Chapter 12 Biomechanics of the upper limb
Motion
Description of motion
The description of motion becomes detailed when multiaxial joints, such as the glenohumeral joint, are studied. The eulerian angle system is a method that has utility in describing three-dimensional rotation.4,5 This method takes into consideration the fact that three-dimensional rotation is sequence dependent. This description can be applied clinically to describe the range of joint motion as well as specify joint position in orthotic prescription.
Normal range of motion arcs versus functional motion requirements
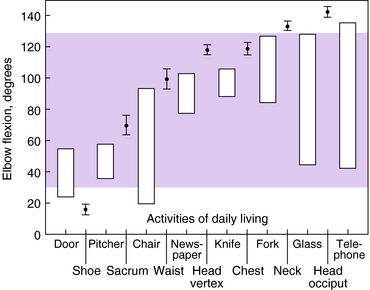
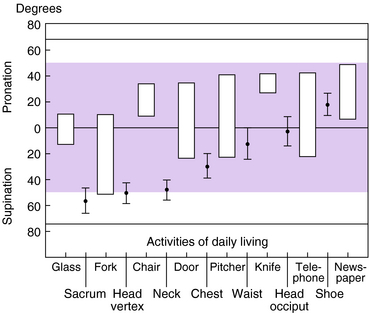
When studying upper extremity motion, it is important to delineate between the normal arc of movement standards for specific joints and the functional arc of motion required for most daily activities. For example, although the elbow has a normal arc of flexion–extension of 0 to 150 degrees and pronation and supination of 75 to 85 degrees, respectively,15 the full arc of motion is not generally used for most activities of daily living. A study of the functional elbow arc of motion conducted by Morrey et al.66 revealed that 15 activities of daily living can be carried out with an arc of motion of 30 to 130 degrees of flexion–extension (Fig. 12-1). Furthermore, these same activities required an equal amount of 50 degrees of pronation and 50 degrees of supination. Those activities that use an arc of motion require it be about equally centered between pronation and supination. Note that the activities studied were related to activities of daily living. Special requirements for other activities, including occupational tasks, have not been clearly elucidated. Figure 12-2 illustrates the importance of forearm supination and pronation in positioning the upper extremity for feeding and dressing tasks.
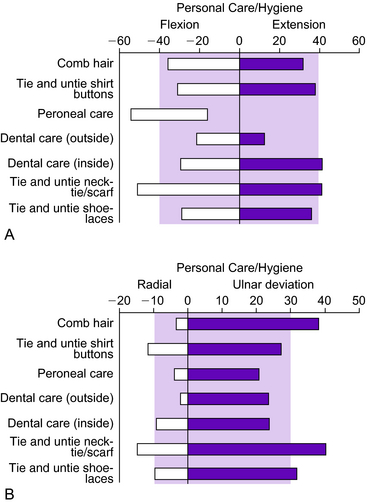
Similarly, the wrist has a normal arc of flexion of 80 to 85 degrees, approximately 70 degrees of extension, 20 degrees of radial deviation, and 30 degrees of ulnar deviation.2 Ryu et al.84 examined 40 normal subjects (20 men and 20 women) to determine the range of motion required to perform activities of daily living. The amount of wrist flexion and extension, as well as radial and ulnar deviation, were measured simultaneously using a biaxial wrist electrogoniometer. The entire battery of evaluated tasks could be accomplished with 60 degrees of extension, 54 degrees of flexion, 40 degrees of ulnar deviation, and 17 degrees of radial deviation. The majority of the hand placement and range of motion tasks studied in this project could be accomplished with 70% of the maximal range of wrist motion (Fig. 12-3). This converts to 40 degrees each of wrist flexion and extension and 40 degrees of combined radial–ulnar deviation (30 degrees of ulnar deviation, 10 degrees of radial deviation). The knowledge of functional range of motion requirements for activities of daily living can act as a guide when developing orthotic assistive devices. It should be an objective to provide devices that will allow motion in order to perform functional tasks and, ideally, occupational tasks.
