Fig. 32.1
Schematic drawing of the course of the axillary nerve after the quadrilateral space . Branches A anterior deltoid , M middle deltoid , P posterior deltoid (Modified with permission from Zhao et al. [70])
The posterior branch of the axillary nerve always supplies teres minor and the superior lateral brachial cutaneous nerve . The anterior branch passes on the deep surface of the deltoid to supply the anterior and middle deltoid . The posterior deltoid can be supplied by either or both branches. The middle deltoid can also be supplied by the posterior branch.
Flatow and Bigliani [25] described the tug test to identify the axillary nerve during a deltopectoral approach to the shoulder. One index finger is passed under the deltoid laterally to palpate the anterior branch. The other index finger is placed along the superficial surface of the subscapularis medially under the coracoid muscles (coracobrachialis and the short head of biceps) and then rotated inferiorly. The gentle tug applied by either finger will be transmitted to the other finger and is usually palpable (Fig. 32.2) (Video 32.1).
Fig. 32.2
‘Tug Test’. One finger is placed on the axillary nerve at the front of subscapularis, and the other finger under the deltoid on the anterior branch. A gentle tug applied by either finger will be transmitted to the other finger and is usually easily palpable (Modified with permission from Flatow and Bigliani [25])
32.1.2 Quadrilateral Space
The quadrilateral space is bound by the medial border of the humerus, teres major, teres minor and the long head of triceps. The axillary nerve and posterior circumflex vessels traverse the space [18] (Fig. 32.3).


Fig. 32.3
Posterior view of the Quadrilateral space, bounded by the humerus laterally, teres major inferiorly, teres minor superiorly and the long head of triceps medially. It is accompanied by the posterior circumflex humeral artery (Image courtesy of Dr Mark Ross, Brisbane, Australia)
32.1.3 Posterior Branch Axillary Nerve
All branches that supply the teres minor and the superior lateral brachial cutaneous nerve arise from the posterior branch. There are variable branches supplying the posterior and middle deltoid .
Loukas et al. [45] found the posterior branch gave a branch to the teres minor and the superior lateral brachial cutaneous nerve in 100 % of cases. A branch to the posterior part of the deltoid muscle was present in 90 % of cases and a branch to the middle part of the deltoid in 38 %.
Ball et al. [5] reported that the axillary nerve divided just anterior to the origin of the long head of the triceps at the 6 o’clock position on the glenoid face. Within the quadrilateral space , the posterior branch is medial to the anterior branch, at an average of only 1 mm lateral to the glenoid rim. The posterior branch courses medially and posteriorly along the lateral edge of the long head of triceps origin, inferior to the glenoid rim for 2–17 mm. The nerve to teres minor originated at the lateral edge of the long head of triceps origin. At this level the nerves lay directly on the joint capsule at the level of the glenoid rim. The nerve to teres minor coursed medially for 11–25 mm before entering the muscle in a medial direction on its inferior surface. A branch to the posterior deltoid was seen in 79 % of cases.
32.1.4 Anterior Branch Axillary Nerve
The anterior branch of the axillary nerve lies lateral to the posterior branch in the quadrilateral space and courses laterally from the glenoid rim toward the neck of the humerus. It travels around the neck of the humerus penetrating the subdeltoid fascia and runs anteriorly distal to the sub acromial bursa to supply the deltoid (Figs. 32.4 and 32.5).

