fixation. Those with poor proximal and distal fit suffer from so-called parallelogram motion as the head extends and the spine flexes, particularly when the collar lacks an anterior buttress. Another shared problem with all cervical and cervicothoracic orthoses is “snaking,” or segmental motion in the sagittal plane with no overall change in position of the most proximal and distal points. This most frequently occurs in the mid-cervical region, which must be considered when a brace is used to treat instability in this region. The simplest cervical orthrosis is a soft collar. This device has limited usefulness because it does little to restrict cervical motion. It has virtually no points of fixation proximally or distally and allows motion in all degrees of freedom. There are a variety of hard cervical collars or high cervicothoracic orthoses, including the Miami J (Jerome Medical, Moorestown, NJ), the Philadelphia collar (Philadelphia Cervical Collar Co., Thorofare, NJ), and the Aspen collar (Aspen Medical Products, Irvine, CA) (Fig. 71.1). These devices all share similar characteristics, with proximal fit onto either the occiput posteriorly or the mandible anteriorly, and extension over the base of the neck and medial shoulder girdle distally. Biomechanical and radiographic in vivo studies have shown the effectiveness of these devices to be very similar. All are more effective in the upper cervical spine and are particularly poor at controlling motion below the C6 level. Collars are generally uncomfortable, so patient preference should be considered in light of their similar effectiveness. Cervicothoracic orthoses (CTOs) obtain fixation to the chest and lateral shoulder girdle, which provides enhanced stability to the lower cervical spine and cervicothoracic junction. The larger working distance from the face or skull to the chest also improves immobilization in the upper spine, particularly at the occiput to C2 levels, where fractures often occur. A variety of CTOs are available, including the SOMI (sternal-occipital-mandibular immobilizer) brace, the Lerman Minerva brace (United States Manufacturing Company, Pasadena, CA), and the two- or four-post Aspen CTOs, which include the Aspen collar as a component (Aspen Medical Products, Irvine, CA) (Fig. 71.2). Probably the gold standard is the halo vest, a commonly used cervicothoracic orthosis with direct fixation of the skull. It consists of pins inserted around the skull at its widest point, connected with a ring and rigid bars to a tightly fitting vest (Fig. 71.3). Contraindications to using a halo vest include skull fracture, sepsis, head injury, and chest injury. It maintains excellent immobilization of the cervical spine, particularly at the cervicothoracic junction and upper cervical spine. It allows some snaking motion of the mid-cervical spine, however, limiting its use for treating injuries at these levels. Other CTOs, such as the Minerva brace, are less effective in controlling rotation and motion at the cervicooccipital junction, but they can be more effective in preventing snaking. The Milwaukee body cast, which is no longer commonly used except in deformity treatment, has the best control of the spine in all areas. In choosing a cervical or cervicothoracic orthosis, one needs to consider the amount of immobilization required, as well as the spinal levels of most importance, while limiting patient discomfort and inconvenience. Fig. 71.1 Aspen collar. Fig. 71.2 Aspen cervicothoracic orthosis (CTO). Fig. 71.3 Halo vest. A variety of orthoses are used to immobilize the thoracic and lumbar spine, ranging from a soft lumbar corset to rigid plastic thoracolumbosacral orthoses (TLSOs). The thoracic spine has inherent stability because of its attachment to the rib cage from T1 to T10. The same stability does not apply to T11 and T12, which have floating ribs. Distally, lumbar braces must have some point of fixation four to five levels below the level of pathology. This often mandates the tight fit of a rigid orthosis onto the iliac crest, sacrum, or a thigh extension. Because of the increased soft-tissue thickness between the brace and the spine as well as the large forces generated by the paraspinal muscles, complete immobilization of the lumbar spine is particularly difficult. The simplest brace is a lumbar corset. These devices have been used to treat back pain and postsurgical instability, although there is minimal evidence for their effectiveness. Although it lacks a rigid external structure, the corset adds stability by increasing intraabdominal pressure. Several more rigid devices exist, including off-the-shelf orthoses and custom thermoplastic body casts. Non-customized braces employ a three-point bending strategy with a metal frame to control either flexion (Jewett brace) (Fig. 71.4) or extension (Williams brace). These braces do not control rotation or lateral flexion well. They have the advantage of being easy to fit and cheaper, and are less intrusive than plastic body casts. TLSO braces are typically made from a custom mold using thermoplastic, rigid materials. They may be one piece (e.g., Boston brace) or clamshell style with strong attachments from front to back (Fig. 71.5). Any motion or slide between the clamshell halves reduces the overall function of the orthosis. TLSOs are effective only as high as T6 without the use of a neck extension, and lose their effect dramatically below L3–L4. A thigh extension may be extended distally to immobilize the L4–L5 and L5–S1 levels. The extension is typically added to the stronger leg. For the thoracolumbar region, off-the-shelf hyperextension braces as well as both one-piece and two-piece clamshell braces all have reasonable effectiveness in immobilizing the spine in extension, which is the most common goal. Fig. 71.4 Front view of Jewett extension brace.
Bracing and Orthoses
![]() Brace Types
Brace Types
Cervical Spine

Thoracic and Lumbar Spine
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