Compensatory motion in the upper extremity
Contrary to accepted thought, the primary functions of the shoulder complex and elbow are mutually exclusive. It has been observed clinically that patients can tolerate elbow flexion contractures of about 30 degrees without much functional impairment. On the other hand, it also is well recognized that with motion loss greater than 30 degrees, patients readily complain of functional impairment. To better understand the implications of this loss of motion, it should be recognized that the shoulder functions as a ball and socket joint, allowing the hand to move in a spherical boundary in space.65 As the elbow moves into a more extended position, a new sphere surface may be described. Thus, the effective sphere of influence of the hand extends from the patient as far into space as the link at the elbow allows. It has been calculated that a loss of elbow motion of 30 degrees, 45 degrees, and 60 degrees leads to loss of functional volume of the hand by 28%, 39%, and 60% respectively.
A study by O’Neill et al.79 analyzed compensatory motion in the upper extremity after simulated elbow arthrodesis. The 3Space Tracker System (Polhemus, Inc., Colchester, VT) was used to measure shoulder motion, a biaxial wrist goniometer was used to measure wrist compensation, and all subjects were videotaped to qualitatively observe other compensatory motion. Ten healthy male subjects were asked to complete a series of tasks that represented use of the elbow in functional tasks. They were fitted with a custom adjustable brace that simulated elbow arthrodesis at 50, 70, 90, and 100 degrees of flexion and asked to repeat the tasks. Unlike other joints, elbow arthrodesis at any angle resulted in a significant impairment because the adjacent shoulder and wrist joints could not compensate to allow completion of activities. In upper extremity orthotic design, it is important to apply this information to understand the role and limits of compensatory motion of adjacent joints in providing function after injury or disease.
Synergistic motion of wrist and hand
Awareness of the relationship between wrist joint position and tendon excursion is essential for understanding motor control of the fingers and hand. Positioning the wrist in the direction opposite that of the fingers alters the functional length of the digital tendons so that synergistic finger movement can be attained. Wrist extension is synergistic to finger flexion and increases the length of the finger flexor muscles, allowing increased flexion with stretch.100 In contrast, wrist flexion is synergistic to finger extension, with wrist flexion placing tension on the long extensors, facilitating finger extension. This relationship has application in tendon-splinting techniques with respect to affecting tendon excursion through positioning and the potential benefits of synergistic wrist motion and metacarpophalangeal (MP) joint motion in promoting flexor tendon gliding after repair. Also, synergistic wrist motion principles are the basis for many orthotic designs that provide assistive function of the hand with quadriplegia.
In a study by Horii et al.,46 the efficacy of a new technique that used synergistic wrist motion (S-splint) was compared with traditional dorsal splinting methods used for mobilization of the flexor tendon after repair: the Kleinert splint (K-splint) and the Brooke Army Hospital/Walter Reed modified Kleinert splint with a palmar bar (P-splint). The results of this study question the anticipated tendon excursion associated with postoperative splinting. They demonstrated that the measured tendon excursion under a condition of low tendon tension was almost half that of theoretically predicted values. In zone II, the magnitude of excursion introduced by the three mobilization methods were in descending order: S-splint, P-splint, K-splint (P < .05). The differential tendon excursion between the flexor digitorum profundus and the flexor digitorum superficialis had a mean value of 3 mm and was not significantly different among the three methods. Passive proximal interphalangeal (PIP) joint motion was the most effective means of providing increased amplitude of tendon gliding in zone II. Passive distal interphalangeal (DIP) joint motion did not increase excursion in zone II as much as had been predicted. Further study is needed to test new designs of splints in vivo.