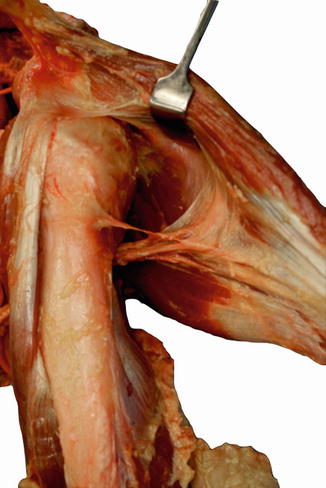

Fig. 32.4
Anterior branch of the axillary nerve . The deep surface of the deltoid muscle was exposed and the subdeltoid fascia removed to expose the axillary nerve (Reproduced with permission from Cetik et al. [14])
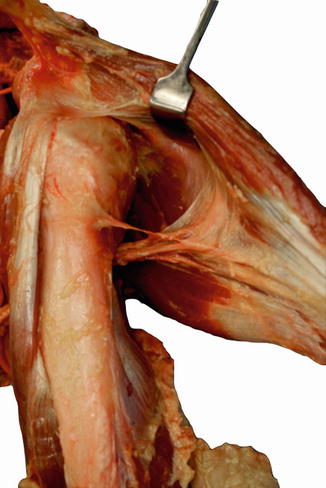
Fig. 32.5
Anterior view of the anterior branch of the axillary nerve traversing laterally from the glenoid rim around the neck of the humerus to supply the anterior and middle deltoid +/− posterior deltoid . (Image courtesy of Dr Mark Ross, Brisbane, Australia)
Zhao et al. [70] described three innervation patterns of the posterior deltoid . Type 1 (47.5 %) innervation by the anterior and posterior branches; Type 2 (42.5 %) innervation entirely by the posterior branch and Type 3 (10 %) innervation entirely by the anterior branch.
Zhao et al. [70] found that the whole of the middle and anterior deltoid was supplied by the anterior branch. The second articular branch to the glenohumeral joint, if present, usually arises from the anterior branch at the inferior border of the teres minor.
Loukas et al. [45] found the anterior branch provided a branch to the joint capsule, a branch to the anterior part of the deltoid muscle and the middle part of the deltoid muscle in 100 % of cases. In 18 % of cases the anterior branch of the axillary nerve provided a branch to the posterior part of the deltoid muscle. The middle part of the deltoid muscle received dual innervation in 38 % of cases and the posterior part of the deltoid muscle in 8 %.
Uz et al. [64] showed innervation of the posterior deltoid was from the posterior branch of the axillary nerve only in 70 %, both anterior and posterior branches in 26.7 % and from the anterior branch only in 3.3 %
Kulkarni et al. [41] studied the position of the axillary nerve in the deltoid muscle. The nerve was found to lie 2.2–2.6 cm superior to a midpoint on the vertical plane of the muscle (Videos 32.2 and 32.3).
32.1.5 Muscles Supplied
The teres minor is supplied by the posterior branch the axillary nerve .
The deltoid is supplied by the anterior and posterior branches of the axillary nerve . The deltoid arises from the anterior border and upper surface of the lateral third of the clavicle, from the whole of the lateral border of the acromion and from the inferior lip of the crest of the scapula spine. On the lateral border of the scapula four ridges may be seen; from them four fibrous septa pass down into the muscle. The deltoid tuberosity on the lateral aspect of the humerus is V-shaped, with a central vertical ridge. From the ridge and limbs of the V three fibrous septa pass upwards between the four septa from the acromion. The spaces between the septa are filled with a fleshy mass of muscle fibres which are attached to contiguous septa. The multipennate middle third of the deltoid so formed has a diminished range of contraction, but a correspondingly increased force of pull. The anterior and posterior fibres, arising from the clavicle and the scapula spine, are not multipennate. They converge on the anterior and posterior margins of the deltoid tuberosity, and their range of movement is greater but the force of their pull is less [57].
32.1.6 Superior Lateral Brachial Cutaneous Nerve
Zhao et al. [70] described two branching patterns of the superior lateral brachial cutaneous nerve . The more common pattern is that all branches of the nerve pierce the fascia on the posterior border of the deltoid . The second pattern has the superior lateral brachial cutaneous nerve dividing into two parts, with one part piercing the fascia on the posterior border of the deltoid , and another piercing the intermuscular septum between the posterior and middle thirds of the deltoid muscle [70].
Ball et al. [5] found the nerve with the arm in adduction pierced the deep fascia at the medial border of the posterior aspect of the deltoid 6.3–10.9 cm inferior to the posterolateral corner of the acromion. The nerve becomes subcutaneous at this level before crossing in an anterolateral direction into the overlying subcutaneous tissue. In no specimen did the nerve pass directly through the posterior deltoid to reach the subcutaneous tissue.
The nerve supplies an area of skin over the inferior deltoid also known as the ‘regimental badge area’ due to its location on the lateral upper arm.
32.1.7 Articular Branch and Proprioception
The innervation of the glenohumeral joint capsule has been widely described and is variable [22, 44, 64] Gelber et al. [27] pointed out the importance of the inferior glenohumeral ligament as a static stabilizer of the glenohumeral joint. The innervation of the inferior glenohumeral ligament is important as being one of the determinants of proprioceptive properties of the glenohumeral joint. Whether it is injured in shoulder joint lesions or not, it may determine changes in processing the mechanical stimuli signals created by natural movements [27, 29].
Uz et al. [64] reported that the articular branch arose from the main nerve trunk in 30 % of cases, from the posterior branch in 33 % and from the anterior branch in 16.6 %. Similarly Aszman et al. [4] described an articular branch from the anterior division of the axillary nerve . Subsequently, two more articular branches arose from the anterior branch as it crossed the inferior border of the subscapularis muscle. However Gelber et al. [27] demonstrated in the majority of cases (65.7 %) the posterior branch of the axillary nerve gave rise to the main articular branch. In 41 % it was from the branch to teres minor and the remaining cases from the initial portion of the posterior branch. Duparc et al. [22] stated that the articular branch may arise from different segments of the axillary nerve and Zhao et al. [70] showed the articular branch arising from the anterior trunk. Loukas et al. [45] reported the same branch to be arising from the anterior trunk in only 18 % of cases [2].
32.1.8 Relationship with Subdeltoid Bursa
The lower edge of the subdeltoid bursa is also considered a safe limit above the axillary nerve [6, 31], but is not a reliable landmark, due to its mobility and variant position related to the level of pressure of the arthroscopy fluid [2]. Beals et al. showed the mean minimum distance from the subdeltoid bursal reflection to the axillary nerve was 0.8 cm (0–1.4). The bursal reflection was always cephalad to the axillary nerve [6].
32.1.9 Relationship to Acromion
Ball et al. [5] looked at the relationship of the posterior branch of the axillary nerve to the posterolateral acromion. Posterior superficial dissection around the medial border of the posterior aspect of the deltoid will only endanger the superior lateral brachial cutaneous nerve when continued for an average of >80 mm. Hence the sensory branch should be at very little risk during routine exposure. Excessive lateral retraction of the deltoid during exposure of the posterior aspect of the shoulder can specifically injure the motor supply from the posterior branch of the axillary nerve to the deltoid . This branch enters the muscle at an average of only 5 cm directly inferior to the posterolateral corner of the acromion. This branch is present in 79–90 % of cases [5, 45]. Uz et al. [64] found the mean distance from the posterolateral corner of the acromion to the axillary nerve and its branches was 7.8 cm.
Traditional teaching suggests the safe zone of the axillary nerve is 5 cm from the middle of the acromiun. This is relevant in protecting the anterior branch of the axillary nerve from procedures involving a split deltoid approach, arthroscopy, intramedullary nailing and intra-muscular injections.
Several reference landmarks have been used to clarify the location of the axillary nerve . These include the acromion, greater tuberosity, bicipital groove, subdeltoid bursa and deltoid tuberosity [5, 14, 31, 38, 40, 46]. Of these landmarks the acromion is most frequently used because its border, located just below the skin and easily palpable, can be clarified most easily [12, 14, 46, 60, 65].
The acromion has some limitations as a reference landmark. First the morphological discrepancy between its angulated anterolateral and posterolateral corners and the deltoid’s round surface make the determination of a constant perpendicular point on the deltoid muscle difficult. Second, often the shape of the anterolateral and posterolateral acromial corners are bluntly, rather than acutely, angulated. Third, because the axillary nerve at the posterolateral corner is not imposed in the fascia of the deltoid , it is not stationary. Fourth, because the anterior branch of the axillary nerve runs superiorly within the muscle, the vertical distance from that branch to the anterolateral corner of the acromion can change abruptly. Fifth, the slope of the acromion is not constantly parallel to the axillary nerve ’s course [10]. It is mostly divergent, sometimes convergent and rarely parallel [60, 65].
Burkhead et al. [12] and Duparc et al. [22] reported relatively short mean distances from the acromion to the anterior branch of the axillary nerve of 5.8 cm (4.3–7.3) and 3.4 cm (3.0–4.8). Prince and Hoppenfeld et al. [33, 55] reported mean distances of 5.87 and 7.0 cm respectively. Duparc et al. [22] measured the distance of the nerve to the upper insertion of the deltoid so the height of the acromion is not included.
Sung et al. [60] showed a mean distance between the anterior axillary nerve and the acromion to be 6.5 cm. There was a strong correlation between acromial axillary nerve distance and cadaver height (r = 0.767) and humeral length (r = 0.797).
Cetik et al. [14] found the average distance of the axillary nerve from the anterior edge of the lateral acromion was 6.08 cm (5.2–6.9). The average distance of the axillary nerve from the posterior edge of the lateral acromion was 4.87 cm (4.3–5.5). The average arm length was 30.4 cm (28.1–32.9). There was a significant correlation between arm length and anterior distance (r = 0.79, p <0.001) and posterior distance (r = 0.61, p = 0.001). The ratio between arm length and distance to the nerve was expressed as an anterior and posterior index. The anterior index averaged 0.20 (0.19–0.22). The posterior index averaged 0.16 (0.15–0.17). Using these measurements a quadrangular safe zone was calculated (Figs. 32.6 and 32.7).
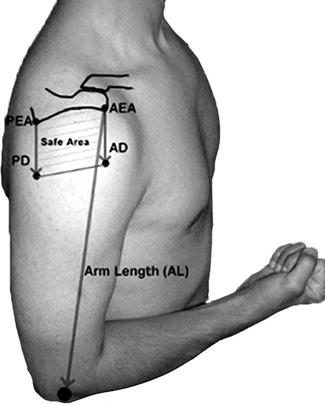
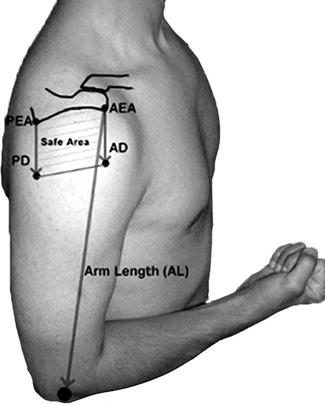
Fig. 32.6
The safe area is quadrangular in shape, with the length of the lateral edges being dependant on arm length. AD anterior distance, PD posterior distance, AEA anterior edge of acromion, PEA posterior edge of acromion (Reproduced from Cetik et al. [14])
Fig. 32.7
The deltoid muscle was replaced in its original anatomic position. The course of the nerve is shown with the needles, and the anterior distance (AD) and posterior distance (PD) were measured. AEA anterior edge of acromion, PEA posterior edge of acromion (Reproduced from Cetik et al. [14])
Kontakis [39] in a letter to the editor raised concerns over the safe zones described by Cetik et al. [14]. Kontakis et al. [40] found in 25 % of cadavers the vertical distance from the upper border of the deltoid was <4 cm. Also Burkhead et al. [12] found, in nearly one-fifth of cadavers the nerve was, 5 cm from the palpable edge of the acromion and at a minimal distance of 3.1 cm.
Stecco et al. [59] found a mean distance from axillary nerve as it enters the deltoid and the humeral head of 5 cm and to the acromion of 6.8 cm. They found when a 5 hole 114 mm PHILOS proximal humeral plate (Synthes, Stratec Medical Ltd, Mezzovico, Switzerland) is inserted with a lateral approach, in 100 % of cases the two distal holes in the plate dedicated to the humeral head coincided with the passage of the axillary nerve . Smith et al. [58] showed that the individuated three holes of the same plate, between those dedicated at the head of the humerus, could damage the integrity of the axillary nerve .
Nijs et al. [51] showed that bent nails with oblique head interlocking bolts appeared to be most dangerous in relation to the axillary nerve . The two designs featuring such a bend and oblique bolt showed a mean distance of the locking screw to the axillary nerve of 1 and 2.7 mm respectively. Sirus (Zimmer®) and (Stryker®) T2PHN (Proximal Humeral Nail).
Injury to the anterior branch of the axillary nerve has been reported with IM injections into the deltoid . Safe zones for prevention of such events have been suggested [17, 20].
There is variability in reported measurements. The measurements regarding safe zones should be used as a guide. The nerve is likely to be closer in subjects of short stature and short arm length.
32.1.10 Relationship to Capsule
Ball et al. [5] found the posterior branch of the axillary nerve to lay inferior to the capsule in the 6 o’clock position only 1 mm lateral to the glenoid rim. The nerve to teres minor and superior lateral brachial cutaneous nerve lay on the capsule at the lateral edge of the triceps origin at the level of the glenoid margin (Fig. 32.8). These nerves are at risk during arthroscopic and open surgery on the posteroinferior capsule. This may affect only the teres minor, as the deltoid is largely supplied by the anterior branch of the axillary nerve which lies lateral to the posterior branch in the quadrilateral space and courses laterally from the glenoid rim toward the neck of the humerus. The teres minor is an important dynamic stabilizer and external rotator of the humerus in an adducted position


Fig. 32.8
Anterior view of cadaveric specimens showing the axillary nerve crossing over the subscapularis to enter the quadrilateral space . The relationship to the capsule is seen (Copyright Dr Gregory Bain)
Sensory changes in the distribution of the superior lateral brachial cutaneous nerve have been noted following arthroscopic thermal shrinkage procedures on the posterior and inferior aspects of the shoulder. Similar findings have been noted following anterior dislocation of the shoulder and in association with Quadrilateral space syndrome [26, 38, 42]. Sensory changes in the distribution of the superior lateral brachial cutaneous nerve may indicate dysfunction in teres minor even if deltoid function is normal [5].
Apaydin et al. [3] found the distance from the most inferior part of the glenohumeral ligament to the axillary nerve averaged 1.1 cm (0.3–2.5 cm).
Price et al. [54] found the distance between the glenoid labrum and the axillary nerve was closest at the 6 o’clock position 12.4 mm (11.6–13.2). The nerve was 1.78 mm closer at the 6 o’clock position than 10 mm anterior or posterior to that position. The distance between the inferior glenohumeral ligament and the axillary nerve was also closest at the 6 o’clock position, 2.3 mm (1.7–2.9).
Yoo et al. [69] examined the axillary nerve from an arthroscopic perspective in a position of 30° abduction and 20° forward elevation. The axillary nerve entered the arthroscopic visual field around the 4 o’clock position (right) or 8 o’clock position (left) below the inferior margin of the subscapularis muscle. The boundaries of the nerve were the subscapularis muscle anteriorly, long head of triceps inferiorly, teres minor and major muscle posteriorly, inferior glenoid rim medially and humeral head laterally. Viewed arthroscopically the nerve was closest at the 5:30–6 o’clock position (right) or 6–6:30 o’clock position (left). The nerve had the closest distance range from 10 to 25 mm. Eleven specimens showed only the main trunk in the operative field, the remaining 12 showed the anterior and posterior branches.
Eakin et al. [24] examined the proximity of the axillary nerve to arthroscopically placed circumferential capsulolabral sutures. All sutures entered the capsule approximately 1 cm away from the glenoid and exited beneath the labrum. The shoulders were frozen in a position of 45° abduction and 20° flexion. The average distance from the axillary nerve was found to be 16.7 mm at the anterior position, 12.5 mm at the anteroinferior position, 14.4 mm at the inferior position, 24.1 mm at the posteroinferior position and 32.3 mm at the posterior position. In no specimen was a suture closer to the axillary nerve than 7 mm.
The axillary nerve can be vulnerable inferior to the glenohumeral capsule during open and arthroscopic procedures, such as capsulolabral repair, capsular plication and shift, capsular release, shoulder arthroplasty, internal fixation and historically thermal capsular shrinkage. Burkhart et al. described releasing the axillary pouch at least 5 mm lateral to the labrum during capsular release to increase the safe zone [11] (Fig. 32.9) (Video 32.4).
Fig. 32.9
The axillary nerve passes approximately 1 cm below the inferior inferior capsule. AN axillary nerve, BT biceps tendon, CP coracoid process, SM subscapularis muscle, TM teres major, Tmi teres minor (Modified with permission from Uno et al. [63])
32.1.11 Effect of Arm Position on Nerve Position
Inferior humeral translation, as in the patient with multidirectional instability reduces the distance between the axillary nerve and the anteroinferior capsule. It also draws the nerve more taut across subscapularis making it more difficult to palpate [25].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