Stability
Shoulder
In the normal shoulder, the articulating surfaces of the humerus and glenoid provide minimal stability to the shoulder.9 The contact area between the two articulating surfaces is relatively small, with only 25% to 30% of the humeral head in contact with the glenoid surface in any anatomical location. Because the glenohumeral joint does not possess inherent bony stability, it relies to a greater extent on capsular, ligamentous, and dynamic muscular activity for constraint.
The capsule and ligamentous structures of the shoulder function in a coordinated manner to resist joint translation. This occurs primarily by resisting displacement but secondarily by soft tissue constraints imparting increased joint contact pressure opposite the direction of the displacement. Dempster30 studied the relationship between increased joint contact pressure and resistance to translation. The influence of atmospheric pressure or intraarticular pressure on the stability of the shoulder has been assessed in experimental and analytic investigations.9 The shoulder was seen to subluxate inferiorly by as much as 2 cm after capsular puncture, with marked alteration in joint constraint while performing passive motion. Venting of the capsule in cadaveric specimens was found to have a significant effect on the position of the humeral head. The mean intraarticular pressure was −76 cm H2O without load, and values decreased in a linear fashion with increased load.
Dynamic shoulder stability during activity is achieved by the shoulder musculature.85 The role of the rotator cuff in shoulder joint stability is well recognized. Howell et al.48 demonstrated in a cadaveric study that the humeral head is positioned in the center of the glenoid in the horizontal plane by a centering mechanism provided by the active rotator cuff. Even in an unbalanced situation, without equal simulated muscle contraction from the anterior or the posterior cuff components, the activity of the remaining cuff centers the humerus on the glenoid surface. Thus, compression of the articular surfaces and the centering effect are believed to be accomplished by secondary tightening of the ligaments. The central role of the deltoid muscle in elevating the arm is countered by depressive action of the anterior and posterior rotator cuff musculature. Thus, the shoulder rotators stabilize the joint by increasing the compressive force between the glenohumeral articular surfaces.
Itoi et al.50 investigated the stabilizing effect of the long (LHB) and short head of the biceps (SHB) muscle. Anterior stability was analyzed in 13 cadaver shoulders. The LHB and SHB were replaced by spring devices, and translation tests of the arm at 90 degrees of abduction were performed by applying a 1.5-kg anterior force. The position of the humeral head was monitored by an electromagnetic tracking device with or without an anterior translational force; with loads of 0, 1.5, or 3 kg applied on either LHB or SHB tendons in 60, 90, or 120 degrees of external rotation; and with the capsule intact, vented, or damaged by a simulated Bankart lesion.
Elbow
The anterior bundle of the medial collateral ligament (MCL) has been implicated as the primary valgus stabilizer of the elbow, with the radial head serving as a secondary joint stabilizer.8,54 Hotchkiss and Weiland47 reported that all elbows became unstable after this structure was sectioned. In an unconstrained kinematic study using an electromagnetic tracking device, Morrey et al.67 demonstrated moderate joint laxity after sectioning of the anterior bundle of the MCL, even with an intact radial head. Sojbjerg et al.93 confirmed the importance of the anterior bundle of the MCL in a cadaveric model. Clinically, both Schwab et al.90 and Conway et al.24 emphasized the functional importance of the ligament reconstructions for patients with a deficiency of this structure.
Studies by O’Driscoll et al.77 suggested that the lateral ulnar collateral ligament is a major stabilizing structure for both rotational and varus instability. Injury to this ligament results in posterolateral rotatory subluxation of the elbow, as demonstrated by feelings of instability and a positive pivot shift test. Reconstruction of this ligament has been shown to restore stability to the elbow both clinically and experimentally.74,76
An et al.10 addressed in a cadaveric study the importance of the proximal ulna articular surface in providing joint stability. In this study, progressive excision of the proximal ulna resulted in a progressive decrease in the stability of the elbow. Valgus stress was in large measure (80%) resisted by the proximal portion of the greater sigmoid notch, whereas varus stress was primarily resisted by the distal portion of the joint surface (65%).
The coronoid process of the ulna is another important stabilizer of the elbow. A failure to reconstitute this structure after fractures occur has been correlated with elbow instability and a poor functional outcome.83 The coronoid process appears to be an essential osseous block to prevent posterior subluxation of the elbow joint, especially with the elbow in extension.
Forearm joint
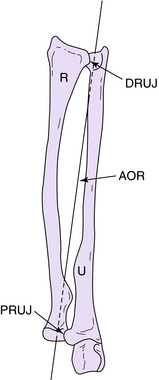
The forearm joint is a complex joint composed of the radius and ulna. In essence it is a bicondylar joint, with the proximal radioulnar joint (PRUJ) and distal radioulnar joint (DRUJ) serving as a condyle. The activity at either joint cannot be separated from the other joint due to the rigid body nature of the radius and ulna. The PRUJ is constrained by the mutual articulating surfaces of the cylindrical radial head and the lateral notch of the ulna, as well as the annular ligament and the joint capsule. The DRUJ is constrained by the articulating surfaces of the head of the ulnar and the sigmoid notch of the radius, as well as the distal radioulnar ligaments (forming the deep part of the triangular fibrocartilage complex) and the DRUJ joint capsule. In the center of the forearm, the interosseous membrane thickens to form the central band or ligament, which also contributes to forearm stability.53,69,107
The motion prescribed by the forearm can best be described as a pivoting behavior, with mobile hand–wrist–radius unit rotation around the fixed ulna.103 There is nearly total rotation at the PRUJ, with a nearly fixed axis of rotation passing through the geometric center of the head of the radius. There is a combination of rotation and translation through the DRUJ, with the forearm axis of rotation passing through the fovea region at the base of the ulnar styloid process (Fig. 12-4). The intersection of the forearm axis of rotation and the cortex of the head of the ulna reciprocally translates posteriorly in supination and anteriorly in pronation.
The factors leading to instability of the DRUJ have been studied extensively, including the contribution of the interosseous membrane to DRUJ stability as well as the contributions of components of the triangular fibrocartilage complex.1,42,89,97,106,107 Overall, the palmar radioulnar ligament and the dorsal DRUJ capsule can be considered the principal constraints against anterior translation of the radius relative to the ulna. The dorsal radioulnar ligament and the anterior DRUJ capsule are the principal constraints against posterior translation of the radius relative to the ulna. Clinically, the most common pattern of instability results from disruption of the common ligament attachment at the base of the ulnar styloid process, rendering both the dorsal and palmar radioulnar ligaments incompetent.42
The presence or absence of the ulnar head has become an important consideration in forearm stability. One of the most common procedures performed for painful arthritis of the DRUJ is the so-called Darrach resection, where the head of the ulna is simply excised.28 This has led to the appreciation of residual instability and pain, largely from convergence of the radius onto the ulna.63 A number of reconstructive procedures to restabilize the forearm joint following excision of the ulnar head have been proposed,18,86–88 but the most efficacious procedure to date has been implantation of an ulnar head endoprosthesis to reestablish direct contact between the radius and ulna.14,88,104
Wrist
In the wrist, a complex system of ligamentous constraints and the articulations of the joint surfaces contribute to stability. This complex ligament system can be divided into extrinsic and intrinsic components. The palmar intrinsic ligaments of the distal row appear to be strongly connected to the carpal bones, as demonstrated by Garcia-Elias et al.38,39
The scapholunate and lunotriquetral ligaments are thought to be the most critical ligaments of the wrist, and they accept the greatest load and strain prior to failure.73 Biplanar x-ray studies of normal and abnormal kinematics after sectioning of these ligaments have elucidated their importance in providing stability to the scaphoid and lunate.45 The ultimate strength behavior, stress–strain curves, and joint kinematic pattern descriptions may be of value in developing repair or reconstruction techniques for the scapholunate and lunotriquetral ligaments.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree